Diverticulitis becoming more common is a growing concern, and this post delves into the reasons behind this trend. We’ll explore the symptoms, potential causes, and how lifestyle choices might be contributing. From dietary changes to stress levels, and even genetics, we’ll uncover potential factors driving this increase in diverticulitis cases.
Understanding the rising incidence of diverticulitis is crucial for both individuals and healthcare systems. This article provides a comprehensive overview of the issue, examining the potential causes, diagnostic methods, treatment approaches, and preventative measures. We’ll also touch upon the impact on healthcare systems and the importance of early diagnosis and treatment.
Understanding the Rise in Diverticulitis

Diverticulitis, a common inflammatory condition affecting the digestive tract, has seen a concerning increase in prevalence. This rise necessitates a deeper understanding of its underlying causes, risk factors, and symptoms to effectively address this growing health concern. Many factors contribute to the escalating incidence, from dietary habits to lifestyle choices and even societal shifts.The increasing prevalence of diverticulitis underscores the importance of proactive measures to prevent its development and effectively manage existing cases.
A holistic approach combining medical advancements, lifestyle modifications, and increased public awareness is critical to combat this trend.
Symptoms of Diverticulitis
Diverticulitis is characterized by inflammation and infection of small pouches (diverticula) that protrude from the lining of the digestive tract, primarily the colon. Common symptoms include abdominal pain, often localized in the lower left quadrant, fever, nausea, vomiting, and changes in bowel habits, such as constipation or diarrhea. The severity of symptoms can vary significantly, ranging from mild discomfort to severe complications requiring hospitalization.
Understanding the spectrum of symptoms is crucial for early diagnosis and effective treatment.
Causes and Risk Factors of Diverticulitis
The exact causes of diverticulitis remain multifaceted, but a combination of factors likely plays a role. Low-fiber diets are frequently cited as a significant contributor. A diet lacking in dietary fiber can lead to harder stools, increased pressure within the colon, and a higher risk of developing diverticula. Other potential contributing factors include a sedentary lifestyle, smoking, and certain medical conditions.
Genetic predisposition also appears to be a significant risk factor, with individuals having a family history of diverticulitis more susceptible to developing the condition.
Misconceptions Surrounding Diverticulitis
Several misconceptions surround diverticulitis, often stemming from inaccurate information or lack of proper medical understanding. One common misconception is that all diverticula inevitably lead to diverticulitis. In reality, many individuals with diverticula experience no symptoms whatsoever. Another prevalent misconception is that diverticulitis is exclusively a disease of the elderly. While the risk does increase with age, diverticulitis can affect individuals of all ages, even younger adults.
Addressing these misconceptions through education and accurate medical information is essential.
Prevalence and Demographics
The prevalence of diverticulitis varies across different demographics. Studies show a higher incidence in developed countries compared to developing nations, potentially linked to dietary differences and socioeconomic factors. Age also plays a crucial role, with the risk increasing significantly in older adults. Socioeconomic factors may also influence the incidence, as access to healthcare and preventative measures can differ among various populations.
Dietary and Lifestyle Factors
Dietary habits and lifestyle choices are significant factors in the development and progression of diverticulitis. A diet low in fiber, often characterized by processed foods and insufficient fruits and vegetables, is a major contributing factor. Furthermore, a sedentary lifestyle, a lack of regular physical activity, and smoking habits all appear to increase the risk. Modifying these factors can be beneficial in preventing or managing diverticulitis.
Medical Advancements and Diagnosis
Medical advancements have significantly improved the diagnosis and treatment of diverticulitis. Diagnostic tools like CT scans and colonoscopies provide clearer images of the colon, enabling physicians to accurately identify diverticula and assess the extent of inflammation. This precise diagnostic approach allows for timely intervention and effective treatment strategies.
