Ending the hiv aids epidemic – Ending the HIV/AIDS epidemic is a monumental global challenge, demanding comprehensive strategies and unwavering commitment. This exploration dives deep into the historical context, current state, and crucial strategies needed to achieve this ambitious goal. From prevention and treatment to addressing specific vulnerable populations, we’ll examine the multifaceted nature of this public health crisis and the path forward.
The epidemic’s impact spans generations and geographies, leaving an indelible mark on communities worldwide. Understanding the complexities of this issue, including its historical roots, present-day challenges, and diverse affected populations, is paramount to developing effective and sustainable solutions.
Defining the HIV/AIDS Epidemic
The HIV/AIDS epidemic, a global health crisis, continues to demand our attention and resources. Understanding its evolution, current state, and key indicators is crucial to guiding effective interventions and achieving a future free from its devastating impact. This understanding provides a foundation for strategizing and allocating resources to address the epidemic’s ongoing challenges.The epidemic, while initially perceived as a relatively contained issue, quickly evolved into a global concern impacting communities across the world.
Early responses, while well-intentioned, were often hampered by limited knowledge and societal stigma. These factors contributed to a delayed and uneven response to the crisis.
Historical Context of the Epidemic
The HIV/AIDS epidemic emerged in the 1980s, initially recognized as a cluster of unusual cases of pneumonia and Kaposi’s sarcoma in gay men in the United States. This initial identification sparked a global response, but understanding the virus and its transmission took time. Critical milestones included the identification of the virus (HIV) in 1983, the development of the first antiretroviral therapies (ARVs) in the 1990s, and the growing recognition of the epidemic’s impact on marginalized communities.
Ending the HIV/AIDS epidemic is a crucial global goal, and access to affordable healthcare plays a massive role. Fixing issues with Obamacare, like those highlighted in this article about what needs to be fixed in obamacare , could significantly improve healthcare access and make a real difference in combating the spread of HIV. Ultimately, a robust and equitable healthcare system is key to ending this epidemic once and for all.
These developments, however, were not without challenges. Stigma, discrimination, and limited access to treatment in many parts of the world hindered efforts to control the epidemic’s spread.
Current State of the Epidemic
The current state of the HIV/AIDS epidemic shows a complex picture. Prevalence rates vary significantly across different regions and populations. While progress has been made in reducing new infections and improving access to treatment, significant disparities persist. Sub-Saharan Africa remains a region with a disproportionately high burden of the disease. Other regions, such as Eastern Europe and Central Asia, have also seen increases in new infections in recent years.
Key affected populations include men who have sex with men (MSM), people who inject drugs (PWID), and sex workers. The epidemic continues to affect vulnerable populations, highlighting the importance of targeted interventions.
Prevalence Rates and Geographic Distribution
The global prevalence of HIV/AIDS is unevenly distributed. Certain regions, such as Southern Africa, have significantly higher rates than others. Factors such as poverty, limited access to healthcare, and social inequalities contribute to these disparities. For example, in countries with limited resources, access to testing and treatment is often hampered, leading to delayed diagnoses and treatment. The following table presents a simplified overview of prevalence rates and regions:
| Region | Estimated Prevalence Rate |
|---|---|
| Sub-Saharan Africa | High |
| Eastern Europe and Central Asia | Increasing |
| North America | Lower, but ongoing concerns for vulnerable populations |
Key Indicators of Progress
Monitoring progress towards ending the HIV/AIDS epidemic requires a set of key indicators. These indicators track changes in new infections, access to treatment, and related health outcomes. The World Health Organization (WHO) and UNAIDS provide comprehensive guidance and data on these indicators. Key indicators include:
- New HIV infections: Tracking the rate of new infections helps assess the effectiveness of prevention strategies and interventions.
- Antiretroviral therapy (ART) coverage: The proportion of people living with HIV who have access to ART is a crucial indicator of treatment success.
- Viral suppression: The percentage of people on ART who achieve viral suppression (undetectable viral load) reflects the effectiveness of treatment in preventing transmission.
- Testing and counseling: Ensuring access to testing and counseling services for all populations at risk is crucial for early diagnosis and prevention.
