Endometriosis mistaken for appendicitis is a frustrating reality for many women. Symptoms often overlap, leading to misdiagnosis and delayed treatment. This exploration delves into the complexities of these two conditions, examining their shared symptoms, diagnostic challenges, and the impact of misdiagnosis on patient well-being.
Understanding the subtle differences between endometriosis and appendicitis is crucial for accurate diagnosis. We’ll explore the commonalities in their initial presentation, the overlapping symptoms, and the diagnostic procedures that can sometimes lead to confusion. A comparative analysis will highlight key distinctions, like the location of pain and potential causes, to aid in recognizing the nuances between these conditions.
Introduction to the Condition
Endometriosis and appendicitis, while distinct conditions, can share overlapping symptoms, sometimes leading to misdiagnosis. Understanding their differences and shared characteristics is crucial for accurate diagnosis and effective treatment. Endometriosis is a condition where tissue similar to the lining of the uterus (the endometrium) grows outside the uterus, often affecting the ovaries, fallopian tubes, and surrounding tissues. Appendicitis, on the other hand, is an inflammation of the appendix, a small, finger-like pouch attached to the large intestine.
Both can cause significant pain, often in the lower abdomen, making differentiation challenging.The initial presentation of both conditions frequently involves similar symptoms, such as lower abdominal pain, cramping, and nausea. These shared symptoms can obscure the underlying cause, potentially delaying appropriate medical intervention and potentially leading to unnecessary interventions or complications. A thorough medical history, physical examination, and diagnostic testing are essential for differentiating between the two.
Distinguishing Symptoms
Understanding the distinct symptom profiles of endometriosis and appendicitis is crucial for differentiating them. Endometriosis often presents with cyclical pain, worsening during menstruation. Appendicitis pain, while often starting around the belly button, typically migrates to the lower right quadrant of the abdomen. Variations in pain intensity and location can also occur.
Comparison of Endometriosis and Appendicitis
The following table summarizes the key differences between endometriosis and appendicitis in terms of symptoms, location of pain, and potential causes.
| Characteristic | Endometriosis | Appendicitis |
|---|---|---|
| Symptoms | Pelvic pain, cramping, heavy bleeding during menstruation, painful intercourse, pain with bowel movements, and sometimes pain during urination. | Periumbilical pain (around the belly button) that migrates to the lower right quadrant of the abdomen, nausea, vomiting, loss of appetite, fever, and constipation. |
| Location of Pain | Typically localized in the pelvis, lower abdomen, and sometimes lower back. Can also radiate to the groin or thighs. | Initially around the belly button, migrating to the lower right quadrant of the abdomen. |
| Potential Causes | Growth of endometrial tissue outside the uterus. Hormonal factors may play a role. | Inflammation of the appendix, often due to blockage. Possible causes include infection, foreign bodies, or tumors. |
Commonalities in Initial Presentation
Despite their distinct characteristics, both conditions share some commonalities in their initial presentation. For instance, both can present with vague abdominal pain, making early diagnosis challenging. The presence of associated symptoms, such as nausea, vomiting, and fever, can further complicate the differentiation. In such cases, a detailed medical history and thorough physical examination are vital for accurate diagnosis.
Symptoms and Diagnostic Challenges
Navigating the complexities of reproductive health can be challenging, especially when dealing with overlapping symptoms. This is particularly true when trying to distinguish between endometriosis and appendicitis, two conditions that can present with strikingly similar initial indicators. The resulting diagnostic journey can be fraught with uncertainty and delay, highlighting the critical need for accurate and timely assessment.
Overlapping Symptoms
Both endometriosis and appendicitis can manifest with a range of abdominal pain, often localized in the lower right quadrant. This similarity in location and presentation makes initial diagnosis difficult. Pain intensity, duration, and accompanying symptoms can vary significantly between individuals, adding another layer of complexity to the diagnostic process. The presence of fever, nausea, vomiting, and tenderness in the lower abdomen can occur in both conditions, obscuring the specific underlying cause.