Potential Contributing Factors
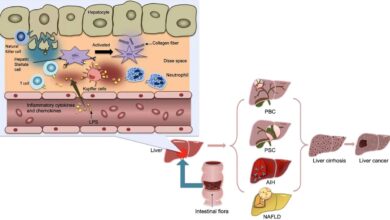
The increasing prevalence of diverticulitis, a condition characterized by inflammation of small pouches in the digestive tract, demands a multifaceted investigation into potential contributing factors. While genetics play a role, environmental influences and lifestyle choices are also significant. This exploration delves into the possible connections between dietary habits, stress, physical activity, and genetic predisposition in the growing incidence of diverticulitis.
Dietary Changes and Processed Foods
Dietary shifts, particularly the increasing consumption of processed foods, are suspected to contribute to the rise in diverticulitis cases. Processed foods, often low in fiber, can lead to a decrease in stool bulk and increased transit time through the colon. This can potentially create conditions that promote the formation of diverticula. Furthermore, these diets often contain high levels of refined sugars and unhealthy fats, which can contribute to inflammation throughout the body, a factor implicated in the development of diverticulitis.
Examples include ready-made meals, packaged snacks, and highly processed cereals, which frequently lack the fiber necessary for healthy digestion.
Stress Levels and Diverticulitis
Chronic stress has been linked to various health issues, and its potential role in the development of diverticulitis is gaining recognition. Stress can trigger physiological responses that affect the digestive system. Elevated cortisol levels, a common response to stress, can impact bowel motility and increase the risk of diverticula formation. The interplay between mental health and gut health is an active area of research, highlighting the importance of managing stress to potentially reduce the risk of diverticulitis.
It seems diverticulitis is becoming more prevalent, which is a bit concerning. While there’s no real silver bullet for this, and no permanent cure for atrial fibrillation, it highlights the ongoing need for proactive health choices to prevent these types of conditions. This increased prevalence of diverticulitis could be linked to lifestyle factors, and underscores the importance of healthy eating and regular exercise.
Sedentary Lifestyle and Diverticulitis
A sedentary lifestyle, characterized by prolonged periods of inactivity, may also contribute to the increasing prevalence of diverticulitis. Physical activity promotes healthy bowel movements and maintains optimal digestive function. Lack of exercise can lead to slower transit times, reduced stool bulk, and potential irritation of the colon, all factors that could contribute to diverticulitis. Promoting physical activity and reducing sedentary behavior is vital for overall health and potentially for mitigating the risk of diverticulitis.
Genetics and Family History
Genetic predisposition plays a significant role in the development of many diseases, including diverticulitis. Individuals with a family history of diverticulitis are at a higher risk of developing the condition. This suggests a genetic component influencing the susceptibility to diverticula formation. Further research into specific genes and their potential influence on diverticulitis development is necessary to understand this relationship fully.
It seems diverticulitis is becoming more prevalent, which is a bit concerning. While the reasons are complex, perhaps the increased focus on certain dietary habits, like the “breast is best” mantra, which some argue can be harmful, breast is best mantra harmful is contributing to the rise in cases. Ultimately, more research is needed to fully understand this trend in diverticulitis.
However, lifestyle factors still play a crucial role, even in individuals with a genetic predisposition.
Prevalence of Diverticulitis Across Regions
| Region | Prevalence (estimated) | Potential Environmental Factors |
|---|---|---|
| Developed Western Nations | High | High consumption of processed foods, lower fiber intake, higher stress levels, sedentary lifestyle |
| Developing Countries | Lower, but increasing | Shifting dietary patterns towards processed foods, increased stress levels, changing lifestyles |
| Certain Asian Regions | Lower | Traditional diets rich in fiber, potentially lower levels of stress and higher physical activity levels (variations within regions exist) |
Note: Prevalence estimates vary significantly depending on the study and the methodology used. Environmental factors can influence dietary patterns, stress levels, and physical activity.
Dietary Factors Associated with Diverticulitis
| Dietary Factor | Potential Impact on Diverticulitis |
|---|---|
| High Fiber Intake | Associated with lower risk; promotes healthy bowel movements and increased stool bulk |
| Processed Foods | Associated with higher risk; low fiber content, high refined sugars, unhealthy fats |
| Red Meat Consumption | Potentially associated with increased risk; inflammation |
| Low Fruit and Vegetable Intake | Potentially associated with increased risk; reduced fiber intake |
| Excessive Sugar Intake | Potentially associated with increased risk; inflammation |
Note: Dietary factors interact with other contributing factors, and more research is necessary to fully understand the complex relationship.
