First ever guidelines safe exercising type 1 diabetes provide a comprehensive resource for individuals navigating the complexities of physical activity. This guide delves into the critical importance of exercise for overall well-being, while highlighting the specific considerations for those with type 1 diabetes. Understanding the potential risks and benefits of different exercises is paramount, and this guide will equip you with the knowledge to safely integrate exercise into your daily routine.
The guidelines cover a range of crucial aspects, from understanding blood sugar fluctuations during exercise to developing personalized exercise plans and implementing safety measures. This is more than just a set of rules; it’s a roadmap to empower individuals to achieve their fitness goals while effectively managing their condition.
Introduction to Safe Exercising for Type 1 Diabetes
Staying active is crucial for overall health, and this is especially true for individuals with type 1 diabetes. Regular exercise helps manage blood sugar levels, improves cardiovascular health, and boosts mood. However, exercising with type 1 diabetes comes with unique considerations. Understanding the potential risks and adopting appropriate strategies is vital for a safe and effective workout routine.Proper guidance and knowledge are essential for individuals with type 1 diabetes to exercise safely.
Without careful monitoring and adjustments to their insulin regimen, blood glucose levels can fluctuate significantly during and after exercise, potentially leading to hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar). This can have serious health consequences. A personalized approach to exercise, tailored to the individual’s specific needs and medical condition, is critical.
Importance of Exercise for Type 1 Diabetes
Exercise plays a multifaceted role in managing type 1 diabetes. It enhances insulin sensitivity, meaning the body utilizes insulin more effectively. This, in turn, helps regulate blood sugar levels. Furthermore, regular physical activity promotes weight management, which is important for blood sugar control. Cardiovascular health benefits also contribute to overall well-being.
Regular exercise has been shown to reduce the risk of heart disease, a significant concern for individuals with diabetes.
Just saw the first-ever guidelines for safe exercising with type 1 diabetes, which is super helpful! It’s amazing how much focus is now on preventative care for chronic conditions. Speaking of innovative health monitoring, a new app, new app monitors the health of pregnant women , is making waves in providing personalized support during pregnancy. This new technology is definitely inspiring and I’m excited to see how it helps improve outcomes.
Back to the diabetes guidelines, though – these are a real game-changer for managing the condition proactively.
Potential Risks of Exercising Without Proper Guidance
Improper exercise management can lead to various complications. Uncontrolled blood sugar fluctuations, including hypoglycemia and hyperglycemia, can arise without adjusting insulin doses or carbohydrate intake. This can lead to symptoms ranging from dizziness and weakness to severe complications like seizures or loss of consciousness. Furthermore, individuals with type 1 diabetes might not experience the typical warning signs of low blood sugar, increasing the risk of serious episodes.
Evolution of Exercise Recommendations
Historically, exercise recommendations for people with type 1 diabetes have evolved from general guidelines to more individualized strategies. Early approaches focused on general exercise principles without specific considerations for blood glucose management. Over time, the understanding of how exercise impacts blood sugar levels has deepened, leading to more precise recommendations for insulin adjustments and carbohydrate intake. Modern recommendations emphasize personalized plans based on individual blood glucose patterns and exercise routines.
Impact of Different Exercise Types on Blood Sugar
Understanding how different types of exercise affect blood sugar levels is crucial for developing a safe and effective exercise routine.
| Exercise Type | Potential Impact on Blood Sugar | Considerations |
|---|---|---|
| Cardiovascular Exercise (e.g., running, swimming, cycling) | Can lead to temporary drops in blood sugar, especially if performed at high intensity or long duration. Can also increase insulin sensitivity in the long term. | Careful monitoring before, during, and after exercise is essential. Adjust insulin doses or carbohydrate intake as needed. |
| Strength Training (e.g., weightlifting, resistance bands) | Can lead to minor increases in blood sugar, particularly in the hours following the workout. However, strength training improves overall insulin sensitivity over time. | Similar to cardiovascular exercise, monitoring is important. Consider insulin adjustments based on individual responses. |
| Flexibility Exercises (e.g., stretching, yoga) | Generally has minimal impact on blood sugar levels, but individual responses may vary. | Focus on maintaining a consistent routine. |
Understanding Blood Sugar Fluctuations During Exercise
Exercise is crucial for overall health, but for individuals with type 1 diabetes, it can significantly impact blood glucose levels. Understanding the physiological mechanisms behind these changes is essential for managing blood sugar effectively and preventing complications. This section delves into how exercise affects blood sugar, offering insights into the factors influencing fluctuations and providing practical guidance.
