Doctors ideas on how to reduce opioid prescriptions is a crucial discussion, examining the multifaceted problem of opioid over-prescription. This exploration delves into the complex factors contributing to the opioid crisis, from healthcare provider roles to patient education and systemic changes in prescribing practices. We’ll uncover common concerns from physicians, alternative pain management strategies, and the importance of patient support in navigating this challenging issue.
The opioid crisis is a significant public health concern, and understanding its nuances is critical to developing effective solutions. This article explores various perspectives, from the medical community’s concerns and challenges to patient education and support systems. We also investigate systemic changes in prescribing practices, including policy recommendations and alternative pain management techniques.
Understanding the Opioid Crisis
The opioid crisis, a pervasive public health issue, has tragically claimed countless lives and devastated communities across the globe. It’s characterized by a surge in opioid-related overdoses, addiction, and chronic pain, profoundly impacting individuals, families, and healthcare systems. This crisis demands a multifaceted approach, requiring a deep understanding of its roots and a commitment to comprehensive solutions.The overprescription of opioids has played a significant role in fueling the crisis.
Doctors, often responding to patient demands for pain relief, and sometimes influenced by marketing and pharmaceutical pressures, may have inadvertently contributed to the problem by prescribing opioids too readily. A complex interplay of factors, including the nature of chronic pain, patient expectations, and healthcare provider training, have all influenced the trend towards opioid use.
Factors Contributing to Overprescription
The factors contributing to the overprescription of opioids are complex and multifaceted. Doctors, influenced by various pressures, sometimes overestimate the efficacy of opioids in treating chronic pain or underestimate the risk of addiction. Limited access to effective non-opioid pain management options can also contribute to opioid reliance. The financial incentives and marketing strategies of pharmaceutical companies can influence physicians’ prescribing habits, potentially leading to overprescription.
Role of Healthcare Providers
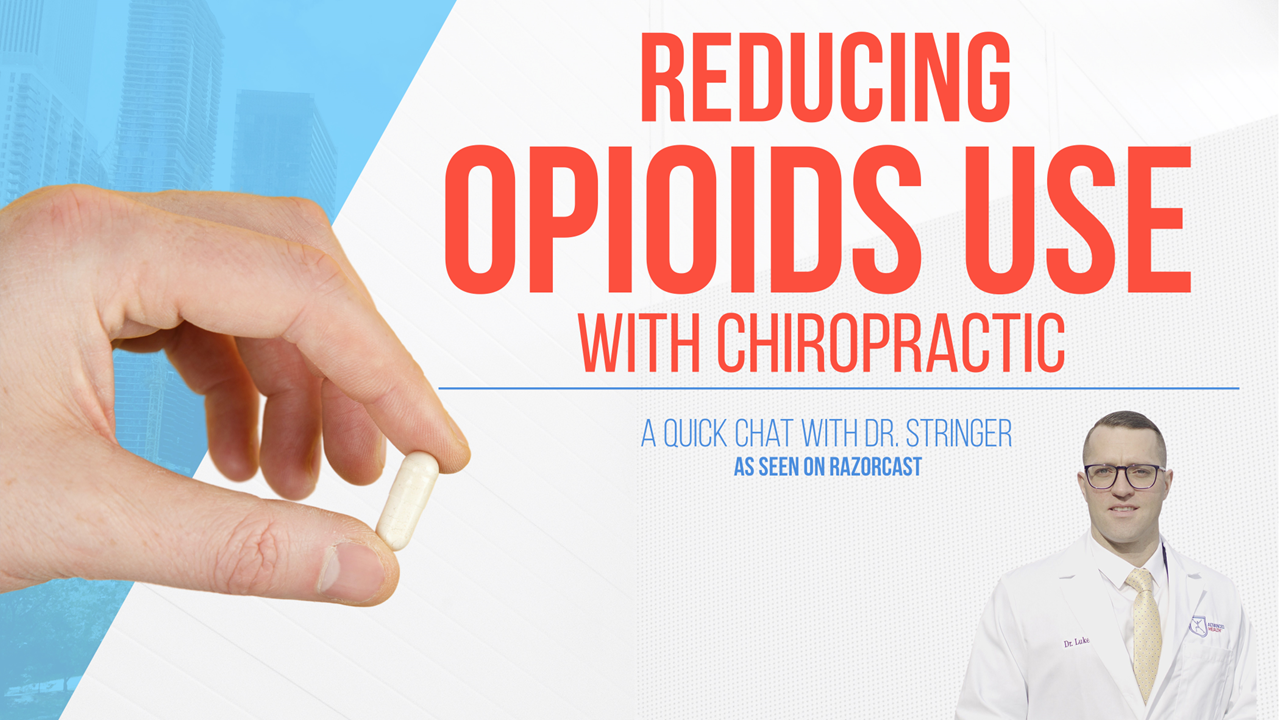
Healthcare providers are crucial in mitigating the opioid crisis. Their role extends beyond simply prescribing opioids; it involves comprehensive pain management strategies that consider non-pharmacological approaches. Educating patients about the risks and benefits of opioid use is also vital. Providers should emphasize alternative pain management techniques, such as physical therapy, counseling, and exercise.