This overlap in symptoms often leads to a period of uncertainty and potentially delays in receiving appropriate treatment.
Distinguishing Features
While several symptoms overlap, certain indicators can subtly suggest one condition over the other. For instance, cyclical pain patterns, particularly those linked to menstruation, might point towards endometriosis. Conversely, a sudden onset of severe pain, accompanied by a rapid increase in symptoms, could be more indicative of appendicitis.
Symptoms Comparison
| Symptom | Endometriosis Possible Interpretation | Appendicitis Possible Interpretation |
|---|---|---|
| Lower abdominal pain | Often cyclical, can worsen during menstruation, may be chronic. | Sudden onset, sharp, often localized to the lower right quadrant. |
| Pelvic pain | Common, often associated with sexual intercourse or bowel movements. | Less common, usually less severe than the lower abdominal pain. |
| Menstrual irregularities | Heavy or prolonged bleeding, painful periods (dysmenorrhea). | Usually not associated with menstrual cycles. |
| Nausea and vomiting | Can occur, but less frequently and less severe compared to appendicitis. | More common, often severe and accompanied by other symptoms. |
| Fever | Less likely to be present without other associated conditions. | More likely, especially with increasing severity of pain. |
| Tenderness to touch | Tenderness may be present, but typically more generalized in the pelvic area. | Marked tenderness, especially in the lower right quadrant. |
| Bowel and bladder changes | Possible bloating, constipation, or changes in urination frequency. | Possible but less pronounced compared to the other symptoms. |
Importance of a Thorough History
A detailed medical history, including menstrual history, family history, and past medical conditions, is crucial. Physicians must carefully consider the duration and character of the pain, its relationship to menstruation, and other accompanying symptoms. This process helps to identify patterns and clues that may not be apparent from the physical examination alone.
Diagnostic Procedures and Misdiagnosis
The journey to a correct diagnosis for both appendicitis and endometriosis can be fraught with challenges. Often, symptoms overlap, making it difficult for even experienced medical professionals to differentiate between the two conditions initially. This often results in misdiagnosis, which can have serious implications for the patient’s health and well-being.This section explores the typical diagnostic procedures used for each condition and how these procedures can sometimes yield similar results, leading to confusion.
We’ll also examine the limitations of current diagnostic tools in precisely differentiating between these two conditions.
Typical Diagnostic Procedures for Appendicitis
Initial diagnosis of appendicitis typically involves a thorough physical examination, focusing on abdominal tenderness, particularly in the lower right quadrant. A detailed patient history, including a description of symptoms, onset, and any associated factors, is crucial. Laboratory tests, such as a complete blood count (CBC) to check for infection markers, may be ordered. The CBC can reveal an elevated white blood cell count (WBC), often a sign of inflammation.
Furthermore, imaging studies, such as an ultrasound or CT scan, are frequently used to visualize the appendix and surrounding structures. An ultrasound is often the first imaging choice, particularly for pregnant women. CT scans provide more detailed anatomical information, and are frequently employed when an ultrasound is inconclusive or other complications are suspected.
Typical Diagnostic Procedures for Endometriosis
Diagnosis of endometriosis is considerably more complex. There’s no single definitive test, and the process often involves ruling out other conditions. A comprehensive medical history, including a detailed description of pain patterns, menstrual cycles, and any previous surgeries, is paramount. Pelvic examinations are frequently conducted, often revealing tenderness and scarring, though this can be unreliable. Imaging studies, such as ultrasound or MRI, can help identify endometrial implants, though they aren’t always conclusive.
Laparoscopy, a surgical procedure involving inserting a small camera into the abdomen, is often necessary for a definitive diagnosis. During laparoscopy, the surgeon can directly visualize the pelvic organs and identify endometrial tissue. Biopsies taken during the laparoscopy can confirm the presence of endometriosis.