Diagnostic and Treatment Approaches
Understanding diverticulitis requires a comprehensive approach to diagnosis and treatment. Early detection and appropriate management are crucial for preventing complications and improving patient outcomes. This section explores the common diagnostic procedures, compares various treatment strategies, and highlights the evolution of medical practices in managing diverticulitis.
Common Diagnostic Procedures
Accurate diagnosis is the cornerstone of effective diverticulitis management. Several procedures are used to confirm the diagnosis and assess the extent of the condition. These methods range from simple physical examinations to more sophisticated imaging techniques.
- Physical Examination: A thorough physical examination, including assessing for abdominal tenderness, fever, and other symptoms, can provide initial clues about the presence and severity of diverticulitis. While not definitive, it helps direct further investigations.
- Blood Tests: Blood tests, such as a complete blood count (CBC) and inflammatory markers (like C-reactive protein or ESR), can help determine the presence of infection or inflammation. Elevated levels of these markers often suggest an active infection.
- Imaging Studies: Imaging plays a vital role in diagnosing diverticulitis. Computed tomography (CT) scans are the most common and effective imaging technique. CT scans provide detailed images of the abdomen, allowing visualization of the inflamed diverticula, surrounding tissue, and potential complications such as abscesses or fistulas. Ultrasound and MRI are also used in certain situations, though CT is generally preferred for its superior ability to detect subtle abnormalities and complications.
Comparison of Treatment Strategies
Treatment approaches for diverticulitis vary depending on the severity of the infection and the presence of complications. Conservative management, often the first-line approach, involves a combination of medication and dietary adjustments. Surgical intervention is reserved for cases with severe complications or those that do not respond to conservative measures.
- Conservative Management: Conservative approaches typically involve a clear liquid diet, bed rest, and administration of antibiotics to control infection. This approach aims to allow the inflammation to subside naturally. The duration of conservative management depends on the patient’s response to treatment and the severity of the diverticulitis.
- Surgical Intervention: Surgical intervention is indicated for cases with severe complications, such as abscess formation, fistulas, or perforation. Different surgical procedures exist, each with its own benefits and limitations. Laparoscopic procedures are increasingly common due to their minimally invasive nature, leading to reduced pain and faster recovery times. However, open surgery may be necessary in complex cases.
Evolution of Medical Practices
Medical practices for diverticulitis have evolved significantly over time. Early approaches often relied heavily on observation and symptomatic relief. Modern advancements in imaging and surgical techniques have improved diagnostic accuracy and treatment options, resulting in better patient outcomes.
- Historical Approaches: Historically, treatment for diverticulitis often focused on symptomatic relief and rest. The use of antibiotics was a significant advancement, allowing for better control of infections.
- Modern Approaches: The introduction of CT scans and other imaging modalities has revolutionized the diagnostic process. Minimally invasive surgical techniques have reduced the invasiveness and recovery time associated with treatment.
Significance of Early Diagnosis and Treatment
Early diagnosis and treatment of diverticulitis are crucial for preventing complications. Prompt intervention can reduce the risk of abscess formation, fistulas, bowel obstruction, and other severe outcomes.
- Prevention of Complications: Early diagnosis allows for timely intervention, reducing the risk of severe complications. A timely response can prevent the progression to more serious conditions, minimizing the impact on patient health.
- Improved Patient Outcomes: Early diagnosis and treatment significantly improve patient outcomes by limiting the extent of tissue damage and minimizing the risk of future problems.
Surgical Procedures for Diverticulitis: Pros and Cons
The choice of surgical procedure depends on the specific situation and the extent of the diverticular disease.
| Surgical Procedure | Pros | Cons |
|---|---|---|
| Laparoscopic resection | Minimally invasive, faster recovery, less pain | Not suitable for all cases, potential for complications |
| Open resection | Allows for better visualization and access, potentially better for complex cases | Longer recovery time, more pain, higher risk of complications |
| Diverticulectomy | Removal of affected diverticula | May not address underlying issues if the disease is extensive |
Effectiveness of Non-Surgical Treatments
Non-surgical treatments are often the initial approach to managing diverticulitis. The effectiveness of these treatments varies depending on the severity of the condition and the individual patient response.
