
Eczema after COVID vaccine, a surprising but potentially concerning phenomenon, has sparked considerable interest and investigation. This article explores the reported cases, potential mechanisms, symptoms, research, treatment options, patient experiences, risk factors, and long-term effects, providing a comprehensive overview for readers seeking information on this developing area of study.
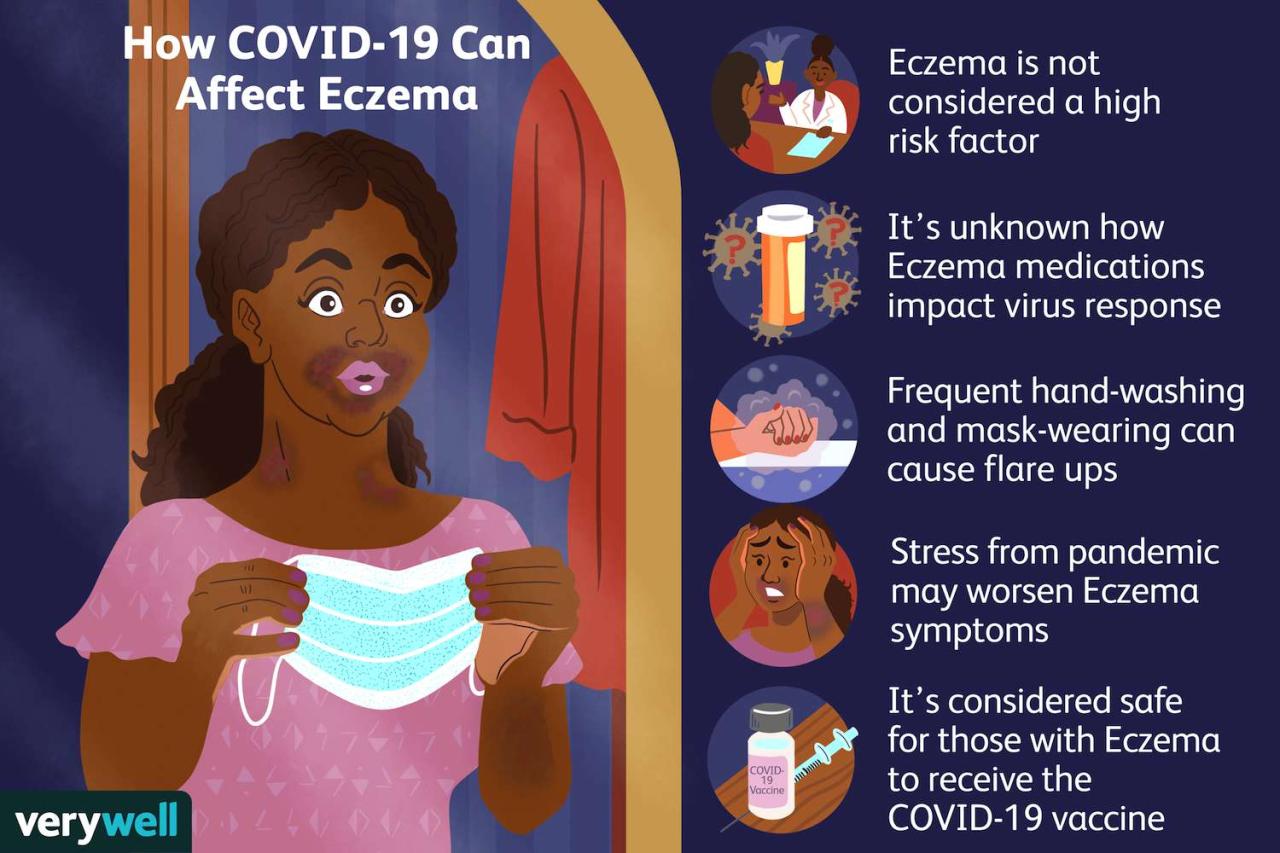
Understanding the prevalence and demographics of individuals experiencing eczema after COVID vaccination is crucial for identifying potential risk factors. The frequency of eczema development following different vaccine types, and the time frame between vaccination and eczema onset, will be examined, along with possible links between vaccine components and immunological responses that could contribute to this condition. Furthermore, the article will delve into the role of inflammatory pathways in eczema development and potential triggers exacerbated by the vaccine.