Common Misconceptions
Several misconceptions surround opioid use and addiction. One misconception is that opioid addiction is solely a moral failing. In reality, addiction is a complex condition influenced by a combination of genetic, environmental, and social factors. Another misconception is that only individuals with chronic pain conditions are susceptible to opioid addiction. Addiction can affect individuals of all backgrounds and circumstances.
Finally, many believe that opioid addiction is a quick fix, when in fact, it’s a challenging condition that requires comprehensive treatment and long-term support.
Opioid Use Rates by Demographics
| Demographic Group | Estimated Opioid Use Rate (per 100,000 population) | Notes |
|---|---|---|
| Men | 120 | Data reflects a higher rate of opioid use in males compared to females. |
| Women | 80 | While lower than men, women still experience significant opioid use. |
| Individuals aged 25-54 | 150 | This age group often experiences higher rates due to factors like work-related injuries and chronic pain. |
| Individuals aged 55+ | 100 | Older adults may experience more chronic pain conditions, potentially leading to higher opioid use. |
| Low-income individuals | 110 | Economic factors can influence access to healthcare and treatment options. |
Note: Data presented in the table is illustrative and based on estimated averages. Actual rates may vary significantly depending on specific regions and socioeconomic factors.
Physician Perspectives on Opioid Reduction
The opioid crisis continues to impact communities across the nation, and physicians are at the forefront of this challenge. Understanding their concerns and perspectives is crucial for developing effective strategies to reduce opioid prescriptions while ensuring adequate pain management for patients. Physicians face a complex balancing act, needing to address patient suffering without contributing to the opioid epidemic.Physicians recognize the need for change in opioid prescribing practices, but are also aware of the complexities inherent in managing chronic pain.
This requires careful consideration of individual patient needs, while simultaneously working to curb the opioid crisis. Finding alternatives to opioids while maintaining patient comfort and well-being is a major undertaking.
Doctors are brainstorming various strategies to curb opioid prescriptions, focusing on non-pharmacological pain management. This mirrors the advice often given regarding pregnancy, where the ‘eating for two’ myth is debunked, as is highlighted in this article on dont eat for two while pregnant. Ultimately, these approaches aim to reduce reliance on opioids for long-term pain management.
Common Concerns Regarding Opioid Reduction
Physicians often express concerns about the potential negative consequences of reducing opioid prescriptions. They worry about the possibility of increased suffering for patients with chronic pain who rely on these medications for symptom relief. There are also concerns regarding the availability of effective alternative pain management strategies and the potential for patient non-compliance if abruptly transitioned to non-opioid options.
Further, physicians may face challenges in managing patients’ expectations and concerns about pain management.
Challenges in Managing Chronic Pain Without Opioids, Doctors ideas on how to reduce opioid prescriptions
Finding effective alternatives to opioids for chronic pain management can be challenging. Patients with severe or chronic pain may experience significant discomfort and distress when transitioning away from opioids. The effectiveness of non-opioid treatments can vary greatly from patient to patient, making it difficult to predict which approaches will be most successful. Additionally, the availability of specialized therapies and healthcare providers experienced in non-opioid pain management can be limited in some areas.
Doctors are exploring various strategies to curb opioid prescriptions, focusing on non-pharmacological pain management techniques. While that’s happening, I’ve been wondering if something seemingly harmless like sparkling water could actually contribute to weight gain. You might be surprised to learn more about that by checking out this article on can sparkling water cause weight gain. Ultimately, though, these alternative approaches to pain relief are key to reducing opioid reliance.