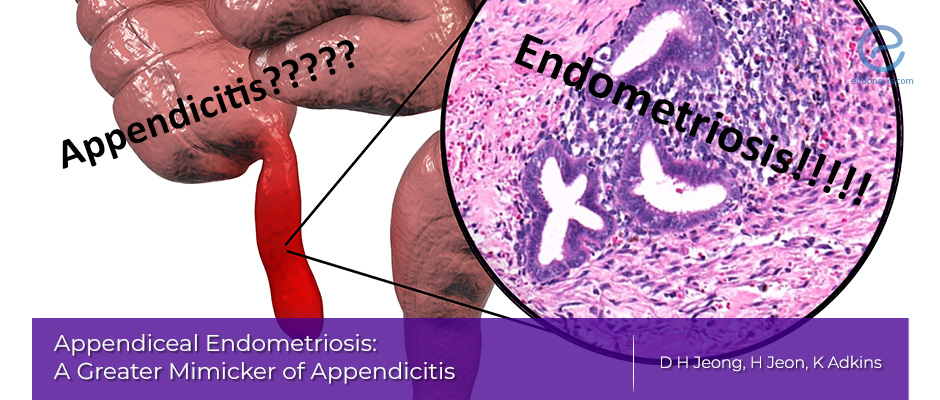
Similarities and Potential for Misinterpretation
Both appendicitis and endometriosis can present with lower abdominal pain, often accompanied by nausea and fever. The location of the pain may overlap, with tenderness potentially found in the lower right quadrant, a common area for appendicitis, but also possible in endometriosis. An elevated WBC count, while a common indicator of infection in appendicitis, can also be elevated in response to inflammation associated with endometriosis.
Early-stage endometriosis may not be visually apparent on imaging studies, and its location can mimic appendicitis. This overlap in symptoms and potential imaging findings makes differentiation difficult.
Limitations of Current Diagnostic Tools
Currently, there aren’t any perfectly reliable diagnostic tools capable of distinguishing between appendicitis and endometriosis with complete certainty. The reliance on symptoms, imaging findings, and even laparoscopy can be insufficient in ambiguous cases. The severity of symptoms can vary significantly between individuals, and the location of pain can overlap. The subtlety of some endometriosis presentations, especially early-stage disease, can further complicate the diagnostic process.
So, I was reading about how endometriosis can sometimes be mistaken for appendicitis, which is seriously concerning. It’s a tricky situation, and apparently, the symptoms can overlap a lot. This often leads to delayed diagnosis, which is a huge problem. Thinking about that, it got me wondering about the sleep deprivation many people experience after the Super Bowl.
Apparently, a recent survey found that 40% of Americans report being sleep-deprived after the big game 40 of americans say theyre sleep deprived after the super bowl. Maybe that exhaustion contributes to misdiagnosis, making it harder to pinpoint the true issue, like endometriosis? It’s definitely a complex web of potential factors, and hopefully, better awareness of these things will lead to quicker, more accurate diagnoses.
The lack of a definitive biomarker further contributes to the challenge.
Diagnostic Comparison Table
| Diagnostic Feature | Appendicitis | Endometriosis | Potential for Misinterpretation |
|---|---|---|---|
| Pain Location | Lower right quadrant | Lower abdomen, potentially overlapping with appendicitis | Overlapping pain locations can mislead diagnosis |
| Imaging Findings | Possible visualization of inflamed appendix on ultrasound/CT | Possible visualization of endometrial implants on MRI/ultrasound, but subtle in early stages | Similar findings on imaging can lead to confusion |
| Laboratory Tests | Elevated WBC count | Elevated WBC count possible due to inflammation | Elevated WBC count doesn’t definitively distinguish between conditions |
| Definitive Diagnosis | Often surgical removal of appendix (appendectomy) | Laparoscopy and biopsy | Misinterpretation can result in unnecessary surgery or delayed treatment |
Impact of Misdiagnosis

Misdiagnosis of endometriosis as appendicitis can have devastating consequences, extending far beyond a simple surgical error. The delay in receiving the correct diagnosis and treatment can significantly impact a woman’s overall health and well-being, leading to chronic pain, fertility issues, and psychological distress. This section will delve into the ramifications of this unfortunate misdiagnosis.The misidentification of endometriosis as appendicitis often results in a delay in appropriate treatment for the underlying condition.
