Fast lane racing with diabetes presents unique challenges, but also incredible opportunities for success. This guide delves into the physical and mental demands of high-performance racing, and how diabetes management strategies can optimize performance while mitigating risks. We’ll explore pre-race meal planning, insulin adjustments, monitoring techniques, and the critical role of technology, support systems, and safety precautions.
From understanding the physiological differences between racers with and without diabetes to crafting personalized meal plans and leveraging advanced technologies, this comprehensive resource aims to empower racers with diabetes to navigate the fast lane safely and effectively.
Understanding the Challenges

Fast lane racing, a high-octane pursuit of speed and precision, demands exceptional physical and mental fortitude. Beyond the sheer speed and agility, racers face a constant barrage of stressors, including the intense pressure to perform at peak levels, the complex interplay of the vehicle and the track, and the ever-present danger of accidents. This dynamic environment presents unique challenges for individuals managing diabetes, a chronic condition requiring meticulous blood sugar management.The demands of fast lane racing extend far beyond simple physical exertion.
The mental concentration required to anticipate turns, react to sudden changes in the racing environment, and maintain consistent performance over extended periods is immense. Racers must constantly monitor their vehicles, track conditions, and their own physiological responses, while also adapting to the strategies of their competitors. This mental acuity is crucial for success, but it also places a significant strain on both the body and the mind.
Physical Demands of Fast Lane Racing
The physical demands of fast lane racing are considerable. Racers must exhibit exceptional strength, stamina, and agility. Repeated acceleration, braking, and cornering place extreme stress on the cardiovascular system, requiring high levels of endurance. This physical exertion is compounded by the need for quick reflexes and precise movements, necessitating a high degree of coordination and motor control.
These demanding physical requirements can be further complicated by the potential impact of diabetes.
Impact of Diabetes on Physical Endurance
Diabetes can significantly affect physical endurance and stamina during high-performance activities like fast lane racing. Insulin resistance or insufficient insulin production can hinder the body’s ability to utilize glucose effectively for energy. This can lead to fatigue, decreased muscle strength, and impaired recovery. Furthermore, long-term complications associated with diabetes, such as nerve damage and cardiovascular issues, can exacerbate these effects.
Fast lane racing, while thrilling, can be incredibly dangerous, especially when coupled with diabetes. The risks are amplified by other risky behaviors, like the concerning rise in flavored tobacco use among teens. This trend highlights a worrying pattern of poor choices that can compound health issues. Ultimately, focusing on preventative measures and responsible choices is crucial for those pursuing high-speed activities and managing diabetes effectively.
In particular, fluctuating blood glucose levels during periods of intense physical exertion can pose significant risks.
Maintaining Blood Sugar Levels During Races
Maintaining stable blood sugar levels during races is paramount for racers with diabetes. Fluctuations in blood glucose can negatively impact performance, leading to fatigue, dizziness, and reduced concentration. Careful monitoring and precise adjustments to insulin dosages and dietary intake are crucial. Racers must develop a personalized strategy that considers the specific demands of the race, including the duration, intensity, and environmental conditions.
This may involve pre-race meals, intra-race carbohydrate intake, and post-race recovery strategies tailored to their individual needs.
Physiological Responses to Intense Physical Exertion
The physiological responses of athletes with and without diabetes to intense physical exertion differ significantly. Athletes without diabetes typically exhibit a controlled and predictable response, with a gradual increase in heart rate, breathing rate, and energy expenditure. Conversely, athletes with diabetes may experience more erratic and unpredictable responses due to fluctuating blood glucose levels. The unpredictability of these physiological responses can create significant challenges for racers with diabetes, demanding a more proactive and vigilant approach to monitoring and managing their blood sugar levels.
Emotional and Psychological Toll
Managing diabetes while pursuing high-performance racing goals presents a significant emotional and psychological toll. The constant vigilance required to maintain blood sugar control, the fear of hypoglycemia or hyperglycemia, and the potential impact on performance can be emotionally draining. Racers with diabetes may experience increased stress, anxiety, and feelings of vulnerability. Developing strong coping mechanisms, a supportive network of friends and family, and a well-structured management plan are crucial for navigating these emotional challenges.