Physiological Mechanisms of Blood Sugar Changes
During exercise, the body’s energy demands increase. To meet these demands, the body utilizes stored glucose from the liver and muscles. Simultaneously, exercise can influence insulin sensitivity, affecting how efficiently the body uses glucose. These factors, combined with the body’s natural hormonal responses, can result in a complex interplay of blood sugar changes.
Effect of Exercise on Insulin Sensitivity and Glucose Uptake
Exercise typically increases insulin sensitivity, meaning cells become more responsive to insulin, facilitating glucose uptake. This enhanced uptake can lead to a decrease in blood glucose levels. However, the extent of this effect depends on various factors, including the type, intensity, and duration of the exercise. For example, moderate-intensity activities often lead to greater insulin sensitivity compared to high-intensity efforts.
The duration of exercise also plays a role; prolonged exercise may further increase insulin sensitivity.
Blood Sugar Responses to Different Exercise Intensities and Durations
The blood sugar response to exercise varies significantly based on intensity and duration. High-intensity workouts can cause a temporary rise in blood glucose levels due to the release of stress hormones. Conversely, moderate-intensity exercise often leads to a decrease in blood glucose. Prolonged exercise, especially if it is of moderate intensity, can result in a sustained decrease in blood sugar levels.
The body’s ability to use glucose for energy becomes more efficient during exercise.
Table of Common Blood Sugar Responses During Exercise
The following table provides a general overview of common blood sugar responses during exercise for individuals with type 1 diabetes. Note that these are general guidelines, and individual responses may vary significantly. Consulting with a healthcare professional is crucial for personalized recommendations.
Ever wonder about safe exercise routines for Type 1 diabetes? Well, the first ever guidelines are finally here, providing a solid foundation for healthy activity. Meanwhile, the recent Olympic figure skating scandal involving a banned drug highlights the importance of ethical sports practices. Understanding the implications of performance-enhancing substances, like those discussed in this article , really puts the new Type 1 diabetes exercise guidelines into perspective.
Ultimately, these guidelines offer crucial tools for safe and effective workouts for those managing this condition.
| Individual | Pre-Exercise Blood Sugar (mg/dL) | Type of Exercise | Exercise Duration (minutes) | Expected Blood Sugar Response |
|---|---|---|---|---|
| Person A | 180 | Walking | 30 | Slight decrease |
| Person B | 120 | Running | 60 | Potential decrease, monitor closely |
| Person C | 250 | Cycling | 90 | Potential rise initially, then gradual decrease |
Factors Influencing Blood Sugar Fluctuations
Several factors can influence blood sugar fluctuations during exercise, including pre-exercise blood sugar levels, type of exercise, and medication dosages. A higher pre-exercise blood sugar level may increase the risk of a post-exercise rise. Different types of exercise (e.g., intense weightlifting versus leisurely swimming) will have different effects. Furthermore, the timing and dosage of insulin can affect blood glucose responses.
Individual responses are highly variable, highlighting the need for careful monitoring and adjustments in exercise plans.
Developing a Personalized Exercise Plan
Creating a safe and effective exercise plan is crucial for individuals with type 1 diabetes. This plan should be tailored to the individual’s specific needs, including their current blood sugar control, chosen activities, and insulin regimen. A well-structured plan will help manage blood sugar fluctuations, preventing both hypoglycemia and hyperglycemia, while promoting overall health and fitness.A personalized exercise plan isn’t a one-size-fits-all approach.