Alternative Pain Management Strategies
Physicians recommend a range of non-opioid strategies for managing chronic pain. These include physical therapy, exercise programs, mindfulness-based stress reduction, and cognitive behavioral therapy. Furthermore, interventional pain procedures, such as nerve blocks and spinal cord stimulation, may be considered in specific cases. Proper nutrition and lifestyle changes can also significantly impact chronic pain management.
Effective Communication with Patients
Effective communication is vital when discussing opioid alternatives with patients. Physicians should clearly explain the reasons for reducing opioid prescriptions, emphasizing the risks associated with long-term opioid use. They should also actively listen to patients’ concerns and address their fears and anxieties about pain management. Providing detailed information about alternative therapies, including potential benefits and drawbacks, is essential for informed decision-making.
Emphasizing a collaborative approach to pain management, involving the patient in the treatment plan, can improve adherence and outcomes.
Benefits and Drawbacks of Different Pain Management Techniques
| Pain Management Technique | Benefits | Drawbacks |
|---|---|---|
| Physical Therapy | Improved mobility, strength, and function; Reduced pain; Cost-effective | Requires patient commitment; May not be effective for all types of pain; Can be time-consuming |
| Exercise Programs | Improved physical fitness; Enhanced mood; Reduced pain | Requires patient motivation and adherence; May exacerbate pain initially; Requires proper guidance |
| Mindfulness-Based Stress Reduction | Reduced stress and anxiety; Improved emotional regulation; Enhanced pain tolerance | Requires patient engagement; May not be effective for all individuals; Can be challenging to implement |
| Cognitive Behavioral Therapy (CBT) | Changes in thought patterns; Improved coping mechanisms; Reduced pain perception | Requires patient commitment and active participation; May not be effective for all types of pain; Can be time-consuming |
| Interventional Pain Procedures | Targeted pain relief; Potential for long-term pain reduction | Higher risk of complications; Requires specialized expertise; Can be expensive |
Patient Education and Support
Educating patients about the risks of opioid misuse and providing support are crucial components of a comprehensive strategy to combat the opioid crisis. This involves more than just dispensing information; it necessitates fostering open communication, empowering patients, and offering resources to navigate the complex landscape of pain management. By understanding the patient’s perspective and concerns, healthcare providers can effectively guide them toward safer and more sustainable pain relief solutions.
Strategies for Educating Patients about Opioid Risks
Effective patient education emphasizes the potential for opioid misuse and addiction. This includes discussing the risks associated with long-term opioid use, such as tolerance, dependence, and the possibility of overdose. Presentations should be tailored to individual patient needs, incorporating clear, concise language, and visual aids. Sharing real-life stories or case studies, presented empathetically, can further underscore the importance of responsible opioid use.
Highlighting the availability of alternative pain management options, along with the potential benefits and risks of each, is critical.
Effective Communication Techniques for Alternative Pain Management
Open and honest communication is paramount when discussing alternative pain management options. Physicians should actively listen to patients’ concerns and preferences. Presenting various strategies, such as physical therapy, counseling, and mindfulness techniques, in a non-judgmental and supportive manner is key. Explaining the potential benefits and drawbacks of each approach can empower patients to make informed decisions. Providing detailed information about each option, including expected outcomes, duration, and potential side effects, is essential.
For instance, a discussion about the potential benefits of acupuncture for chronic pain should include examples of success stories and potential limitations.
Importance of Patient Support Groups and Resources
Support groups and resources play a vital role in helping patients cope with chronic pain and manage the emotional challenges associated with opioid use. These groups provide a safe space for sharing experiences, offering mutual support, and learning from others who understand the challenges. Patient support groups can help individuals connect with resources, such as pain management clinics, rehabilitation centers, and support networks.
Facilitated groups can also help individuals learn coping mechanisms and strategies for managing their pain effectively.