Strategies for Management
Successfully navigating a fast-lane race with diabetes requires meticulous planning and adaptability. Effective management hinges on understanding your body’s unique response to physical exertion and glucose fluctuations. This involves pre-race meal planning, precise insulin adjustments, consistent blood glucose monitoring, strategic hydration, and a well-defined pacing strategy. By incorporating these strategies, racers can minimize the risk of complications and optimize performance.
Pre-Race Meal Planning
Proper nutrition before a race is crucial for maintaining stable blood glucose levels. A balanced pre-race meal should include complex carbohydrates, lean protein, and healthy fats. This combination provides sustained energy release, preventing rapid spikes and subsequent crashes in blood sugar. For example, a meal consisting of brown rice, grilled chicken breast, and a side salad provides a balanced source of carbohydrates, protein, and healthy fats, sustaining energy levels throughout the race.
Timing of this meal is also essential, consuming it several hours before the race to allow for digestion and glucose absorption.
Insulin Management and Adjustments
Insulin management during and after a race requires careful adjustments based on anticipated exertion and blood glucose levels. Insulin sensitivity often changes during physical activity. Adjusting insulin doses to account for this change is crucial to prevent hypoglycemia or hyperglycemia. Racers should consult with their healthcare team to develop a personalized insulin management plan, considering their specific needs and the anticipated demands of the race.
This plan should include adjustments for different race phases and potential scenarios.
“Individualized insulin regimens are essential for managing blood glucose fluctuations during strenuous physical activity.”
Blood Glucose Monitoring Techniques
Frequent monitoring of blood glucose levels is essential for real-time adjustments in insulin and nutrition. Continuous glucose monitoring (CGM) systems offer valuable insights into glucose trends, enabling proactive adjustments to maintain optimal blood glucose levels. These systems provide continuous data, allowing for timely interventions to prevent hypoglycemia or hyperglycemia. Manual blood glucose testing, using a glucometer, can be used in conjunction with CGM data, especially in situations where CGM is unavailable or inaccurate.
The choice of monitoring method should be tailored to the racer’s comfort level and the specific race environment.
Fast lane racing with diabetes presents unique challenges, requiring careful blood sugar management. It’s fascinating to consider how seemingly disparate issues, like the debate over the relationship between autism and allergies, debate over relationship between autism allergies , might also have underlying complex factors. Ultimately, understanding these factors can help us navigate similar difficulties in managing the physical and emotional demands of fast lane racing with diabetes.
Hydration Strategies
Hydration plays a significant role in blood sugar regulation. Dehydration can impair insulin function and lead to glucose imbalances. Racers should maintain consistent hydration throughout the race by consuming fluids at regular intervals, even if they don’t feel thirsty. This strategy helps maintain blood volume and supports the body’s ability to regulate glucose levels. Choosing appropriate hydration solutions is crucial, as some sugary drinks can further exacerbate blood sugar fluctuations.
Pacing Strategies
A well-defined pacing strategy can significantly impact blood sugar management. Gradual increases in intensity during the race can help maintain a more stable blood glucose level. Avoiding sudden bursts of high-intensity activity that can trigger rapid glucose fluctuations is crucial. Careful consideration of individual glucose responses to exertion is essential in optimizing pacing. Adjustments to the pacing strategy may be necessary based on blood glucose readings and individual needs.
Typical Blood Glucose Targets and Adjustments
| Race Phase | Target Blood Glucose (mg/dL) | Insulin Adjustment | Dietary Considerations |
|---|---|---|---|
| Warm-up | 100-150 | May require minor adjustments based on pre-race meal | Light snack or drink if needed |
| Race | 120-180 | Adjustments based on exertion and CGM data | Regular fluid intake and small, easily digestible snacks |
| Cool-down | 120-140 | Reduce insulin if needed | Light meal to replenish glycogen stores |
This table provides a general guideline for blood glucose targets. It’s crucial to consult with a healthcare professional to establish personalized targets and adjustments based on individual factors.