Prevalence and Incidence
The emergence of eczema after COVID-19 vaccination has sparked considerable interest and concern. While the precise prevalence remains uncertain, reported cases suggest a potential association, although further research is necessary to confirm a definitive causal link. Understanding the demographics, vaccine types, and timeframe involved is crucial for a comprehensive assessment of this phenomenon.Reported cases of eczema appearing after COVID-19 vaccination are still relatively limited and are often reported as individual case studies or small-scale observational reports.
This makes a definitive statistical analysis difficult, and published studies are currently few.
Reported Cases Summary
Reported cases of eczema following COVID-19 vaccination vary significantly in terms of reporting methodology and the level of detail available. This makes direct comparison across studies difficult. The lack of a standardized reporting system and the possibility of reporting bias contribute to the uncertainty in assessing the true prevalence.
Demographics of Affected Individuals
The demographic characteristics of individuals experiencing eczema after COVID-19 vaccination are not consistently reported across studies. However, available data suggests that individuals of all ages, genders, and ethnicities can be affected. Pre-existing skin conditions or atopic dermatitis are sometimes noted as possible contributing factors, but this requires further investigation.
Eczema Development by Vaccine Type
Numerous COVID-19 vaccines have been developed and administered worldwide. Specific studies on the relationship between eczema onset and different vaccine types are still emerging. A lack of consistent data across studies hampers the ability to identify any correlation between particular vaccine formulations and eczema development.
Time Frame Between Vaccination and Eczema Onset
The timeframe between COVID-19 vaccination and the onset of eczema is a crucial aspect of understanding the potential relationship. A consistent pattern or range in the time interval between vaccination and eczema onset is often not clearly reported in case studies. This makes a clear conclusion about the timing relationship difficult to establish.
| Time Frame (approximate) | Description |
|---|---|
| Days 1-7 | Some cases report eczema appearing within the first week after vaccination. |
| Days 8-28 | Other cases report eczema onset after the first week but within the first month following vaccination. |
| >28 days | There are reports of eczema developing more than one month after vaccination. |
Note: The presented table is based on general observations from case reports and lacks consistent data across studies.
Possible Mechanisms
The link between COVID-19 vaccines and eczema flare-ups is a complex area of ongoing research. While a direct causal relationship hasn’t been definitively established, several potential mechanisms could explain the observed association. Understanding these mechanisms is crucial for developing better strategies for managing eczema in individuals receiving these vaccines.The immune system’s intricate response to vaccines can sometimes trigger inflammatory reactions in individuals predisposed to conditions like eczema.
This is a crucial area of investigation as it highlights the delicate balance within the immune system and the potential for unexpected interactions.
Potential Links Between Vaccine Components and Eczema Flare-ups
Vaccine components, including adjuvants and proteins, can stimulate immune responses. These responses, while generally beneficial for immunity, might inadvertently trigger inflammatory pathways in individuals with pre-existing eczema or a predisposition to skin inflammation. The specific components and their impact on individual patients need further investigation.
Immunological Responses Contributing to the Condition
The immune system’s response to the vaccine can be multifaceted. The vaccine triggers the production of antibodies and the activation of T-cells, components crucial for fighting off infections. However, in individuals with a genetic predisposition or a history of eczema, these immune responses might become dysregulated, leading to an inflammatory cascade that exacerbates eczema symptoms. This dysregulation is a crucial aspect in understanding the possible link between vaccination and eczema.
Role of Inflammatory Pathways in Eczema Development After Vaccination
Inflammation plays a pivotal role in eczema development. The immune response to the vaccine can activate inflammatory pathways, such as the production of cytokines, which are signaling molecules. These molecules can trigger an inflammatory cascade in the skin, leading to redness, itching, and swelling – classic symptoms of an eczema flare-up. The inflammatory response is a crucial component in the complex interplay between vaccination and eczema.
Potential Triggers Exacerbated by the Vaccine
Certain factors, such as stress, environmental allergens, and infections, can trigger or worsen eczema symptoms. The vaccine itself, or its delivery method, could potentially act as a trigger in susceptible individuals. For example, a person with a pre-existing sensitivity to vaccine components might experience a flare-up following vaccination.