These indicators are essential for understanding the impact of interventions and informing future strategies. Monitoring these indicators helps in tailoring interventions and resource allocation for improved outcomes.
Fighting the HIV/AIDS epidemic is a massive undertaking, requiring innovative strategies and passionate individuals. One way to contribute is by building a strong, healthy community, which includes prioritizing physical well-being. Learning how to become a barre fitness instructor become a barre fitness instructor could be a rewarding career path that promotes health and fitness. Ultimately, fostering a healthier lifestyle through accessible fitness options is a critical piece of the puzzle in ending the HIV/AIDS epidemic.
Strategies for Ending the HIV/AIDS Epidemic
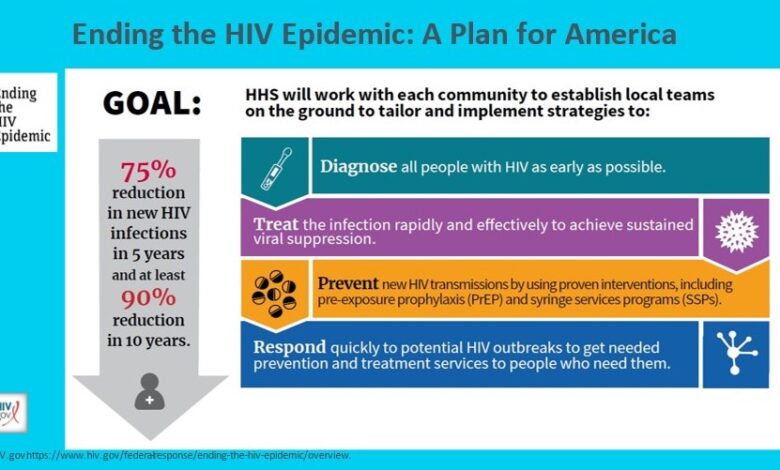
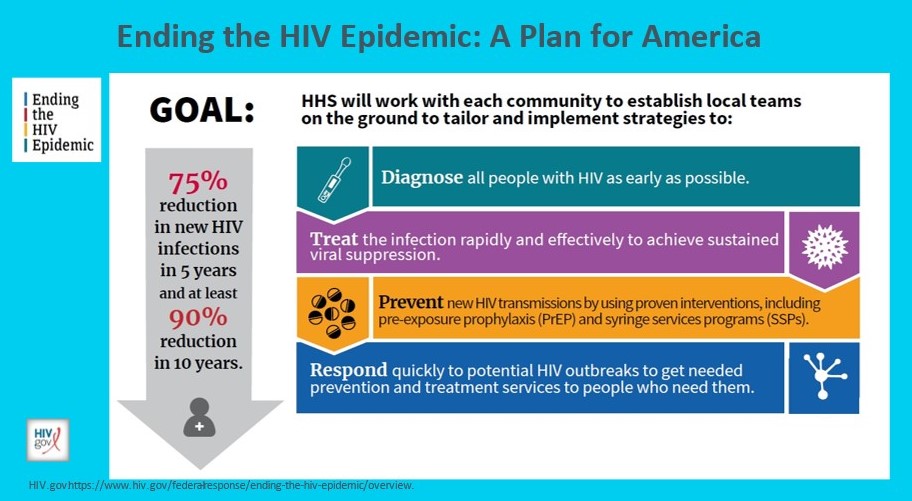
Ending the HIV/AIDS epidemic requires a multifaceted approach that tackles prevention, treatment, and care, while prioritizing community engagement. Global efforts must integrate evidence-based strategies with local contexts to maximize impact and ensure equitable access to resources. This comprehensive strategy necessitates a strong commitment from governments, healthcare providers, and individuals affected by the epidemic.The path to ending the HIV/AIDS epidemic hinges on a holistic strategy that goes beyond simply treating the disease.
It demands a comprehensive approach encompassing prevention, treatment, and care, all interwoven with robust community engagement. This approach recognizes the interconnectedness of these elements and acknowledges that success relies on the active participation of individuals, communities, and healthcare systems.