Nutritional Considerations

Fueling your body properly is crucial for any athlete, but especially for a fast-lane racer with diabetes. A well-structured meal plan tailored to the pre-race, during-race, and post-race periods is vital for maintaining stable blood sugar levels and optimal performance. Understanding the impact of different carbohydrate sources, protein, and fat, along with electrolyte needs, will help you navigate the unique challenges of managing diabetes during intense athletic competition.Effective fueling strategies are not just about eating; they’re about optimizing nutrient intake to support training, recovery, and peak performance.
By understanding the interplay between nutrition and blood sugar management, racers can significantly improve their chances of success while maintaining their health.
Sample Meal Plan for a Fast Lane Racer with Diabetes
A personalized meal plan should be developed in consultation with a registered dietitian or certified diabetes educator. The following is a sample meal plan, emphasizing balanced macronutrients and portion control, but remember, individual needs vary.
- Pre-Race (2-3 hours before): A complex carbohydrate source like brown rice or quinoa paired with lean protein (chicken breast or fish) and a healthy fat source (avocado or nuts) provides sustained energy release without causing a significant blood sugar spike. Example: Quinoa bowl with grilled chicken and avocado slices.
- During-Race (every 1-2 hours): Small, frequent carbohydrate snacks are essential to maintain blood sugar levels. Choose easily digestible carbohydrates like glucose gels or sports drinks. Example: A glucose gel and a few sips of sports drink.
- Post-Race (immediately after): Refuel with a combination of carbohydrates and protein to replenish glycogen stores and aid in muscle repair. Example: A protein shake with fruit and a small portion of whole-grain toast.
Carbohydrate Sources and Impact on Blood Sugar, Fast lane racing with diabetes
Different carbohydrates have varying effects on blood sugar levels. Understanding these differences is key to managing blood sugar fluctuations.
| Carbohydrate Source | Glycemic Index (GI) | Impact on Blood Sugar |
|---|---|---|
| White bread | High (70-100) | Rapid increase in blood sugar |
| Brown rice | Medium (50-70) | Moderate increase in blood sugar |
| Oatmeal | Medium (50-70) | Moderate increase in blood sugar |
| Fruits (apple) | Medium (50-70) | Moderate increase in blood sugar |
| Glucose gels | High (80-100) | Rapid increase in blood sugar |
Note: The Glycemic Index (GI) is a ranking of carbohydrates based on their effect on blood glucose levels.
Protein and Fat Intake for Blood Sugar Stability
Protein and healthy fats play crucial roles in stabilizing blood sugar. They help slow down the absorption of carbohydrates, preventing rapid spikes and crashes. Incorporating adequate amounts of protein and healthy fats into meals and snacks is essential for maintaining blood sugar balance during racing. Example: A post-race meal of grilled fish with brown rice and a side salad with olive oil dressing.
Fueling Strategies for Training and Recovery
Fueling strategies for training and recovery should be aligned with the intensity and duration of the workout. Consistent carbohydrate intake throughout training sessions prevents blood sugar dips and fatigue. Adequate recovery nutrition helps replenish glycogen stores and supports muscle repair.
Electrolytes and Hydration
Electrolytes, like sodium, potassium, and magnesium, are vital for maintaining hydration and blood sugar balance during prolonged exercise. Sweating during intense exercise leads to electrolyte loss, which can negatively affect blood sugar regulation and overall performance. Replenishing electrolytes through sports drinks or electrolyte tablets is crucial for racers.
Technological Advancements: Fast Lane Racing With Diabetes
The landscape of diabetes management is constantly evolving, and technological advancements are profoundly impacting the lives of athletes, especially those competing in fast-lane racing. These innovations provide unprecedented tools for real-time monitoring, personalized adjustments, and optimized performance strategies, enabling racers to effectively manage their condition while striving for peak athleticism.Continuous glucose monitoring (CGM) systems, insulin delivery devices, and wearable technology are revolutionizing how racers with diabetes approach training and competition.