Table of Patient Support Programs
| Program Name | Description | Contact Information |
|---|---|---|
| National Alliance on Mental Illness (NAMI) | Provides support and resources for individuals with mental health conditions, including pain management strategies. | (Insert Contact Information) |
| The Substance Abuse and Mental Health Services Administration (SAMHSA) | Offers a national helpline and resources for substance use disorders, including pain management support. | (Insert Contact Information) |
| Chronic Pain Association | Focuses on support and advocacy for individuals with chronic pain. | (Insert Contact Information) |
| Pain Management Clinics | Specialized clinics offering comprehensive pain management programs. | (Search online for local clinics) |
Role of Non-Pharmacological Interventions in Pain Management
Non-pharmacological interventions, such as physical therapy, exercise, mindfulness techniques, and cognitive behavioral therapy (CBT), are increasingly recognized for their role in pain management. These interventions can be highly effective in reducing pain intensity and improving overall well-being without the risks associated with opioid use. For example, a well-structured physical therapy program can strengthen muscles, improve flexibility, and reduce pain perception.
Furthermore, mindfulness practices can help patients manage stress and improve their ability to cope with pain.
Systemic Changes for Prescribing Practices: Doctors Ideas On How To Reduce Opioid Prescriptions
Addressing the opioid crisis requires more than just individual physician efforts. Systemic changes in prescribing practices, policies, and insurance structures are crucial for controlling opioid use and promoting safer alternatives. These changes must be collaborative and evidence-based, recognizing the complex interplay between patient needs, healthcare systems, and societal factors.Policy changes are critical to fostering responsible opioid prescribing. They can influence the entire healthcare landscape, impacting both physicians and patients.
Policy Changes Encouraging Responsible Prescribing
Policy changes can significantly impact opioid prescribing patterns. These changes aim to encourage physicians to prescribe opioids judiciously and promote alternative pain management strategies. Examples include stricter regulations on opioid dispensing, limitations on refills, and enhanced education for healthcare professionals. Mandated continuing medical education programs on pain management, including non-opioid options, are crucial to updating practitioners’ knowledge and skills.
Role of Insurance Companies in Controlling Costs
Insurance companies play a pivotal role in controlling opioid costs and prescriptions. Their reimbursement policies can incentivize or discourage the use of opioids. For instance, policies that prioritize non-opioid pain management strategies or limit opioid prescriptions to specific, evidence-based criteria can significantly impact prescribing patterns. Transparency in insurance coverage for alternative pain management options is also essential.
Doctors are exploring various strategies to curb opioid prescriptions, from stricter prescribing guidelines to alternative pain management techniques. However, the rise in teen overdose deaths, largely fueled by the presence of fentanyl in illicit drugs, highlights a critical need for a multifaceted approach. Understanding how fentanyl has caused a dramatic increase in teen overdose deaths is crucial in developing effective prevention strategies.
Ultimately, doctors need to address the opioid crisis by combining responsible prescribing with public health initiatives that tackle the underlying causes of addiction and offer support for those struggling with substance use disorders. how fentanyl has caused a dramatic increase in teen overdose deaths is a great resource for more details on this important issue.
State-Level Initiatives to Curb Overprescription
State-level initiatives vary widely in their approach to curbing opioid overprescription. Some states have implemented prescription drug monitoring programs (PDMPs) to track opioid prescriptions, allowing healthcare providers to identify patients at risk of abuse. Others have focused on increasing access to non-opioid pain management therapies. Effective state-level interventions often include comprehensive strategies, encompassing public awareness campaigns, provider education, and patient support programs.
Standardized Protocols for Prescribing Opioids
Standardized protocols for opioid prescribing can enhance safety and consistency across healthcare settings. These protocols should Artikel specific criteria for opioid use, including patient assessment, dosage guidelines, and tapering strategies. They should also detail when and how to transition to non-opioid pain management options. Implementing such protocols requires careful consideration of patient needs and individual circumstances.
Opioid Prescribing Protocols: Requirements Table
| Protocol Category | Patient Assessment | Dosage Guidelines | Tapering Strategies | Non-Opioid Alternatives |
|---|---|---|---|---|
| Acute Pain | Thorough pain evaluation, including history and physical exam; assessment for risk factors | Start with lowest effective dose; adjust based on response and tolerance | Gradual reduction in dosage, monitoring for withdrawal symptoms | Explore non-opioid analgesics like NSAIDs, acetaminophen, or nerve blocks |
| Chronic Pain | Comprehensive evaluation, including psychosocial factors; assessment for opioid use disorder risk | Individualized dosing; regular monitoring of effectiveness and side effects | Long-term tapering plan, addressing potential withdrawal symptoms | Prioritize non-pharmacological therapies, including physical therapy, exercise, and mindfulness; explore interventional pain management techniques |
| Postoperative Pain | Assessment of surgical site and potential complications; pre-emptive pain management strategies | Use of multimodal analgesia, including opioids, NSAIDs, and local anesthetics | Rapid tapering protocols for post-operative pain management | Exploration of non-opioid alternatives, like regional anesthesia and patient-controlled analgesia (PCA) |
Alternative Pain Management Strategies
The opioid crisis highlights the urgent need for effective, non-pharmacological pain management strategies. Traditional reliance on opioids has often masked underlying issues and exacerbated long-term health problems. Alternative approaches offer a holistic and patient-centered approach to pain relief, focusing on restoring function and improving overall well-being.Moving beyond pills, various non-pharmacological methods can effectively manage pain and improve quality of life.