It requires careful consideration of several factors and regular adjustments based on individual responses. This process ensures that exercise becomes a safe and beneficial part of managing diabetes, rather than a source of concern.
Pre-Exercise Blood Sugar Checks, First ever guidelines safe exercising type 1 diabetes
Understanding blood sugar levels before exercise is paramount. Pre-exercise blood sugar checks are essential to determine the starting point and ensure that levels are within a safe range. This crucial step helps prevent potential complications during and after exercise. Generally, a target blood glucose range of 100-180 mg/dL is recommended before exercise. Lower levels may increase the risk of hypoglycemia, while higher levels may lead to hyperglycemia.
Post-Exercise Blood Sugar Monitoring
Monitoring blood sugar levels after exercise is equally vital. Post-exercise monitoring allows for assessment of how the body responds to physical activity. This information helps tailor future exercise plans and insulin adjustments. Blood sugar levels can fluctuate significantly after exercise, sometimes dropping dramatically or rising unexpectedly. Careful observation of post-exercise blood sugar patterns is critical for personalized management.
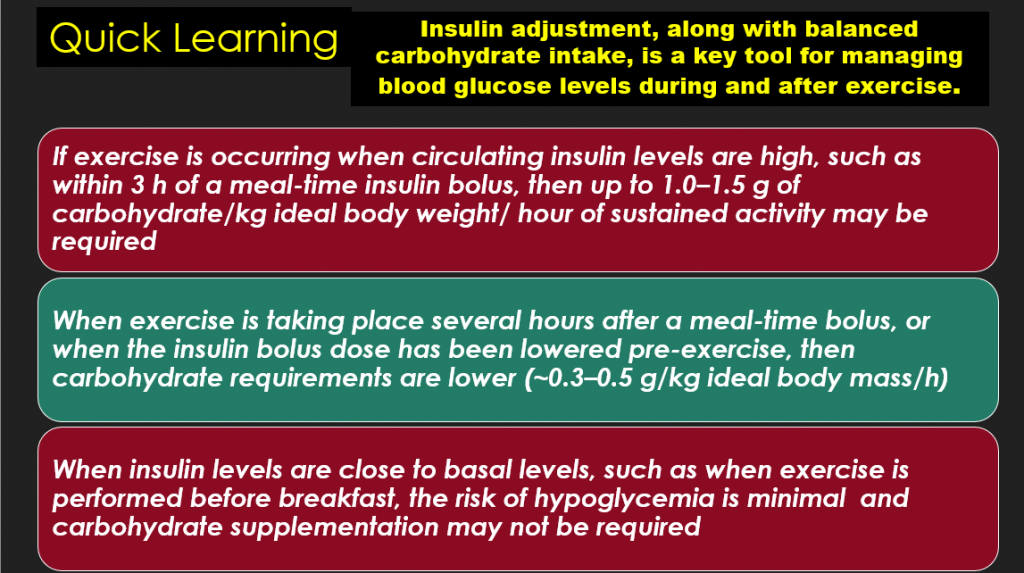
Carbohydrate Intake
Carbohydrate intake plays a critical role in managing blood sugar during and after exercise. Adjusting carbohydrate intake before, during, and after exercise is essential to maintain healthy blood glucose levels. Pre-exercise carbohydrates provide fuel for the workout, while during-exercise carbohydrates may be needed to prevent hypoglycemia. Post-exercise carbohydrates replenish glycogen stores and support recovery. The amount of carbohydrates needed will vary based on the intensity and duration of exercise, individual insulin sensitivity, and current blood glucose levels.
Insulin Dose Adjustments
Adjusting insulin doses before, during, and after exercise is crucial for managing blood sugar. Exercise can affect insulin sensitivity, leading to unexpected blood sugar fluctuations. Careful consideration of exercise intensity, duration, and individual response is critical when adjusting insulin doses. Decreased insulin requirements are often necessary before, during, and after exercise, depending on the individual’s needs.