Prevention Strategies
Effective prevention strategies are crucial in stemming the spread of HIV. Different methods target various populations and have varying degrees of effectiveness. Careful consideration of potential limitations is essential to optimize their implementation and maximize impact.
- Pre-Exposure Prophylaxis (PrEP): PrEP involves taking medication to prevent HIV infection. It’s highly effective when taken consistently and can significantly reduce the risk of acquiring HIV. However, adherence to the regimen is crucial for optimal results. A key strength of PrEP is its ability to prevent infection in individuals at high risk, such as men who have sex with men (MSM), and transgender people.
Limitations include potential side effects and the need for consistent access to the medication.
- Post-Exposure Prophylaxis (PEP): PEP involves taking medication within 72 hours of potential HIV exposure. It can reduce the risk of infection if taken promptly and correctly. However, PEP is not a substitute for prevention and requires immediate access to healthcare. It is particularly useful in cases of sexual assault or accidental needle stick injuries. A significant limitation is the need for rapid access to healthcare and medication, which may not be readily available in all settings.
- Condoms: Consistent condom use remains a cornerstone of HIV prevention. Condoms offer a physical barrier against the transmission of HIV and other sexually transmitted infections. Condom use is highly effective when used correctly and consistently. Limitations include the potential for inconsistent use and the need for proper storage and handling.
Treatment Strategies
Effective treatment significantly impacts the lives of people living with HIV. Access to antiretroviral therapy (ART) is crucial in preventing progression to AIDS and improving overall health.
- Antiretroviral Therapy (ART): ART is a life-saving treatment for HIV. It suppresses the virus, preventing progression to AIDS and associated complications. ART is highly effective when taken consistently. A key strength is the ability to prevent transmission of HIV from an infected person to an uninfected person through sexual contact. Limitations can include potential side effects and the need for long-term adherence.
Care Strategies
Comprehensive care for people living with HIV encompasses physical and psychosocial support. This includes access to medical care, mental health services, and social support.
- Multidisciplinary Care: Care for people living with HIV should be provided by a team of healthcare professionals, including physicians, nurses, social workers, and mental health specialists. This multidisciplinary approach ensures holistic care, addressing both physical and psychosocial needs. It is particularly useful for ensuring long-term health and well-being, and for addressing the social determinants of health.
Public Health Interventions
Public health interventions play a critical role in preventing the spread of HIV and ensuring access to treatment and care. These interventions often involve raising awareness, education, and outreach to vulnerable populations.
Prevention Strategies Summary Table
| Method | Target Population | Effectiveness | Limitations |
|---|---|---|---|
| PrEP | Individuals at high risk | High, when taken consistently | Adherence, potential side effects |
| PEP | Individuals exposed to HIV | High, if taken promptly | Timely access to healthcare |
| Condoms | All sexually active individuals | High, when used correctly | Inconsistent use, storage |
Challenges and Barriers: Ending The Hiv Aids Epidemic
Ending the HIV/AIDS epidemic faces significant obstacles. While considerable progress has been made in prevention, treatment, and care, substantial challenges persist, demanding a multifaceted approach to overcome the systemic barriers that impede progress. These challenges vary significantly across different regions, necessitating tailored strategies and resources.The journey to eliminate HIV/AIDS requires not only medical breakthroughs but also a deep understanding of the complex interplay of social, economic, and political factors that perpetuate the epidemic.
Addressing stigma, ensuring equitable access to resources, and fostering community engagement are crucial elements of a comprehensive strategy.
Social and Cultural Barriers
Social stigma and discrimination remain major obstacles to HIV prevention and treatment. Fear of judgment and social exclusion often deter individuals from seeking testing, treatment, and support. This fear is compounded by misconceptions about HIV transmission and a lack of accurate information, creating a climate of fear and isolation. Many communities continue to experience discrimination, making it harder for people to access essential services.
Cultural norms and practices can also limit access to information and prevention services, particularly for vulnerable populations.
Economic Disparities
Economic disparities play a crucial role in hindering access to HIV prevention and treatment services. Poverty and lack of economic opportunity often limit access to healthcare, education, and social support networks. People living in poverty may face significant barriers in accessing testing, treatment, and care due to affordability issues, lack of transportation, and limited awareness of available services.