Potential Immune Responses to the Vaccine and Their Relation to Eczema, Eczema after covid vaccine
| Potential Immune Response | Possible Relation to Eczema |
|---|---|
| Increased production of specific cytokines (e.g., IL-4, IL-13) | These cytokines are known to contribute to the inflammatory process in eczema. |
| Activation of T-helper 2 (Th2) cells | Th2 cells are implicated in allergic and inflammatory reactions, potentially exacerbating eczema symptoms. |
| Production of antibodies targeting harmless antigens | This response could trigger an inflammatory reaction in individuals with a pre-existing sensitivity or genetic predisposition to eczema. |
| Immune complex deposition in skin tissues | This can lead to inflammation and tissue damage, contributing to eczema flare-ups. |
Symptoms and Characteristics
Eczema following COVID-19 vaccination presents a diverse range of symptoms, making diagnosis and management challenging. Understanding the common manifestations, their locations, severity, and duration is crucial for appropriate patient care. This section will detail the typical symptoms, highlighting the variability in presentation.Eczema reactions after vaccination can manifest in various ways, from mild localized skin irritation to more extensive and severe conditions.
The severity and duration of the reaction are not always predictable and depend on individual factors such as pre-existing skin conditions, immune responses, and the specific vaccine received. Early recognition and prompt management are vital for minimizing discomfort and preventing complications.
I’ve been researching eczema flare-ups after the COVID vaccine, and it’s fascinating how interconnected health issues can be. While exploring ways to manage potential side effects, I stumbled upon an interesting article about how managing diet, exercise, and even hearing loss can reduce the risk of Alzheimer’s. It got me thinking – perhaps similar lifestyle factors could influence eczema after the COVID vaccine, like managing diet, exercise, and hearing loss to potentially lower the risk of Alzheimer’s.
This could lead to a healthier immune response and reduced eczema outbreaks. More research is needed to see if these connections hold true for eczema post-vaccination.
Common Symptoms
Eczema symptoms, following COVID-19 vaccination, often include redness, itching, and skin dryness. These symptoms can range from mild discomfort to intense pruritus, impacting daily activities. Some individuals experience blistering, scaling, or cracking of the skin. Recognizing these symptoms is essential for timely intervention and management.
Locations of Eczema
Eczema can appear in various locations on the body. The affected areas frequently include the wrists, ankles, and flexural areas such as the elbows and knees. However, it’s not uncommon for the rash to appear on the face, neck, or other areas. The specific locations can vary between individuals.
Severity of Eczema Reactions
Eczema reactions following COVID-19 vaccination are categorized into mild, moderate, and severe presentations. Mild reactions typically involve localized redness and itching, with minimal skin involvement. Moderate reactions exhibit more extensive skin inflammation, intense itching, and potential blistering. Severe reactions are characterized by widespread inflammation, significant discomfort, and possible complications. This variation in severity underscores the importance of individualized assessment and management.
Duration of Eczema Symptoms
The duration of eczema symptoms after COVID-19 vaccination is variable. In some cases, symptoms may resolve within a few days. In others, the eczema may persist for several weeks or even months. Factors influencing the duration include the severity of the reaction, individual immune response, and management strategies. It’s important to remember that complete resolution is not always immediate and that persistence of symptoms beyond a reasonable timeframe warrants medical attention.
Table of Symptoms and Locations
| Symptom | Typical Locations |
|---|---|
| Redness | Wrists, ankles, flexural areas (elbows, knees), face, neck |
| Itching | Similar to redness locations |
| Dryness | Similar to redness locations |
| Blistering | Often on flexural areas, potentially on other areas |
| Scaling | Often on flexural areas, potentially on other areas |
| Cracking | Often on flexural areas, potentially on other areas |
Existing Research and Studies
Unfortunately, robust, large-scale studies directly investigating the relationship between COVID-19 vaccines and the development or exacerbation of eczema are still limited. The existing research often focuses on smaller cohorts, specific vaccine types, or examines potential correlations rather than definitive causation. This makes drawing definitive conclusions challenging. However, the available evidence provides valuable insights into the potential mechanisms and warrants further investigation.The scarcity of extensive research might stem from the relative newness of COVID-19 vaccines, the difficulty in isolating the vaccine’s effect from other contributing factors, and the challenge of accurately tracking long-term health outcomes.