This delay can lead to the progression of endometriosis, causing more severe symptoms and potentially increasing the difficulty in subsequent diagnoses and treatments. This delay in care can be particularly detrimental for individuals who may experience debilitating pain and have their symptoms dismissed or minimized due to the misdiagnosis.
Potential Consequences of Delayed Endometriosis Treatment
The consequences of delayed treatment for endometriosis can manifest in various ways. A delay in diagnosis can result in a more aggressive form of the disease, potentially leading to the need for more invasive procedures and a reduced chance of successful treatment. Furthermore, the delay can hinder fertility prospects, as endometriosis can affect the reproductive organs and potentially cause infertility.
Early and accurate diagnosis allows for timely intervention and management, reducing the risk of long-term complications.
Impact on Overall Health and Well-being
Delayed treatment for endometriosis can significantly affect a woman’s physical and emotional well-being. Chronic pain, often a hallmark of endometriosis, can lead to fatigue, anxiety, and depression. The uncertainty and frustration associated with misdiagnosis and delayed treatment can further exacerbate these emotional burdens. A timely diagnosis allows for tailored pain management strategies and emotional support, minimizing the detrimental impact on overall well-being.
Long-Term Effects of Delayed Endometriosis Treatment
The table below illustrates the potential long-term effects of delayed endometriosis treatment, highlighting the importance of early and accurate diagnosis. It’s crucial to recognize that these are potential consequences and individual experiences can vary significantly.
Ever wondered how easily endometriosis can be mistaken for appendicitis? Symptoms can be so similar, making diagnosis tricky. Thankfully, companies like the one working on a pill that would replace injected drugs company working on pill that would replace injected drugs are exploring innovative treatments, potentially leading to more accurate diagnoses and better management of conditions like endometriosis.
Hopefully, this will reduce the misdiagnosis rates for conditions like endometriosis.
| Area of Impact | Potential Long-Term Effects |
|---|---|
| Pain Management | Chronic, debilitating pain; increased difficulty in pain management; need for more aggressive and potentially invasive pain management strategies. |
| Fertility | Reduced fertility; difficulty conceiving; potential infertility; increased risk of ectopic pregnancy. |
| Emotional Well-being | Increased anxiety and depression; feelings of frustration, uncertainty, and helplessness; decreased quality of life. |
| Physical Health | Increased risk of adhesions and scar tissue formation; potential damage to surrounding organs; increased risk of ovarian cysts. |
| Reproductive Health | Potential for complications during pregnancy; potential for miscarriages or premature births. |
Importance of Accurate Diagnosis
Getting the right diagnosis for endometriosis is crucial. It’s the key to receiving the most effective treatment and managing the condition’s impact on your life. A correct diagnosis allows for tailored therapies, helping to alleviate pain, improve quality of life, and potentially prevent long-term complications. Incorrect diagnoses, especially when symptoms mimic other conditions, can lead to delayed or inappropriate treatment, further exacerbating the issue.Accurate diagnosis is not just about identifying the condition, but also understanding its severity and individual presentation.
This allows healthcare providers to create a personalized treatment plan that addresses the unique needs of each patient. Moreover, it empowers patients to make informed decisions about their care and actively participate in their recovery journey.
Critical Role of Accurate Diagnosis in Effective Treatment
A precise diagnosis of endometriosis, distinguishing it from other potential causes, is paramount for successful treatment. Treatment options vary based on the severity of the condition and the patient’s individual circumstances. For example, mild endometriosis may respond well to over-the-counter pain relievers, while severe cases might require surgery or hormonal therapies. Accurate diagnosis ensures that the most appropriate and effective treatment strategy is implemented, leading to better outcomes.