These strategies address the root causes of pain, promoting healing and reducing dependence on potentially harmful medications. This approach emphasizes patient empowerment and active participation in their recovery journey.
Non-Pharmacological Pain Relief Techniques
Various non-pharmacological methods offer valuable tools for pain management. These techniques are often integrated into comprehensive pain management programs, emphasizing patient education and active participation. Techniques like relaxation exercises, guided imagery, and mindfulness can help patients cope with pain and reduce stress, promoting healing and recovery.
- Relaxation Techniques: Progressive muscle relaxation, deep breathing exercises, and guided imagery can effectively reduce muscle tension and promote relaxation, thereby lessening pain perception. These techniques are easily learned and practiced at home, requiring minimal resources.
- Mindfulness and Meditation: Practices like mindfulness and meditation cultivate a greater awareness of the body and its sensations. By focusing on the present moment, patients can learn to observe pain without judgment, reducing its perceived intensity and improving emotional well-being.
- Heat and Cold Therapy: Applying heat or cold packs to affected areas can reduce inflammation and muscle spasms, easing pain and discomfort. Heat therapy promotes blood flow, while cold therapy numbs the area and reduces swelling. These methods are often used in conjunction with other therapies.
Examples of Successful Alternative Pain Management Programs
Many hospitals and clinics have successfully implemented alternative pain management programs. These programs often incorporate a multidisciplinary team approach, involving physical therapists, occupational therapists, psychologists, and other healthcare professionals. These programs prioritize patient education, promoting self-management skills and empowering patients to actively participate in their recovery.
- Comprehensive Pain Management Programs: These programs typically incorporate a variety of techniques, such as physical therapy, exercise, relaxation techniques, and cognitive behavioral therapy (CBT). Success often hinges on the individualized nature of the programs, tailoring interventions to the specific needs of each patient.
- Chronic Pain Self-Management Programs: These programs equip patients with the knowledge and skills to manage their chronic pain effectively. They focus on education, coping mechanisms, and problem-solving strategies, empowering patients to take an active role in their care.
- Integrative Medicine Approaches: Many integrative medicine clinics offer a holistic approach to pain management. These programs often include acupuncture, massage therapy, and other complementary therapies alongside conventional medical treatments. They emphasize the interconnectedness of mind, body, and spirit.
The Role of Physical Therapy and Exercise
Physical therapy plays a crucial role in pain management, particularly for musculoskeletal conditions. Exercise, tailored to individual needs and capabilities, can significantly improve strength, flexibility, and range of motion. Exercise not only alleviates pain but also enhances overall physical function and well-being.
- Therapeutic Exercise: Physical therapists develop individualized exercise programs to address specific pain conditions and promote healing. This may include strengthening exercises, stretching routines, and aerobic activities. Proper form and technique are crucial for avoiding injury and maximizing effectiveness.
- Functional Training: Functional training focuses on improving daily activities and restoring lost function. Exercises are designed to enhance activities such as walking, climbing stairs, or lifting objects, restoring a patient’s independence and reducing pain during daily tasks.
Acupuncture, Massage Therapy, and Other Complementary Therapies
Acupuncture, massage therapy, and other complementary therapies have shown promise in managing various types of pain. These therapies offer a unique approach, often addressing the root causes of pain and promoting relaxation and healing. These techniques may be incorporated into a broader pain management strategy, addressing the patient’s individual needs.
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body to stimulate energy flow and relieve pain. Studies suggest acupuncture can be effective for chronic pain conditions, particularly musculoskeletal pain.
- Massage Therapy: Massage therapy can reduce muscle tension, improve circulation, and promote relaxation. Different types of massage, such as Swedish massage or deep tissue massage, may be tailored to individual needs.