These economic disparities create a cycle of vulnerability, making individuals more susceptible to HIV infection and less likely to receive appropriate care.
Political and Policy Factors, Ending the hiv aids epidemic
Political will and policy decisions significantly impact the success of HIV/AIDS prevention and treatment efforts. Political instability, corruption, and lack of prioritization can hinder the allocation of resources and the implementation of effective programs. Policymakers need to create supportive environments and frameworks that promote access to care, prevention, and treatment. Legislation that addresses discrimination and stigma is essential to create a safe and equitable environment for people living with HIV.
Insufficient funding for HIV/AIDS programs is a common challenge in many regions.
Resource Constraints
Limited resources significantly impact efforts to end the HIV/AIDS epidemic. Inadequate funding for prevention programs, treatment, care, and research hinders progress. This shortage of resources often affects the quality and reach of services, particularly in resource-limited settings. Training of healthcare workers, procurement of essential medications, and ongoing monitoring and evaluation programs are often underfunded. A lack of skilled personnel and infrastructure further exacerbates these challenges.
Regional Variations in Challenges
| Region | Key Challenges | Examples |
|---|---|---|
| Sub-Saharan Africa | High prevalence, poverty, stigma, limited access to treatment, and weak healthcare systems. | Many rural communities lack access to testing and treatment centers. Stigma can prevent individuals from disclosing their HIV status, leading to isolation and poor health outcomes. |
| Eastern Europe and Central Asia | High rates of new infections, particularly among key populations, coupled with insufficient prevention and treatment programs. | Injection drug use is a significant driver of HIV transmission in some regions. Limited access to harm reduction services and stigma contribute to the spread of the virus. |
| South Asia | Large populations, complex social norms, and limited access to testing and treatment. | Cultural norms surrounding sexual health and gender roles can limit access to information and services. Discrimination against marginalized groups is prevalent. |
| Latin America | Growing epidemics in some countries, poverty, violence, and challenges in reaching vulnerable populations. | Violence and criminalization against sex workers and other key populations hinder their access to services. Economic inequalities lead to unequal access to care. |
Global Collaboration and Partnerships
Ending the HIV/AIDS epidemic requires a unified global effort, transcending national borders and individual interests. Collaboration is crucial for sharing resources, expertise, and best practices, fostering a coordinated response that reaches vulnerable populations worldwide. Effective partnerships are vital for building capacity, implementing evidence-based strategies, and ultimately achieving a world free from HIV/AIDS.Global collaboration is not merely a desirable goal; it is a necessity.
The interconnected nature of the epidemic demands a collective approach. The virus does not respect geographical boundaries; its spread and impact are felt across continents. A coordinated global response is critical to effectively address the challenges and ensure equitable access to prevention, treatment, and care for all affected communities.
Importance of International Organizations
International organizations play a pivotal role in coordinating global efforts to combat HIV/AIDS. They provide a platform for countries to share information, develop strategies, and pool resources. Organizations like UNAIDS, the World Health Organization (WHO), and the Global Fund to Fight AIDS, Tuberculosis, and Malaria are instrumental in facilitating these collaborations. Their expertise, experience, and global reach are invaluable in mobilizing resources and technical support for affected nations.
Role of Governments in Coordinating Efforts
National governments are responsible for implementing policies and programs within their borders. Strong leadership and political commitment are crucial to successfully integrating HIV/AIDS responses into national health strategies. Effective coordination between national governments and international organizations is paramount to achieving comprehensive epidemic control. Harmonizing national strategies with global initiatives is key to achieving a unified and effective global response.
Partnerships and Initiatives
Numerous partnerships and initiatives are underway to combat the HIV/AIDS epidemic. These include collaborations between governments, international organizations, non-governmental organizations (NGOs), community-based organizations, and private sector entities. These diverse partnerships leverage diverse strengths, ensuring that interventions are tailored to specific needs and address the unique challenges faced by different populations. The involvement of community organizations ensures that programs are culturally sensitive and community-driven.