- Antibiotics: Antibiotics are crucial for controlling infection. The selection of antibiotics depends on the specific bacterial infection. Effective antibiotics can drastically reduce inflammation and infection.
- Dietary Modifications: A clear liquid diet and gradual return to a normal diet, including high-fiber foods, once inflammation subsides, are essential for managing the condition and preventing future episodes. Proper dietary adjustments are crucial for long-term management.
Preventive Measures and Public Health Strategies
Diverticulitis, a condition affecting the large intestine, is increasingly prevalent. While a definitive cause remains elusive, dietary and lifestyle factors likely play a significant role. Understanding these contributing factors and implementing preventive strategies is crucial for mitigating the rising incidence. This section will Artikel personal actions and public health initiatives that can reduce the risk of diverticulitis.
Individual Preventive Measures
Dietary changes and lifestyle adjustments can dramatically reduce the risk of diverticulitis. A high-fiber diet is a cornerstone of prevention. This includes consuming plenty of fruits, vegetables, and whole grains, which promote healthy bowel movements and reduce pressure on the colon.
- Increased Fiber Intake: Gradually increasing fiber intake is vital. Sudden increases can lead to digestive discomfort. Aim for at least 25-30 grams of fiber daily. Good sources include beans, lentils, whole grains, and various fruits and vegetables.
- Hydration: Adequate hydration supports healthy bowel movements. Drink plenty of water throughout the day.
- Regular Exercise: Physical activity aids digestion and overall health, contributing to a lower risk of diverticulitis.
- Maintaining a Healthy Weight: Maintaining a healthy weight reduces stress on the digestive system.
- Reducing Processed Foods and Red Meat: Minimizing processed foods and red meat consumption is linked to a lower risk of diverticulitis. These foods are often low in fiber and can potentially contribute to inflammation.
Public Health Campaigns
Public awareness campaigns can play a crucial role in educating the public about diverticulitis and its prevention. These campaigns should emphasize the importance of healthy diets and lifestyle choices.
It seems like diverticulitis is becoming more prevalent these days, which is a bit concerning. While I’m not a doctor, I’ve been researching and I’m curious about the connection between diet and this rising prevalence. Perhaps a closer look at potential mislabeling of CBD products, like those often containing THC (check out cbd products often mislabeled some containing thc what to know ), could shed some light on the broader health picture.
Maybe there’s a hidden factor contributing to the increase in diverticulitis cases. It’s a fascinating area to explore, and I’m definitely keeping my eye on this.
- Educational Workshops and Seminars: Organizing workshops and seminars in communities can provide valuable information about the condition, its risk factors, and preventative measures.
- Community Health Fairs: Conducting health fairs in communities provides a platform for disseminating information, promoting healthy lifestyle choices, and encouraging screening.
- Partnerships with Healthcare Professionals: Collaborating with healthcare providers can increase the reach of preventive information to broader communities.
- Media Campaigns: Using social media, television, and radio to highlight the importance of preventive measures and raising awareness.
- Dietary Guidelines: Promoting dietary guidelines that encourage fiber-rich diets in public health initiatives can substantially impact the prevention of diverticulitis.
Promoting Healthy Diets and Lifestyles
Promoting healthy diets and lifestyles are essential to preventing diverticulitis. These strategies should be integrated into public health programs and community initiatives.
- School Programs: Incorporating nutrition education into school curriculums can establish healthy eating habits early in life.
- Workplace Wellness Programs: Offering wellness programs at workplaces can promote healthy diets and encourage physical activity among employees.
- Community Gardens: Promoting community gardens and initiatives can encourage access to fresh produce, enhancing dietary habits.
Increasing Awareness
Raising awareness about the increasing prevalence of diverticulitis is crucial for early detection and appropriate management.