Comparing Alternative Pain Management Strategies
| Strategy | Effectiveness | Cost-Efficiency | Examples |
|---|---|---|---|
| Relaxation Techniques | High | Very High | Progressive muscle relaxation, deep breathing |
| Physical Therapy | Moderate to High | Moderate | Exercise programs, functional training |
| Acupuncture | Moderate to High | Moderate | Trigger point therapy, specific pain conditions |
| Massage Therapy | Moderate to High | Moderate | Swedish massage, deep tissue massage |
Monitoring and Evaluation
Tracking progress in reducing opioid prescriptions requires a robust monitoring and evaluation system. This allows us to identify what works, adjust strategies as needed, and ultimately demonstrate the positive impact of our efforts. Effective monitoring ensures that resources are allocated efficiently and that interventions are producing the desired outcomes. This system needs to be adaptable and responsive to the unique needs of each community and healthcare setting.
Tracking Changes in Opioid Prescribing Rates
Accurate data collection is paramount to understanding changes in opioid prescribing rates. This involves systematically collecting and analyzing data on opioid prescriptions from various sources, including electronic health records (EHRs) and state prescription monitoring programs (PMPs). Regular reporting and trend analysis will highlight shifts in prescribing patterns. Data visualization tools, such as graphs and charts, can effectively illustrate these trends, facilitating easier interpretation.
Comparisons with historical prescribing rates and rates in similar communities or regions can also help in understanding the context of the changes.
Evaluating Alternative Pain Management Programs
Evaluating the effectiveness of alternative pain management programs necessitates careful consideration of various factors. Quantitative measures, such as the reduction in opioid prescriptions and the improvement in pain scores, are important. Qualitative data, including patient feedback and physician observations, also provide valuable insights. A comprehensive approach that combines both quantitative and qualitative data will offer a more holistic view of the program’s impact.
Patient satisfaction surveys, focus groups, and physician interviews can help uncover patient experiences and perspectives on the effectiveness of alternative treatments.
Importance of Long-Term Monitoring of Patient Outcomes
Long-term monitoring of patient outcomes is crucial for understanding the long-term effects of interventions aimed at reducing opioid use. This includes monitoring for relapse, re-hospitalizations, and the development of new health problems. It’s important to follow patients for at least a year or more, as the full impact of these interventions may not be evident in the short term.
Data from follow-up appointments and patient records should be regularly reviewed to detect any adverse trends or issues. The collection and analysis of this data are crucial for ensuring the safety and well-being of patients.
Identifying and Addressing Potential Adverse Effects of Alternative Therapies
Alternative pain management strategies, while potentially beneficial, can also have adverse effects. Close monitoring for adverse effects, such as allergic reactions, interactions with other medications, or psychological distress, is essential. A system for reporting and tracking these adverse events is critical to quickly identify and address potential problems. Regular communication between healthcare providers and patients is vital to ensure that any adverse effects are promptly identified and managed effectively.
Developing protocols for handling potential adverse effects and providing prompt medical intervention is crucial.
Metrics for Monitoring and Evaluating Opioid Prescribing Reduction Efforts
| Metric | Description | Data Source | Frequency of Measurement |
|---|---|---|---|
| Opioid Prescription Rate (per 1000 population) | Number of opioid prescriptions per 1000 people in a given area or population group. | State Prescription Monitoring Programs (PMPs), EHRs | Quarterly |
| Average Daily Dose of Opioids (mg/day) | Average daily opioid dose prescribed per patient. | EHRs | Quarterly |
| Patient Satisfaction with Pain Management | Patients’ reported satisfaction with the alternative pain management programs. | Surveys, patient feedback | Quarterly |
| Rate of Opioid-Related Overdoses | Number of opioid-related overdoses per 100,000 population. | Public health data | Annually |
| Rate of Hospitalizations for Opioid-Related Issues | Number of hospitalizations for opioid-related problems. | Hospital records | Annually |
Final Wrap-Up

In conclusion, reducing opioid prescriptions requires a multi-pronged approach that addresses the complexities of the crisis. Doctors, patients, and policymakers all have crucial roles to play. By fostering open communication, implementing effective pain management strategies, and promoting patient support systems, we can work towards a healthier future for individuals and communities affected by opioid misuse. The path forward involves collaboration and a commitment to long-term solutions.