These tools offer a higher degree of precision and flexibility compared to traditional methods, enabling racers to maintain optimal blood glucose levels during intense periods of exertion and recovery.
Continuous Glucose Monitoring (CGM) Systems
CGM systems provide real-time glucose readings, allowing racers to proactively adjust their insulin doses and dietary intake. This continuous feedback loop is invaluable for preventing both hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) during high-intensity racing, crucial for maintaining optimal performance. These systems have evolved significantly, offering varying degrees of accuracy and convenience.
- Different Types of CGM Sensors: Some CGM sensors use a small, easily-applied sensor on the skin, collecting interstitial fluid samples for glucose readings. Others involve a more invasive subcutaneous infusion set, offering more reliable and consistent readings but with potential for localized discomfort. Each type offers unique advantages in terms of ease of use and accuracy.
- CGM Application in Racing: During races, CGM data can guide insulin adjustments and dietary strategies. For example, a racer experiencing a rapid rise in blood glucose could adjust their insulin dose or consume a carbohydrate-containing snack to prevent hyperglycemia. Conversely, a drop in blood sugar could trigger the consumption of a glucose-containing item. This proactive approach allows racers to maintain stable glucose levels, minimizing the risk of performance-affecting fluctuations.
The data can be analyzed in detail, allowing the racer and medical team to pinpoint the most effective strategies for optimal performance and well-being during and after the race.
Insulin Delivery Systems
Insulin delivery systems play a critical role in maintaining blood glucose control. Several types are available, each with distinct characteristics and advantages.
- Traditional Insulin Injections: While still a common method, traditional injections require manual calculations and adjustments, which can be challenging during a race. The speed of delivery and accuracy are affected by the racer’s ability to perform injections, especially during the stress of a race. Time-consuming and requires consistent effort.
- Insulin Pumps: Insulin pumps provide a continuous infusion of insulin, minimizing the need for manual injections. They offer a more automated and precise method of insulin delivery. These systems allow for basal insulin delivery (a constant flow) and bolus doses (additional insulin for meals or exercise), enabling greater flexibility and personalized control. Insulin pumps are becoming increasingly sophisticated, with features that automatically adjust insulin delivery based on real-time CGM data.
They are more complex than injections but can significantly improve blood glucose control during a race.
Wearable Technology
Wearable technology is expanding the possibilities for real-time monitoring of vital signs and blood sugar levels. Heart rate monitors, activity trackers, and advanced smartwatches can be combined with CGM systems to provide a comprehensive picture of physiological responses during a race.
- Real-Time Monitoring: This allows for rapid identification of changes in heart rate, exertion levels, and blood glucose levels, allowing racers to quickly adjust their strategies and make informed decisions during the race. Early detection of potential issues can be crucial in maintaining performance and avoiding complications.
Data Analysis and Optimization
Data analysis plays a vital role in optimizing insulin adjustments and performance strategies. CGM data can be analyzed to identify patterns and trends, allowing racers and healthcare providers to refine their management protocols.
- Personalized Strategies: This can lead to personalized strategies that are tailored to the individual racer’s physiological responses and training regimens, enabling optimal blood glucose control during and after racing events.
Accessibility and Affordability
Ensuring accessibility and affordability of these technologies is critical for broader implementation. The costs of CGM devices and insulin pumps can be significant, and efforts to improve affordability are vital to promote equitable access for all racers with diabetes.
Fast lane racing with diabetes requires meticulous management, and that’s just the tip of the iceberg. It’s a complex balancing act, similar to the challenges faced by those navigating a misdiagnosis – like how almost 20 percent of people with MS are misdiagnosed at first. This article highlights the importance of early and accurate diagnosis, a lesson that translates directly to the rigorous training and constant monitoring needed in fast lane racing with diabetes.
The dedication and precision required are truly remarkable.