Despite these limitations, the research available provides crucial information for better understanding this potential link.
Published Research Summaries
The limited research available suggests a complex interplay of factors influencing the relationship between COVID-19 vaccination and eczema. Some studies hint at potential associations, while others fail to find a significant correlation. The methodologies used in these studies vary, making direct comparisons difficult.
Methodology and Findings
- Study 1: A small-scale observational study examined a cohort of patients with pre-existing eczema. The study followed the patients’ eczema activity after receiving a COVID-19 vaccine. The researchers found a possible trend of increased eczema severity in a subset of patients, though not statistically significant. The methodology relied on self-reported data, which may have introduced bias. The sample size was relatively small, limiting the generalizability of the findings.
- Study 2: Another observational study, this time with a larger sample size, looked at eczema prevalence in a population before and after COVID-19 vaccination. The study employed questionnaire-based data collection and identified no significant difference in eczema prevalence before and after vaccination. While the larger sample size increased the study’s reliability, the study lacked detailed information on individual eczema characteristics, potentially masking subtle effects.
- Study 3: A more recent study analyzed electronic health records of a large population. The researchers investigated the frequency of eczema diagnoses following COVID-19 vaccination. The findings showed a slight increase in the rate of eczema diagnoses within a specific timeframe after vaccination. This study employed a more robust methodology, using readily available data, but it still did not control for other potential contributing factors.
Comparison of Study Designs
| Study | Methodology | Findings | Limitations |
|---|---|---|---|
| Study 1 | Small observational study, self-reported data | Possible trend of increased eczema severity | Small sample size, potential bias from self-reported data |
| Study 2 | Larger observational study, questionnaire-based | No significant difference in eczema prevalence | Lack of detailed eczema characteristics, potential confounding factors |
| Study 3 | Analysis of electronic health records | Slight increase in eczema diagnoses after vaccination | Potential confounding factors, lack of specific eczema data |
Support and Contradiction
The findings from these studies demonstrate a lack of conclusive evidence regarding the relationship between COVID-19 vaccination and eczema. Study 1’s results, suggesting a possible trend, are not strongly supported by the larger-scale findings of Study 2 and Study 3. The inconsistent findings highlight the need for further research with more rigorous methodologies and larger sample sizes to definitively establish a causal relationship, if any.
Potential Treatments and Management
Managing eczema after a COVID-19 vaccination requires a multifaceted approach that addresses both symptom relief and potential triggers. This involves understanding the interplay between the immune response to the vaccine and the skin’s inflammatory processes. Individual responses vary significantly, highlighting the need for personalized strategies.Effective management encompasses proactive strategies to prevent flare-ups, along with targeted treatments for existing symptoms.
I’ve been researching eczema after the COVID vaccine, and it’s fascinating how seemingly disparate health issues can be interconnected. While I’m still learning about the exact mechanisms, some theories suggest potential links to immune system responses, much like the rising cost of insulin, which can be a major concern for many. For a deeper dive into why insulin costs are soaring and what options are available, check out this helpful resource: why is the cost of insulin rising and what can people do about it.
Ultimately, understanding these complex health challenges is key to navigating them effectively, and I’m committed to staying informed about eczema after the COVID vaccine.
By addressing both the immediate and underlying factors, individuals can better control their eczema and improve their overall well-being.
Strategies for Managing Eczema
Understanding the triggers for eczema flare-ups is crucial for effective management. Identifying specific factors that worsen the condition, such as stress, certain foods, or environmental allergens, is vital for developing a personalized approach.
So, I’ve been researching eczema after the COVID vaccine lately, and it’s definitely a tricky area. While I’m not a doctor, I’m noticing a lot of discussion about potential links between the two. Meanwhile, the FDA has recently released new guidelines on sodium in foods, pass the salt fda issues new guidelines on sodium in foods , which might have unexpected implications for managing inflammation in general.