Preventing and Managing Hypoglycemia and Hyperglycemia
Hypoglycemia and hyperglycemia are potential complications during exercise. Recognizing and responding promptly to these conditions is essential. Strategies to prevent hypoglycemia include pre-exercise carbohydrate intake, reduced insulin doses, and close monitoring of blood sugar levels. Strategies to prevent hyperglycemia include adjustments in insulin doses and careful carbohydrate management. Regular monitoring and communication with a healthcare provider are key to managing these potential complications effectively.
Sample Exercise Plan
| Activity | Time (minutes) | Pre-Exercise Blood Sugar (mg/dL) | Insulin Adjustment | Carbohydrate Intake (grams) | Post-Exercise Blood Sugar (mg/dL) |
|---|---|---|---|---|---|
| Brisk Walking | 30 | 120 | Reduce insulin dose by 1 unit | 15 | 105 |
| Cycling | 45 | 150 | Reduce insulin dose by 2 units | 20 | 140 |
| Swimming | 60 | 160 | Reduce insulin dose by 1.5 units | 25 | 170 |
This table provides a sample exercise plan. It’s crucial to remember that these are just examples, and individual needs may vary significantly. Always consult with a healthcare professional to develop a personalized plan tailored to your specific situation. Individual adjustments based on blood sugar responses and individual sensitivity are vital.
Safety Measures and Considerations
Staying safe while exercising with type 1 diabetes requires proactive planning and awareness. Understanding potential complications and having a robust safety net are crucial for enjoying physical activity without jeopardizing your health. This section Artikels essential safety measures and considerations to help you navigate your exercise routine with confidence and peace of mind.Proper preparation and awareness are key to managing blood sugar fluctuations during exercise.
The first-ever guidelines for safe exercising with type 1 diabetes are a game-changer, offering a structured approach to physical activity. It’s inspiring to see how this new resource can empower people with the condition. Similarly, stories like the one of the woman who decided to stop covering her vitiligo and join an awareness effort woman decides to stop covering vitiligo joins awareness effort demonstrate the power of embracing one’s identity and promoting understanding.
These positive steps, both in the medical and personal spheres, highlight the importance of inclusivity and self-acceptance, ultimately enriching the well-being of individuals with type 1 diabetes.
By understanding the risks and implementing safety precautions, you can prevent serious complications and enjoy the many benefits of physical activity.
Crucial Safety Precautions
A comprehensive approach to exercise safety includes several crucial precautions. Adherence to these precautions minimizes the risk of adverse events associated with diabetes management during physical activity.
- Regular Blood Glucose Monitoring: Consistent blood glucose monitoring before, during, and after exercise is paramount. This allows you to track your blood sugar levels and adjust your insulin regimen as needed, ensuring you maintain optimal glucose control.
- Proper Hydration: Dehydration can exacerbate blood sugar fluctuations. Staying well-hydrated before, during, and after exercise is vital for maintaining overall health and preventing potential complications.
- Choosing the Right Exercise Intensity and Duration: Starting slowly and gradually increasing the intensity and duration of your workouts is essential. This allows your body to adapt and minimizes the risk of extreme blood sugar changes.
- Avoiding Exercise During Peak Blood Sugar Fluctuation Times: Recognizing the periods when blood sugar is most likely to fluctuate can help you schedule exercise accordingly. For example, avoiding exercise during times of high stress or when you’ve consumed a large meal can prevent significant fluctuations.
Importance of Wearing Proper Identification
Wearing proper identification is critical in case of an emergency. This ensures that medical personnel can readily identify your condition and provide appropriate treatment.
- Medical Alert Bracelet or Necklace: A medical alert bracelet or necklace clearly stating your diagnosis of type 1 diabetes is a valuable tool. It helps medical professionals quickly recognize your condition and administer necessary care in case of an emergency.
Carrying Fast-Acting Carbohydrates
Carrying glucose tablets or other fast-acting carbohydrates is crucial for managing hypoglycemic episodes during exercise.
- Fast-Acting Carbohydrates: Having glucose tablets, fruit juice, or other fast-acting carbohydrates on hand allows you to quickly raise your blood sugar if it drops too low.