Importance of Considering Alternative Diagnoses
When presented with ambiguous symptoms, considering alternative diagnoses is crucial. Endometriosis symptoms can mimic those of other conditions, including appendicitis, ovarian cysts, or pelvic inflammatory disease. This highlights the importance of a comprehensive diagnostic approach that explores all possibilities before arriving at a definitive conclusion. A thorough evaluation helps to rule out other potential conditions, ensuring the most accurate and appropriate treatment plan is implemented.
Need for a Thorough Medical History and Physical Examination, Endometriosis mistaken for appendicitis
A detailed medical history and a comprehensive physical examination are essential components of accurate diagnosis. The history should include a detailed account of symptoms, their duration, frequency, and any associated factors. The physical examination should focus on identifying any physical findings that might provide clues about the underlying condition. This combined approach helps to gather a complete picture of the patient’s condition and potential causes, leading to a more informed diagnosis.
Significance of a Multidisciplinary Approach to Diagnosis
A multidisciplinary approach involving various specialists can significantly enhance the accuracy of endometriosis diagnosis. Collaboration between gynecologists, pain management specialists, and other relevant healthcare professionals can lead to a more comprehensive evaluation and a better understanding of the patient’s unique needs. This collaborative effort ensures that the patient receives the most appropriate and effective treatment plan, tailored to their specific situation.
Case Studies
Unfortunately, misdiagnosis of endometriosis as appendicitis is a reality for many women. These cases highlight the complexities of medical diagnostics and the crucial role accurate initial assessments play in effective treatment. The symptoms can be strikingly similar, making differentiation challenging. These real-life examples underscore the importance of a thorough diagnostic process and emphasize the need for a high index of suspicion for endometriosis, especially in women presenting with persistent pelvic pain.
Examples of Misdiagnosis
Several factors can contribute to a misdiagnosis. One key element is the subtle and often overlapping nature of symptoms. A patient may experience pain in the lower abdomen, mimicking appendicitis, which can be accompanied by nausea, vomiting, and fever. The initial examination might reveal tenderness in the right lower quadrant, a typical sign of appendicitis. However, the underlying condition could be endometriosis.
Case Study 1: Sarah’s Story
Sarah, a 27-year-old woman, experienced severe abdominal pain, accompanied by nausea and a low-grade fever. The pain was localized in the right lower quadrant, a classic presentation for appendicitis. Initial blood tests and imaging scans (such as an ultrasound) indicated inflammation in the appendix. Surgical intervention was deemed necessary. However, during the appendectomy, the surgeon discovered endometriosis implants in the surrounding tissues.
The extensive endometriosis obscured the inflamed appendix, leading to a misdiagnosis. Post-operative examination revealed the true nature of the condition, and Sarah received appropriate treatment for endometriosis.
Case Study 2: Emily’s Journey
Emily, a 32-year-old woman, presented with intermittent pelvic pain for several months. The pain was often accompanied by bloating and irregular menstrual cycles. The pain intensified, mimicking appendicitis, leading to an initial diagnosis of appendicitis. Repeated bouts of pain prompted further investigations, including a CT scan. The CT scan results did not clearly indicate appendicitis.
A second opinion and a detailed history eventually revealed the presence of endometriosis, and Emily underwent a minimally invasive surgical procedure to address the endometriosis.
Case Study 3: Jessica’s Experience
Jessica, a 20-year-old, experienced severe abdominal pain, accompanied by fever and vomiting. The pain was localized to the right lower quadrant. The symptoms were suggestive of appendicitis. Initial blood tests and ultrasound results indicated inflammation consistent with appendicitis. A subsequent laparoscopic appendectomy revealed endometriosis lesions, indicating the initial diagnosis was inaccurate.
This case underscores the need for a comprehensive diagnostic approach, especially when initial investigations do not fully elucidate the cause of the pain.