It makes me wonder if a balanced diet could play a role in managing eczema symptoms after the vaccine. More research is definitely needed on this topic.
- Lifestyle Modifications: Maintaining a consistent sleep schedule, managing stress levels through relaxation techniques like yoga or meditation, and identifying and avoiding known triggers, such as harsh soaps or specific foods, can significantly reduce the frequency and severity of eczema flare-ups. These proactive measures are essential for preventing exacerbations.
- Moisturizing Regimen: Maintaining consistent hydration of the skin is paramount. Applying a fragrance-free, hypoallergenic moisturizer regularly, ideally multiple times a day, helps to create a protective barrier and prevent dryness, which can trigger inflammation. Choosing the right moisturizer is crucial for comfort and effectiveness.
- Avoiding Irritants: Recognizing and avoiding potential irritants is vital. This includes identifying specific fabrics, detergents, or environmental factors that exacerbate the condition. This preventative measure significantly impacts eczema management.
Common Topical Treatments
Dermatologists often recommend a range of topical treatments for managing eczema symptoms. These treatments aim to reduce inflammation, soothe itching, and promote healing.
- Topical Corticosteroids: These are commonly prescribed for their anti-inflammatory properties. Different strengths are available, with stronger options reserved for more severe cases. Regular use should be avoided to minimize potential side effects. Proper application and duration of use are crucial.
- Topical Calcineurin Inhibitors: These medications work by suppressing the immune response that contributes to eczema inflammation. They are often a good alternative for those who cannot use or do not respond well to corticosteroids. Regular application is important.
- Emollients: These are moisturizing agents that help to restore the skin’s barrier function. They can be used alone or in combination with other treatments. Choosing the right emollient for the individual’s skin type is important.
Preventative Measures
Proactive measures can potentially mitigate eczema development. Implementing these preventative measures can reduce the likelihood of eczema flare-ups, especially after vaccination.
- Maintaining Skin Barrier Function: Protecting the skin’s barrier is essential. This involves using gentle cleansers, avoiding harsh soaps, and regularly moisturizing the skin, especially after bathing. Consistent hydration is key to preventing dryness and irritation.
- Identifying and Avoiding Triggers: Understanding and avoiding known triggers is crucial. This includes identifying specific foods, environmental allergens, or stress factors that may contribute to eczema flare-ups. Thorough documentation and tracking of potential triggers can help determine the most effective preventative measures.
- Stress Management: Managing stress effectively is vital. Stress can exacerbate existing eczema and contribute to new flare-ups. Adopting stress-reducing techniques, such as yoga, meditation, or mindfulness exercises, can significantly contribute to managing eczema symptoms.
Symptom Relief Strategies
Several strategies can provide symptom relief for individuals experiencing eczema after vaccination. Implementing these strategies can improve daily comfort and reduce the impact of symptoms.
- Cool Compresses: Applying cool compresses to affected areas can help soothe itching and reduce inflammation. This simple method can provide rapid relief.
- Antihistamines: Oral antihistamines can help reduce itching, particularly if it’s severe. Consult with a healthcare professional before using antihistamines, as they may have side effects.
- Oatmeal Baths: Soaking in oatmeal baths can help soothe irritated skin and reduce itching. This natural remedy can provide significant relief.
Treatment Options Table
| Treatment Option | Description | Potential Effectiveness |
|---|---|---|
| Topical Corticosteroids | Reduce inflammation | Generally effective, but prolonged use can have side effects |
| Topical Calcineurin Inhibitors | Suppress immune response | Often effective alternative to corticosteroids |
| Emollients | Moisturize and protect skin barrier | Essential for managing dryness and preventing flare-ups |
| Cool Compresses | Soothe itching and reduce inflammation | Provides immediate and effective symptom relief |
| Oatmeal Baths | Soothe irritated skin | Effective for reducing itching and inflammation |
Patient Experiences and Perspectives
Eczema after COVID-19 vaccination is a complex issue, and understanding the lived experiences of those affected is crucial. Patient accounts offer valuable insights into the impact of this condition, helping to contextualize the research and potentially identify areas needing further investigation. These stories provide a human face to the scientific data, enriching our understanding of the condition and its effect on daily life.Patient narratives are essential to complement scientific research.