- Public Service Announcements: Creating public service announcements (PSAs) can highlight the growing prevalence of diverticulitis and the importance of preventive measures.
- Online Resources: Creating accessible online resources with information about diverticulitis can increase awareness and provide individuals with accurate knowledge.
- Collaboration with Organizations: Collaborating with non-profit organizations focused on digestive health can expand the reach of awareness campaigns.
Recommendations for Preventing Diverticulitis
| Preventive Measure | Details |
|---|---|
| Increased Fiber Intake | Gradually increase fiber intake to 25-30 grams per day. |
| Hydration | Maintain adequate hydration by drinking plenty of water. |
| Regular Exercise | Engage in regular physical activity to support digestive health. |
| Healthy Weight Management | Maintain a healthy weight to reduce stress on the digestive system. |
| Reduced Processed Foods and Red Meat | Limit consumption of processed foods and red meat. |
Impact on Healthcare Systems
The increasing prevalence of diverticulitis presents a significant challenge to healthcare systems worldwide. Managing this condition requires substantial resources, from specialized medical personnel to advanced diagnostic tools and treatment protocols. This escalating demand places strain on existing infrastructure and necessitates careful consideration of long-term strategies for effective care.The rising incidence of diverticulitis necessitates a comprehensive understanding of its impact on healthcare systems, encompassing resource allocation, financial burdens, research needs, and comparative management across diverse healthcare settings.
This involves examining the implications for various stakeholders, from patients and clinicians to healthcare administrators and policymakers.
Resource Allocation and Strain on Systems
The growing number of diverticulitis cases puts a strain on available resources within healthcare systems. Hospitals and clinics face increased demands for beds, operating rooms, and specialized staff like gastroenterologists and surgeons. This leads to potential delays in diagnosis and treatment for other conditions, potentially impacting patient outcomes. For instance, a surge in emergency room visits for diverticulitis exacerbates existing pressure on already overloaded emergency departments, potentially impacting the timely care of patients with other critical conditions.
The strain is not limited to acute care; outpatient clinics and community health centers may also experience increased workload due to follow-up visits and management of chronic diverticulitis cases.
Financial Burden and Economic Implications
The economic impact of diverticulitis is substantial. Treatment costs encompass a range of expenses, including diagnostic procedures (CT scans, colonoscopies), medication, hospitalization, and surgical interventions. The longer a patient requires treatment, the higher the overall cost. This places a considerable financial burden on both individual patients and the healthcare system as a whole. For example, the cost of hospitalization for a diverticulitis patient can range from several thousand to tens of thousands of dollars, depending on the complexity of the case and the length of stay.
The cumulative effect of these costs on healthcare systems is significant and needs careful consideration. Increased resource allocation for diverticulitis care could potentially reduce costs associated with complications and long-term care, thereby optimizing healthcare expenditure.
Research Needs and Advancements
More research is crucial to improve our understanding of the causes and progression of diverticulitis. This includes investigating potential environmental and dietary factors that contribute to the disease’s development and exploring novel treatments and preventative strategies. For instance, ongoing research into the role of dietary fiber and gut microbiota in diverticulitis development could yield valuable insights into preventive measures.
Further investigation into the effectiveness of non-surgical treatments and the identification of biomarkers for early diagnosis could improve patient outcomes and reduce healthcare costs.
Comparative Management Across Healthcare Settings
The management of diverticulitis varies across different healthcare settings. Rural communities may experience difficulties in accessing specialized care, potentially leading to delayed diagnosis and treatment. Conversely, urban centers may face overcrowding and longer wait times for specialist consultations. This disparity highlights the need for standardized protocols and improved access to care in all healthcare settings. This may involve telemedicine initiatives to bridge geographical gaps and improve access to specialists in underserved areas.
Furthermore, robust community health programs and educational initiatives can help patients understand their condition and make informed choices about their treatment.
Economic Implications of Rising Cases
The increasing prevalence of diverticulitis leads to a significant financial burden on healthcare systems. This encompasses direct costs like hospitalization, surgery, and medication, as well as indirect costs associated with lost productivity due to patient illness and potential complications. This impact on the healthcare system is broad and requires a multifaceted approach to address the rising prevalence of this condition.