Examples of Successful Global Collaborations
Successful global collaborations in combating infectious diseases provide valuable lessons for HIV/AIDS initiatives. The Global Fund to Fight AIDS, Tuberculosis, and Malaria, for example, has demonstrated the power of collaborative funding mechanisms to dramatically reduce the burden of these diseases. Other successful examples include the fight against polio and measles, highlighting the effectiveness of coordinated international efforts in achieving global health goals.
Responsibilities of Stakeholders
| Stakeholder | Responsibilities |
|---|---|
| Governments | Developing and implementing national HIV/AIDS strategies, allocating resources, and coordinating with international partners. |
| NGOs | Providing direct services, supporting community mobilization, and advocating for policy changes. |
| Individuals | Seeking testing and treatment, adhering to medication regimens, and promoting awareness and prevention within their communities. |
Addressing Specific Populations
The fight against HIV/AIDS requires a nuanced approach, recognizing that certain populations face unique challenges and vulnerabilities. Focusing on specific populations, such as men who have sex with men (MSM), transgender individuals, and people who inject drugs (PWID), is crucial for effective prevention and treatment strategies. These groups often encounter systemic discrimination, social stigma, and limited access to healthcare, which exacerbates their risk of HIV infection and hinders their ability to access vital care.
This necessitates tailored interventions that address their specific needs and empower them to make informed choices about their health.Tailoring prevention and treatment programs to these groups is essential to reduce disparities and improve health outcomes. This involves understanding the specific risks and barriers each group faces, and developing interventions that resonate with their lived experiences and cultural contexts.
This proactive approach fosters trust, promotes engagement, and ultimately leads to more successful outcomes in reducing the spread of HIV and improving the health of these populations.
Unique Challenges Faced by Specific Populations
Addressing the unique challenges of specific populations vulnerable to HIV/AIDS is crucial to effective prevention and treatment. Understanding the social, economic, and structural factors that contribute to their vulnerability is essential to develop appropriate responses. These populations often experience stigma, discrimination, and marginalization, which can lead to barriers in accessing healthcare and support services.
- Men who have sex with men (MSM): MSM face significant stigma and discrimination, often leading to social isolation and mental health issues. This can impact their willingness to engage with HIV prevention and testing services. Cultural norms and societal attitudes also play a role, creating barriers to accessing appropriate care and support.
- Transgender people: Transgender individuals face multiple layers of marginalization, including stigma, discrimination, and violence. These factors can significantly affect their access to healthcare, including HIV prevention and treatment. Many transgender individuals face discrimination from healthcare providers, which further compounds the challenges they face in accessing necessary services.
- People who inject drugs (PWID): PWID face complex challenges, including substance use disorders, poverty, and criminalization. These factors often lead to barriers in accessing healthcare and social support, making them highly vulnerable to HIV infection. The stigma associated with substance use can prevent PWID from seeking necessary care and treatment.
Strategies for Tailoring Prevention and Treatment Programs
Effective prevention and treatment programs must be tailored to address the specific needs of these vulnerable populations. This includes understanding their unique social and cultural contexts and incorporating these insights into program design.
- Culturally Appropriate Interventions: Interventions should be culturally appropriate, respectful of the diverse experiences and backgrounds of the populations they serve. This means engaging community leaders, utilizing culturally sensitive communication strategies, and ensuring that programs are delivered in languages and formats that are accessible to the target population.
- Community-Based Approaches: Community-based approaches are essential for fostering trust and engagement. Involving community organizations, peer educators, and local leaders in program design and delivery is crucial to ensuring that interventions are relevant and effective.
- Addressing Stigma and Discrimination: Combating stigma and discrimination is vital. This involves educating the public, advocating for policy changes, and creating supportive environments that promote inclusivity and respect.
Importance of Culturally Appropriate Interventions
Culturally appropriate interventions are crucial for successful engagement and effective health outcomes. These interventions recognize and respect the diverse cultural backgrounds, values, and beliefs of the target populations. This approach fosters trust, promotes openness, and increases the likelihood of individuals seeking and adhering to prevention and treatment services.
Role of Advocacy Groups
Advocacy groups play a critical role in promoting the rights and needs of these vulnerable populations. Their advocacy efforts can influence policy decisions, challenge discriminatory practices, and raise public awareness. Strong advocacy efforts are essential for creating supportive environments and ensuring access to vital services.