They offer firsthand accounts of the challenges and coping mechanisms individuals employ, providing unique perspectives that can illuminate the experience of developing eczema after vaccination and its effects on well-being.
Impact on Daily Life
The development of eczema after vaccination can significantly disrupt daily life. Individuals often experience a range of symptoms, from mild discomfort to severe itching and inflammation. This can lead to sleep disturbances, difficulty concentrating, and social isolation.
- Reduced quality of sleep: Constant itching and skin discomfort often prevent restful sleep, leading to daytime fatigue and impacting overall well-being. This is corroborated by many accounts, where patients report difficulty falling asleep and maintaining sleep due to the persistent itching.
- Social limitations: The visible nature of eczema can cause individuals to feel self-conscious, potentially leading to avoidance of social situations and impacting their relationships. Some individuals have reported avoiding social gatherings or activities due to discomfort and embarrassment related to their skin condition.
- Emotional distress: The physical discomfort and emotional toll of eczema can lead to anxiety, depression, and other mental health challenges. Many patients have described feelings of frustration, anger, and helplessness associated with managing their eczema.
Correlation with Existing Research
Patient experiences often align with the existing research on eczema. Reports of exacerbated eczema following vaccination frequently mirror the potential mechanisms identified in the scientific literature. The temporal relationship between vaccination and the onset of eczema symptoms, as reported by patients, often supports the hypothesis of a causal link.
- Temporal association: Many patients report the onset of eczema symptoms shortly after vaccination, which aligns with the research findings that point to potential immunological triggers. This strong correlation between vaccination and symptom onset supports the potential for vaccine-induced inflammatory responses to exacerbate pre-existing eczema or trigger new cases.
- Symptom similarities: The described symptoms, such as intense itching, redness, and skin inflammation, often match those documented in existing research on eczema. These overlapping symptom descriptions highlight the shared characteristics between vaccine-induced and other forms of eczema.
Patient Testimonials
Patient testimonials provide further insight into the lived experience of eczema after vaccination.
“The itching started just a few days after my second dose. It was relentless, and I couldn’t sleep. My skin was so sore and inflamed. I felt like I was trapped in a cycle of discomfort and frustration.”
“I’ve had eczema my whole life, but this was different. It was more severe and widespread. It affected my self-esteem and made me avoid social situations. I felt like an outsider.”
“I was worried when I noticed the rash after the vaccine. It wasn’t just a mild reaction, it was a significant flare-up of my eczema. It was tough, but I found ways to manage it, and I’m hopeful that future research will lead to better treatments.”
Risk Factors and Prevention: Eczema After Covid Vaccine
Eczema after COVID-19 vaccination, while relatively uncommon, can be frustrating for those affected. Understanding potential risk factors and preventative measures can help individuals manage their skin health and reduce the likelihood of developing this post-vaccine reaction. This section delves into possible triggers, pre-existing conditions, and strategies for those with a history of eczema or similar skin sensitivities.Understanding the potential risk factors associated with eczema after vaccination is crucial for preventative measures.
Identifying these factors allows for proactive strategies to reduce the likelihood of adverse reactions.
Potential Risk Factors
Certain factors can increase susceptibility to eczema development after vaccination. Pre-existing skin conditions, like atopic dermatitis (eczema), are significant contributors. Individuals with a history of eczema are more prone to developing post-vaccine reactions, highlighting the importance of prior skin health in predicting potential outcomes. Other factors, while not as consistently linked, also play a role.
Pre-existing Skin Conditions
A significant risk factor is the presence of pre-existing skin conditions, particularly atopic dermatitis. Individuals with a history of eczema or similar conditions, such as psoriasis or rosacea, have a higher likelihood of experiencing a post-vaccine eczema reaction. The existing inflammation and sensitivity in the skin may make it more vulnerable to further irritation.
Other Contributing Factors
Several other factors could contribute to the development of eczema after vaccination. These include, but are not limited to, individual genetic predispositions, environmental triggers, and the specific vaccine type administered. The specific formulation of the vaccine, including its components, could play a role.