Summary of Case Studies
| Patient | Age (Years) | Symptoms | Initial Diagnosis | Outcome |
|---|---|---|---|---|
| Sarah | 27 | Severe abdominal pain, nausea, low-grade fever, localized pain in right lower quadrant | Appendicitis | Correct diagnosis of endometriosis after appendectomy |
| Emily | 32 | Intermittent pelvic pain, bloating, irregular menstrual cycles, increasing pain mimicking appendicitis | Appendicitis | Diagnosis of endometriosis and subsequent treatment |
| Jessica | 20 | Severe abdominal pain, fever, vomiting, localized pain in right lower quadrant | Appendicitis | Correct diagnosis of endometriosis after appendectomy |
Risk Factors
Understanding the risk factors for endometriosis and appendicitis is crucial for correctly diagnosing these conditions, especially when one mimics the other. This knowledge can help healthcare providers identify patients who might be more susceptible to misdiagnosis and develop targeted diagnostic strategies. Identifying potential overlaps in risk factors can also illuminate why a patient might present with symptoms suggestive of both conditions.
Risk Factors Associated with Endometriosis
Endometriosis, a condition where endometrial tissue grows outside the uterus, affects women of reproductive age. Several factors contribute to the development of this condition. Age is a significant factor, as endometriosis is more prevalent in women in their reproductive years. Family history of endometriosis also increases the risk. Certain lifestyle factors, such as smoking and obesity, can potentially contribute to the condition.
Moreover, there’s a possible link between endometriosis and certain hormonal imbalances or immune system responses.
- Age: Women of reproductive age are at higher risk due to hormonal fluctuations and reproductive cycles.
- Family History: A family history of endometriosis significantly increases the risk of developing the condition.
- Lifestyle Factors: Smoking and obesity are potential risk factors, although the exact mechanisms are still under investigation.
- Hormonal Factors: Imbalances in hormone levels might play a role in the development of endometriosis.
- Immune System Response: Some studies suggest a possible connection between the immune system and endometriosis, although the exact relationship remains unclear.
Risk Factors Associated with Appendicitis
Appendicitis, inflammation of the appendix, often presents with abdominal pain. Several factors contribute to the risk of developing appendicitis. Age, although appendicitis can occur at any age, is often more prevalent in adolescents and young adults. Certain medical conditions, such as cystic fibrosis and Crohn’s disease, might increase the risk. Furthermore, certain anatomical variations in the appendix can increase susceptibility.
Ever wonder how misdiagnosis can delay treatment? I’ve been researching endometriosis, and it’s truly fascinating how often it’s mistaken for appendicitis. It highlights the importance of understanding your body’s complex signals. That’s why I’m now also interested in how using your body clock to treat cancer, as detailed in this insightful piece using your body clock to treat cancer , could potentially revolutionize treatments.
Ultimately, better understanding our own internal rhythms might be key to more accurate diagnoses, especially when dealing with conditions like endometriosis.
- Age: While appendicitis can affect individuals of any age, adolescents and young adults are more frequently affected.
- Underlying Medical Conditions: Conditions like cystic fibrosis and Crohn’s disease can increase the risk of appendicitis.
- Anatomical Variations: Variations in the appendix’s location or structure can increase the risk of obstruction and subsequent inflammation.
- Certain Medications: Certain medications may influence the risk, though this is not a primary factor.
Overlapping Risk Factors and Misdiagnosis
Some risk factors for endometriosis and appendicitis might overlap, potentially leading to diagnostic challenges. For instance, both conditions can cause lower abdominal pain, and age is a factor for both. A family history of either condition could also be a contributing factor. This overlap can make differentiating between the two conditions more difficult, particularly in cases where the symptoms are less pronounced or atypical.
In some situations, the severity of symptoms might vary, influencing the accuracy of diagnosis.
Specific Risk Factors Increasing Misdiagnosis Likelihood
Certain circumstances increase the likelihood of misdiagnosis when endometriosis is mistaken for appendicitis. These include cases with atypical symptoms, where the presentation is not consistent with typical appendicitis or endometriosis. A lack of specific diagnostic tests tailored to these particular scenarios can also contribute to misdiagnosis. Furthermore, the lack of a clear understanding of the interplay between the two conditions can lead to incorrect interpretations of the symptoms.