Specific Needs and Vulnerabilities Table
| Population | Specific Needs | Vulnerabilities |
|---|---|---|
| Men who have sex with men (MSM) | Stigma reduction, culturally sensitive education, accessible testing and prevention services, tailored support groups | Social isolation, discrimination, mental health issues, limited access to healthcare |
| Transgender people | Gender-affirming care, culturally competent healthcare providers, legal protections, safe spaces | Violence, discrimination, lack of access to healthcare, systemic barriers to gender affirmation |
| People who inject drugs (PWID) | Needle exchange programs, harm reduction strategies, treatment for substance use disorders, accessible HIV testing and treatment | Substance use disorders, poverty, criminalization, stigma associated with substance use, limited access to healthcare |
Measuring Progress and Evaluating Outcomes
Tracking progress towards ending the HIV/AIDS epidemic necessitates a robust system for measuring and evaluating outcomes. This involves more than just counting new infections; it requires a multifaceted approach that encompasses various factors influencing the epidemic’s trajectory. Effective monitoring allows for timely adjustments to strategies and ensures that resources are allocated efficiently. A critical component of this process is the establishment of clear performance indicators, allowing for objective assessments of success.Accurate and comprehensive data collection and analysis are indispensable for evaluating the impact of interventions and identifying areas needing improvement.
This data-driven approach provides insights into the effectiveness of various strategies, enabling the development of evidence-based programs that are more likely to achieve the desired outcomes. A crucial aspect of this is the use of key performance indicators (KPIs) to quantify progress and identify trends.
Methods for Tracking Progress
Tracking progress toward ending the HIV/AIDS epidemic involves a combination of quantitative and qualitative methods. These methods include epidemiological surveillance systems, routine data collection from healthcare facilities, community-based surveys, and qualitative assessments of social determinants of health. The integration of these diverse approaches provides a more complete picture of the epidemic’s evolution and the effectiveness of interventions. Crucially, these methods need to be standardized and regularly updated to ensure comparability and reliability of data.
Key Performance Indicators (KPIs)
Key performance indicators (KPIs) are essential metrics for evaluating the success of interventions. They provide a framework for quantifying progress toward specific goals, such as reducing new HIV infections, increasing access to treatment, and improving health outcomes. Choosing appropriate KPIs is crucial for accurately reflecting the impact of interventions and allowing for objective assessments of success. These indicators need to be relevant to the specific context of the epidemic and must align with global goals and targets.
Examples of Successful Interventions
Numerous interventions have demonstrated positive impacts on specific metrics. For instance, the expansion of antiretroviral therapy (ART) programs has significantly reduced AIDS-related deaths and improved the health and well-being of people living with HIV. The successful implementation of harm reduction strategies, such as needle exchange programs, has effectively reduced the spread of HIV among injecting drug users. Additionally, comprehensive prevention programs targeting key populations, including men who have sex with men, transgender individuals, and sex workers, have yielded positive results in lowering new HIV infections within these communities.
Data Collection and Analysis
Data collection and analysis play a vital role in evaluating outcomes and informing decision-making. Regular data analysis helps identify trends, assess the effectiveness of interventions, and pinpoint areas requiring adjustments. This process requires strong data management systems, trained personnel, and consistent data quality checks. The analysis should incorporate a range of perspectives, including community feedback and expert opinions.
This multi-faceted approach ensures a holistic understanding of the epidemic’s dynamics and the effectiveness of responses.
Ending the HIV/AIDS epidemic is a monumental task, demanding a multifaceted approach. It’s fascinating to see how the struggles surrounding addiction play out, like in the Netflix documentary on adderall epidemic, which highlights the devastating consequences of addiction. Ultimately, though, the focus must return to the powerful strategies that are needed to vanquish the HIV/AIDS epidemic entirely.