The economic implications of diverticulitis extend beyond individual patients and healthcare providers; they also impact the broader economy through lost productivity and the need for public health interventions. Strategies to reduce the burden of diverticulitis on healthcare systems should consider prevention, early diagnosis, and efficient treatment protocols.
Illustrative Examples: Diverticulitis Becoming More Common
Understanding diverticulitis requires more than just statistics; it demands a look at real-life scenarios to grasp its impact. These examples illustrate the disease’s progression, diagnostic challenges, and treatment approaches, offering a more personal and tangible understanding.
Diverticulitis Progression
A visual representation of diverticulitis progression is crucial to understanding the severity and potential complications. Imagine a small pouch (diverticulum) in the colon wall, like a tiny balloon, that becomes inflamed due to trapped fecal matter. Initially, this inflammation might be mild, causing only discomfort and mild pain. As the inflammation worsens, the pouch can become infected, leading to a more severe diverticulitis flare-up.
This can manifest as intense abdominal pain, fever, and nausea. Left untreated, the infection could spread to surrounding tissues, potentially causing a life-threatening complication like an abscess or perforation. This progression is best understood through a series of illustrations, each highlighting a stage of the process, showing the escalating inflammation and potential infection.
Patient Case Study: Sarah’s Journey
Sarah, a 45-year-old woman, experienced intermittent abdominal pain for several months. She initially attributed the discomfort to stress and poor diet. However, the pain became progressively worse, accompanied by fever and nausea. After visiting her doctor, a physical examination and blood tests revealed signs of infection. A CT scan confirmed the presence of inflamed diverticula in her sigmoid colon.
The diagnosis of diverticulitis was made. Sarah’s treatment involved a combination of antibiotics to address the infection, a clear liquid diet to allow the colon to rest, and pain management. With diligent adherence to the treatment plan, Sarah’s symptoms subsided, and she recovered completely. This case highlights the importance of seeking medical attention for persistent abdominal pain, especially if accompanied by other symptoms like fever or nausea.
Proper diagnosis and prompt treatment can prevent complications and ensure a successful recovery.
Dietary Patterns and Diverticulitis
A visual representation of two dietary patterns—one high in processed foods and low in fiber, the other rich in fruits, vegetables, and whole grains—can effectively illustrate the potential relationship to diverticulitis. The high-fiber diet promotes healthy bowel movements, which reduces the likelihood of trapped fecal matter, a primary contributing factor to diverticulitis. Conversely, a diet lacking fiber can lead to harder stools, increasing the risk of straining during bowel movements, potentially leading to inflammation and the development of diverticula.
Dietary choices are key factors in maintaining digestive health.
Anatomy of the Digestive Tract and Diverticula, Diverticulitis becoming more common
A detailed illustration of the human digestive tract is crucial for understanding diverticulitis. The illustration should highlight the location of the colon, specifically emphasizing the sigmoid colon, where diverticula are most commonly found. The diagram should clearly depict the different sections of the colon, showcasing the potential for diverticula to form along the colon’s wall. This visualization will allow a better understanding of the specific location of the issue.
Diverticulitis Flare-up
A detailed visual representation of a diverticulitis flare-up should showcase the inflammation of the diverticula. The image should depict the inflamed pouch, possibly with an abscess or a sign of infection. It should illustrate the swelling and redness of the surrounding tissues. The illustration could also include a caption that describes the characteristic symptoms of a flare-up, such as intense abdominal pain, fever, and changes in bowel habits.
Visualizing the flare-up can help patients and healthcare professionals better recognize the symptoms and the severity of the condition.
Closing Notes
The increasing prevalence of diverticulitis underscores the importance of proactive health choices. By understanding the potential contributing factors and adopting preventative measures, individuals can significantly reduce their risk. The growing need for research and improved healthcare strategies to manage this condition effectively is also highlighted. Early diagnosis and treatment are crucial to minimizing the impact on individuals and healthcare systems.
Ultimately, this information empowers readers to make informed decisions about their health and well-being.