- Atypical Symptoms: Cases with symptoms that deviate from typical presentations for either condition can hinder accurate diagnosis.
- Limited Diagnostic Tests: A lack of specialized tests specifically designed for differentiating endometriosis and appendicitis can lead to misdiagnosis.
- Incomplete Understanding of Interplay: Inadequate understanding of how these two conditions might interact and present symptoms can contribute to diagnostic errors.
Prevention and Early Detection
Navigating the complexities of endometriosis and appendicitis, especially when one mimics the other, necessitates proactive measures to prevent misdiagnosis and improve early detection. Understanding the symptoms, recognizing potential red flags, and knowing when to seek medical attention are crucial steps in this process. By empowering ourselves with knowledge and utilizing available resources, we can work towards a future where accurate diagnoses are prioritized.
Strategies to Prevent Misdiagnosis
Accurate medical history taking and a thorough physical examination are foundational to avoiding misdiagnosis. Patients should meticulously document all symptoms, including their onset, duration, and intensity. This detailed record can significantly aid clinicians in distinguishing between various conditions. A detailed history encompassing previous medical conditions, surgeries, and family history of endometriosis or other related conditions can provide invaluable context for diagnosis.
Open communication between patients and healthcare providers is paramount; patients should feel comfortable expressing their concerns and providing as much detail as possible.
Methods to Improve Early Detection
Early detection of both endometriosis and appendicitis is essential for timely treatment and improved outcomes. Raising awareness about the subtle signs and symptoms of these conditions is critical. Endometriosis, often characterized by chronic pelvic pain, can manifest in various ways, making early detection challenging. Awareness campaigns and educational materials can help individuals recognize the potential symptoms and encourage them to seek prompt medical attention.
For appendicitis, early detection hinges on recognizing the initial, often vague symptoms. Promoting public understanding of appendicitis’s diverse presentation can facilitate early intervention.
When to Seek Medical Attention
Prompt medical attention is vital when experiencing symptoms suggestive of either endometriosis or appendicitis. Persistent pelvic pain, particularly when accompanied by heavy bleeding, bowel irregularities, or pain during intercourse, warrants immediate medical evaluation. Sudden, severe abdominal pain, especially if accompanied by nausea, vomiting, or fever, demands immediate medical attention. The severity and duration of symptoms should guide the urgency of seeking medical attention.
Flowchart for Symptom Evaluation
The following flowchart Artikels the steps to take when experiencing symptoms suggestive of endometriosis or appendicitis:
| Symptom | Action |
|---|---|
| Persistent pelvic pain (especially with heavy bleeding, bowel irregularities, or pain during intercourse) | Schedule an appointment with a gynecologist or general practitioner. |
| Sudden, severe abdominal pain (accompanied by nausea, vomiting, or fever) | Seek immediate emergency medical attention. |
| Vague, intermittent abdominal pain (with or without accompanying symptoms) | Schedule an appointment with a general practitioner to discuss concerns. |
| Family history of endometriosis or appendicitis | Discuss family history with physician during consultation. |
This flowchart serves as a guide, and individual circumstances may necessitate variations in the course of action. It is essential to consult with a healthcare professional for personalized guidance.
Ending Remarks: Endometriosis Mistaken For Appendicitis
In conclusion, the potential for misdiagnosis between endometriosis and appendicitis underscores the importance of a thorough and attentive approach to patient care. Delays in proper treatment for endometriosis can have severe long-term consequences. By highlighting the challenges in diagnosis, the potential for misinterpretation, and the importance of considering alternative diagnoses, we aim to promote a greater understanding of this complex issue and ultimately improve patient outcomes.
Accurate diagnosis is paramount, and a multidisciplinary approach, including a careful medical history and physical examination, is crucial to avoiding the devastating effects of delayed care.