Table of Key Performance Indicators
| Metric | Target | Current Status | Projected Outcome |
|---|---|---|---|
| New HIV Infections | Reduce by 90% by 2030 | Decreased by 50% since 2010 | Further reduction to 75% by 2025, reaching the 90% target by 2030 |
| Access to Antiretroviral Therapy (ART) | 95% of people living with HIV on ART | 80% currently accessing ART | Achieving 90% access by 2025, exceeding the target by 2030 |
| Viral Suppression | 95% of people on ART with undetectable viral loads | 85% currently achieving viral suppression | Reaching 95% viral suppression by 2025 |
The Future of HIV/AIDS Prevention
The fight against HIV/AIDS is far from over, but the future holds immense promise for prevention strategies. Innovative approaches, new technologies, and a commitment to community engagement are crucial for achieving an HIV-free generation. Continued investment in research and implementation of proven strategies are essential to achieving this ambitious goal.The journey towards an HIV-free future demands a multifaceted approach, combining existing successful interventions with cutting-edge advancements.
This includes bolstering prevention efforts, fostering collaboration between researchers, healthcare providers, and communities, and ensuring equitable access to life-saving resources.
Pre-Exposure Prophylaxis (PrEP) and Other Innovative Approaches
Pre-exposure prophylaxis (PrEP) has emerged as a powerful tool in HIV prevention. PrEP involves taking antiretroviral medications daily to prevent HIV infection. Its effectiveness in reducing the risk of HIV acquisition is well-documented, with studies demonstrating significant reductions in HIV transmission rates among high-risk populations. The expansion of PrEP access to broader populations, including adolescents and young adults, is crucial for maximizing its impact.
Other innovative approaches, such as post-exposure prophylaxis (PEP), are also important and will continue to be developed.
New Technologies and Research
Advancements in technology and research hold immense potential for advancing HIV prevention strategies. The development of rapid diagnostic tests, point-of-care technologies, and digital health platforms can improve access to testing and treatment, particularly in resource-limited settings. Furthermore, research into novel prevention methods, including microbicides and vaccines, is ongoing. The development of a preventative vaccine would be a game-changer, significantly reducing the global burden of HIV.
Community-Based Research
Community-based research is essential for informing and implementing future HIV prevention interventions. By actively engaging communities in research design, implementation, and evaluation, we can ensure that interventions are relevant, culturally appropriate, and effective. This participatory approach allows for the integration of local knowledge and perspectives, which are critical for successful program implementation. Community engagement also builds trust and empowers individuals to take ownership of their health.
Advancements in Vaccine Development
Progress in vaccine development is yielding promising results. Researchers are exploring various approaches, including preventative vaccines, to reduce HIV transmission. Different vaccine platforms and strategies are being investigated, and ongoing clinical trials are evaluating their safety and efficacy. The ultimate goal is to create a vaccine that is highly effective, safe, and accessible to all. Developing a preventative vaccine is a long-term process requiring significant investment and collaboration among researchers, clinicians, and public health officials.
Innovative Prevention Strategies
| Strategy | Description | Potential Impact | Challenges |
|---|---|---|---|
| Pre-exposure Prophylaxis (PrEP) | Daily use of antiretroviral medication to prevent HIV infection. | Significant reduction in HIV transmission rates among high-risk populations. | Cost, adherence, and access to medication, particularly in resource-limited settings. |
| Post-exposure Prophylaxis (PEP) | Taking antiretroviral medication after potential exposure to HIV. | Reduces the risk of infection following exposure. | Timely access to PEP, adherence to the regimen, and awareness of potential exposure. |
| Microbial Vaccines | Development of vaccines targeting specific HIV-related microbial agents. | Potentially enhancing immune response to prevent infection. | Developing vaccines targeting various microbial agents, ensuring effectiveness, and maintaining long-term immunity. |
| Rapid Diagnostic Tests | Rapid and accurate detection of HIV infection. | Improved access to testing, enabling prompt diagnosis and treatment. | Cost-effectiveness, reliability, and accessibility in various settings. |
Closing Summary
In conclusion, ending the HIV/AIDS epidemic requires a global alliance, encompassing governments, organizations, communities, and individuals. The journey demands sustained effort, innovative strategies, and unwavering commitment to the vulnerable populations affected. While significant progress has been made, challenges remain, necessitating continued collaboration and a shared responsibility to achieve a future free from the devastating impact of this disease.