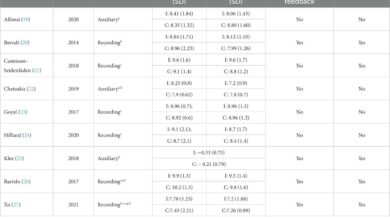
Comparison of CGM Devices
| Feature | Device A | Device B | Device C |
|---|---|---|---|
| Accuracy | High | High | Moderate |
| Ease of Use | Easy | Moderate | Difficult |
| Cost | High | Medium | Low |
| Battery Life | Good | Excellent | Poor |
Support Systems and Communities
Racing with diabetes requires more than just meticulous planning and precise execution; it demands a robust support network. A strong foundation of support empowers athletes to navigate the complexities of diabetes management while pushing their physical and mental limits. This network extends beyond medical professionals to encompass coaches, fellow racers, family, and friends, all playing crucial roles in the journey.A well-structured support system provides racers with the emotional and practical resources necessary to succeed.
This encompasses access to expert guidance, encouragement during challenging moments, and a sense of community that fosters shared experiences and mutual support. By fostering a culture of understanding and collaboration, we create a more inclusive and empowering environment for athletes managing diabetes.
Significance of Support Networks
A robust support network is paramount for racers with diabetes. It provides a safety net during challenging moments, offering encouragement and guidance. The shared experiences and advice within these networks can prove invaluable in navigating the complexities of diabetes management while training and competing. This fosters a sense of belonging and shared understanding, which is critical for maintaining motivation and well-being.
Role of Medical Professionals
Medical professionals play a pivotal role in supporting athletes with diabetes. They are instrumental in providing ongoing care, monitoring blood glucose levels, adjusting medication regimens, and addressing any complications that may arise. They act as a crucial resource, offering personalized guidance and expertise tailored to the specific needs of the racer. Furthermore, they provide valuable insights into the potential impact of exercise and competition on blood sugar control.
Working collaboratively with coaches and athletes, medical professionals ensure that the athlete’s health remains a priority.
Importance of Coaches
Coaches are critical in supporting racers with diabetes. They understand the demands of training and competition and can tailor training plans to accommodate the athlete’s specific needs, including blood glucose fluctuations and potential adjustments. A knowledgeable coach can also provide crucial insights into pacing strategies and recovery protocols that minimize the risk of hypoglycemia or hyperglycemia during competition.
Effective communication between coaches and medical professionals is essential to ensure the athlete’s safety and optimal performance.
Benefits of Online Communities
Online communities and forums provide a valuable platform for racers with diabetes to share experiences, advice, and support. These platforms facilitate a sense of community, allowing athletes to connect with others who understand the unique challenges of managing diabetes while pursuing athletic goals. Sharing strategies for managing blood sugar during training and races, and gaining insights from others facing similar situations, provides a supportive environment.
Online resources can also be a source of valuable information and encouragement.
Role of Family and Friends
Family and friends play a vital role in providing emotional and practical support. Their understanding and encouragement are crucial in navigating the challenges of managing diabetes while balancing personal and athletic commitments. Their presence offers a sense of stability and reassurance, particularly during periods of stress or uncertainty. Their support can be instrumental in ensuring that the athlete feels equipped and empowered to pursue their goals.
Education and Awareness in Racing Environments
Education and awareness regarding diabetes management are crucial in racing environments. This includes educating teammates, coaches, and support staff about the specific needs of athletes with diabetes. Clear communication and understanding are essential to ensure the safety and well-being of the athlete. Creating a supportive environment where everyone understands the challenges and potential risks associated with diabetes management fosters a more inclusive and empowering atmosphere for the racer.
Resources for Racers with Diabetes
| Category | Resources |
|---|---|
| Medical Professionals | Diabetologists, endocrinologists, sports medicine physicians |
| Support Groups | Local diabetes support groups, online forums, athlete-specific groups |
| Educational Materials | Diabetes management guides, educational websites, training resources |
Safety Precautions and Risks
Racing with diabetes requires meticulous planning and awareness of potential complications. This isn’t about fear-mongering, but about understanding the specific challenges and proactively mitigating risks. Successful racing, even with diabetes, hinges on a robust safety net built on thorough preparation and a rapid response system.Diabetes management during high-intensity activities like fast lane racing demands extra vigilance. Factors like fluctuating blood sugar levels, physical exertion, and environmental changes all contribute to the dynamic nature of the disease.