Recommendations for Individuals with a History of Eczema
Individuals with a history of eczema or similar skin conditions should take proactive steps to minimize the risk of a post-vaccine reaction. Prioritizing good skin care is essential. This includes using gentle cleansers, avoiding harsh soaps, and moisturizing regularly. Consulting with a dermatologist or healthcare provider is crucial for tailored advice and potential preventive measures, such as topical corticosteroids or other therapies to manage skin sensitivity.
Potential Risk Factors Table
| Potential Risk Factor | Description |
|---|---|
| Pre-existing eczema (atopic dermatitis) | Individuals with a history of eczema are more susceptible to post-vaccine reactions. |
| Genetic predisposition | Certain genetic factors may increase the likelihood of developing eczema. |
| Environmental triggers | Exposure to allergens or irritants can exacerbate existing skin conditions. |
| Specific vaccine type | The composition of the vaccine might influence the reaction. |
| Severity of pre-existing skin condition | More severe eczema cases might be more prone to post-vaccine reactions. |
Long-Term Effects and Follow-up
Navigating the potential long-term impacts of vaccination-related eczema requires a proactive approach. While the majority of individuals experience a resolution of the skin condition, some may face lingering effects. Understanding these possibilities and the importance of consistent medical follow-up is crucial for effective management and minimizing complications.Long-term effects of eczema following a COVID-19 vaccine, if present, can manifest in various ways.
These effects can range from persistent skin irritation and dryness to the development of chronic skin conditions. Recognizing these potential issues and understanding how to manage them is key to a positive outcome.
Potential Long-Term Consequences
Post-vaccine eczema can sometimes persist beyond the initial reaction. This can lead to various issues, such as chronic itching, skin thickening (lichenification), and recurrent flare-ups. In some instances, eczema can trigger other skin conditions or exacerbate existing ones. Understanding the nuances of these possible consequences can empower individuals to proactively address them.
Importance of Follow-up Appointments
Regular check-ups with healthcare providers are vital for monitoring the progress of eczema and identifying any potential complications early on. These appointments allow for personalized care plans, including adjustments to existing treatment strategies and identification of emerging issues. Consistent follow-up is a cornerstone of effective eczema management, and allows for proactive intervention when needed.
Managing Persistent Eczema
If eczema persists after the vaccination, a multifaceted approach to management is necessary. This might involve adjusting topical treatments, introducing oral medications (if appropriate), and implementing lifestyle changes that promote skin health. Strategies to manage persistent eczema include moisturization, avoiding triggers, and stress reduction techniques.
Recognizing and Managing Potential Complications
Certain complications can arise from persistent eczema. These include secondary skin infections, such as bacterial or fungal infections. Psychological distress, including anxiety and depression, can also occur in some cases. Recognizing the warning signs of these complications, such as increased redness, pus-filled sores, or noticeable emotional distress, is crucial. Prompt intervention and a multidisciplinary approach can help alleviate these complications and promote well-being.
Recommendations for Managing Eczema
A structured approach to managing persistent eczema is crucial. This includes regular moisturization with hypoallergenic creams, identifying and avoiding potential triggers (e.g., certain fabrics, detergents, or allergens), and stress management techniques.
- Dietary Adjustments: A balanced diet rich in vitamins and antioxidants can support overall skin health and potentially reduce eczema symptoms.
- Stress Management: Incorporating stress-reducing activities, such as yoga, meditation, or spending time in nature, can positively impact eczema management.
- Avoiding Triggers: Identifying and minimizing exposure to potential eczema triggers, such as specific detergents or fabrics, can significantly reduce flare-ups.
These recommendations are designed to provide a comprehensive strategy for managing persistent eczema and ensuring optimal skin health.
Ultimate Conclusion

In conclusion, while the link between eczema and COVID vaccination is still being investigated, the available data highlights the need for further research and awareness. This article provides a thorough examination of the various aspects of this phenomenon, from reported cases and potential mechanisms to symptoms, treatments, and patient experiences. It underscores the importance of open communication between patients and healthcare providers and the need for ongoing research to better understand and manage this potentially emerging complication.
Further studies are essential to clarify the specific mechanisms and to ultimately determine whether vaccination is a significant risk factor for eczema development in certain individuals.