Recognizing and Responding to Hypo/Hyperglycemic Episodes
Recognizing and responding promptly to both hypoglycemic and hyperglycemic episodes is critical for safety.
- Hypoglycemia Symptoms: Recognizing the symptoms of hypoglycemia (e.g., shakiness, sweating, dizziness, confusion) is essential. If these symptoms occur, immediately consume fast-acting carbohydrates to raise your blood sugar.
- Hyperglycemia Symptoms: Recognizing the symptoms of hyperglycemia (e.g., excessive thirst, frequent urination, blurred vision) is equally important. If these symptoms arise, discontinue exercise, contact your doctor, and monitor your blood sugar closely.
Importance of Having a Support System
A strong support system is essential for navigating the complexities of managing type 1 diabetes during exercise.
- Support from Friends and Family: Informing friends and family about your exercise routine and potential complications can provide invaluable support and assistance during exercise.
- Professional Guidance: Regular consultation with your healthcare team is essential for developing a personalized exercise plan and addressing any concerns.
Emergency Contacts and Procedures
Having a readily available list of emergency contacts and procedures is critical in case of a severe hypoglycemic or hyperglycemic event.
| Emergency Contact | Relationship | Phone Number | Procedure |
|---|---|---|---|
| Dr. [Doctor’s Name] | Physician | [Phone Number] | Call immediately if experiencing severe hypo/hyperglycemia. |
| [Emergency Contact Name] | Family Member/Friend | [Phone Number] | Contact for immediate support and assistance. |
| [Local Hospital] | Hospital | [Phone Number] | Call in case of severe hypo/hyperglycemia requiring immediate medical attention. |
Illustrative Case Studies
Putting knowledge into practice is key to managing type 1 diabetes effectively. This section delves into real-life scenarios, showcasing successful exercise strategies and highlighting the importance of personalized plans. We’ll explore the challenges and triumphs experienced by individuals with type 1 diabetes as they navigate the world of safe exercise.Understanding how blood sugar fluctuates during exercise and how to adjust insulin doses accordingly is crucial.
Each individual’s response to exercise is unique, so personalized plans are vital for optimizing outcomes.
Safe Exercise Plan for Sarah
Sarah, a 28-year-old woman with type 1 diabetes, has been consistently exercising for six months. She’s committed to a safe and effective routine. Her exercise plan includes a mix of cardio and strength training, adjusted based on her blood glucose levels. She meticulously monitors her blood sugar before, during, and after exercise.
- Exercise Routine: Sarah starts her day with a 30-minute brisk walk, followed by 30 minutes of strength training (using light weights). She adjusts her insulin dosage based on pre-exercise blood glucose levels. Her plan includes regular breaks and adequate hydration throughout her workout. She always carries glucose tablets for low blood sugar emergencies.
- Blood Sugar Management: Sarah monitors her blood glucose levels before, during, and after each workout. If her pre-exercise blood glucose is below 100 mg/dL, she consumes a small carbohydrate snack (15-20g) before starting her exercise. Post-exercise, if her blood glucose drops too low, she takes glucose tablets to prevent hypoglycemia. She adjusts her insulin dosage as per the guidance of her doctor and diabetes educator.
Challenges and Successes in Exercising Safely
Exercising safely with type 1 diabetes presents several challenges. These include unpredictable blood sugar fluctuations, the need for meticulous monitoring, and the potential for hypoglycemia or hyperglycemia. However, successful strategies and consistent adherence to a personalized plan can overcome these hurdles. The successes often include improved blood glucose control, increased energy levels, and enhanced overall well-being.
- Challenge: Predicting how exercise will impact blood sugar levels can be tricky. This often requires adjustments to the exercise plan, including insulin dose changes and dietary adjustments.
- Success: With experience and monitoring, individuals learn to recognize patterns in their blood sugar responses to different types and intensities of exercise.
Personalized Exercise Plans: A Case Study
This case study highlights the importance of a personalized approach to exercise. A 16-year-old boy, David, initially struggled to maintain a consistent exercise routine. He experienced frequent blood sugar fluctuations and hypoglycemia episodes. After working with a certified diabetes educator, he developed a personalized plan that addressed his specific needs and preferences.