Proactive measures, from pre-race assessments to emergency protocols, are paramount.
Potential Complications of Diabetes Management
Fast-paced racing environments can exacerbate existing diabetic conditions or introduce new complications. Fluctuations in blood sugar levels, both high (hyperglycemia) and low (hypoglycemia), are the most significant concerns. These fluctuations can impact cognitive function, reaction time, and overall performance, increasing the risk of accidents. Dehydration, a common concern in high-intensity activities, can further compound these issues, making it even harder to maintain blood sugar control.
The risk of infection is also elevated when blood sugar levels are not well-managed, especially during prolonged exertion.
Importance of Pre-Race Medical Assessments
Thorough pre-race medical assessments are critical. These assessments should encompass a review of the racer’s current blood sugar control, medication regimen, and any recent health changes. Doctors should consider factors like the racer’s recent A1C levels, insulin sensitivity, and any past episodes of severe hypoglycemia or hyperglycemia. This information is vital for developing individualized emergency plans tailored to the racer’s specific needs.
The racer should also be well-versed in the use of glucose monitoring devices and have a clear understanding of the symptoms of both low and high blood sugar.
Emergency Plans
Emergency plans are not just documents; they are living strategies. They should Artikel specific actions to take in case of hypoglycemia or hyperglycemia. These plans should detail the racer’s medication protocol, procedures for rapid glucose monitoring, and the contact information for support personnel. Crucially, the racer must communicate these plans clearly to their support team and medical personnel.
Practicing the emergency plan beforehand, even in a non-race environment, can significantly improve the chances of a successful outcome.
Risk Factors Associated with Hypoglycemia and Hyperglycemia
Hypoglycemia, or low blood sugar, can occur during or after a race due to the exertion’s impact on insulin requirements. Prolonged exertion without adequate glucose intake can trigger hypoglycemia. Hyperglycemia, or high blood sugar, can occur if the racer’s insulin dosage is insufficient or if they consume excessive carbohydrates. The combination of intense exertion and uncontrolled blood sugar can lead to dehydration and further complications.
Methods to Prevent Low Blood Sugar Events and High Blood Sugar Spikes
Maintaining stable blood sugar levels is crucial. This requires a combination of meticulous pre-race preparation and on-the-spot adjustments. The racer should consume a pre-race meal or snack with a controlled amount of carbohydrates to avoid a sharp blood sugar spike or dip. During the race, frequent blood sugar checks and adjustments to insulin dosages, if necessary, are crucial.
Consuming easily digestible carbohydrates during periods of low blood sugar is a crucial component of emergency preparedness.
Importance of Communication
Effective communication between the racer, medical personnel, and support staff is paramount. The racer should clearly communicate their medical needs and emergency plans to the support team and medical professionals. The support team should be well-versed in the racer’s medical condition and able to respond effectively in case of an emergency. Clear communication protocols and pre-determined signals should be established.
Emergency Procedures and Contact Information
| Emergency Situation | Procedure | Contact Information |
|---|---|---|
| Hypoglycemia | Administer fast-acting glucose; monitor blood sugar; contact medical personnel. | Emergency Contact 1: [Name], [Phone Number]; Emergency Contact 2: [Name], [Phone Number] |
| Hyperglycemia | Adjust insulin dosage; monitor blood sugar; contact medical personnel. | Doctor’s Name: [Name], [Phone Number]; Hospital: [Name], [Phone Number] |
| Other Medical Concerns | Follow established emergency plan; contact medical personnel immediately. | Medical Support Team Leader: [Name], [Phone Number]; Team Contact Person: [Name], [Phone Number] |
Closing Summary
Ultimately, fast lane racing with diabetes requires a multifaceted approach combining meticulous planning, proactive management, and a strong support system. This guide provides a framework for racers to optimize their performance, manage their blood sugar levels, and ultimately thrive in the demanding world of high-performance racing. By understanding the unique challenges and utilizing effective strategies, racers can pursue their goals while prioritizing their health and well-being.