- Initial Challenges: David’s initial plan was not tailored to his individual response to exercise. This resulted in inconsistent blood sugar control and reduced motivation.
- Personalized Plan: His new plan incorporates activities he enjoys, like swimming and cycling. It also includes specific carbohydrate intake strategies and insulin adjustments based on his pre-exercise blood sugar readings.
- Outcomes: David now experiences improved blood glucose control and increased physical activity. His confidence and self-management skills have significantly improved.
Different Exercise Routines
Several successful exercise routines exist for individuals with type 1 diabetes. The key is to find activities that are enjoyable and sustainable. These may include:
- Yoga and Pilates: These low-impact activities can be easily adapted to accommodate varying blood sugar levels.
- Swimming: Swimming is a great cardiovascular workout with minimal impact on blood sugar.
- Cycling: Cycling offers a good cardiovascular workout and can be adapted to different levels of intensity.
- Walking: A simple and accessible form of exercise, walking can be incorporated into daily routines.
Summary of Case Studies
| Case Study | Individual Characteristics | Exercise Plan | Challenges | Successes |
|---|---|---|---|---|
| Sarah | 28-year-old woman, consistent exerciser | Cardio and strength training | Unpredictable blood sugar fluctuations | Improved blood glucose control, increased energy levels |
| David | 16-year-old boy, initial struggles | Personalized plan with swimming and cycling | Inconsistent blood sugar control, hypoglycemia | Improved blood glucose control, increased physical activity, improved confidence |
Monitoring and Evaluation
Staying on top of your exercise routine is crucial for managing type 1 diabetes effectively. A personalized plan isn’t a one-and-done deal. Regular monitoring and evaluation are essential for understanding how your body responds to exercise, identifying areas needing adjustment, and ensuring you’re achieving your fitness goals while keeping your blood sugar levels stable.Consistent monitoring allows you to track your progress, identify patterns, and make informed decisions about your exercise regimen.
This proactive approach empowers you to fine-tune your plan, maximizing its effectiveness and minimizing risks associated with blood sugar fluctuations.
Importance of Ongoing Monitoring
Regular monitoring of your blood glucose levels before, during, and after exercise is paramount. This data is invaluable in understanding how your body reacts to physical activity and how your chosen exercise affects your blood sugar. By tracking these levels, you can adjust your insulin regimen, carbohydrate intake, or exercise intensity as needed. This proactive approach helps you avoid potential complications and ensures that your exercise routine supports, rather than hinders, your overall health.
Methods for Tracking Progress
A structured approach to tracking progress is vital. Keeping a detailed logbook is an effective method. Record your exercise duration, intensity, type of activity, and blood glucose levels before, during, and after each session. Note any symptoms experienced, such as shakiness or dizziness. This comprehensive record allows for the identification of trends and patterns, helping you recognize potential issues.
Utilizing a dedicated mobile app or software designed for diabetes management can further streamline this process, providing you with visual representations of your data and facilitating analysis.
Adjusting the Exercise Plan
Adapting your exercise plan is a dynamic process. If you notice a consistent pattern of high blood sugar after certain types of exercise, you may need to adjust the timing of your insulin dose or the amount of carbohydrates consumed before or during your workout. Similarly, if you experience low blood sugar during or after exercise, you may need to alter your carbohydrate intake or insulin dose.
This iterative process, informed by your monitoring data, allows for a tailored approach to your exercise regimen.
Successful Strategies for Adapting an Exercise Plan
Adapting your exercise plan should be approached with a focus on understanding your body’s unique responses. One successful strategy involves incorporating short bursts of high-intensity interval training (HIIT) into your routine. By meticulously tracking your blood glucose levels, you can fine-tune the intensity and duration of HIIT sessions, ensuring a positive impact on your health without adverse effects on your blood sugar.
Another example is incorporating rest days into your schedule. This proactive approach helps your body recover and prevents overexertion, minimizing the risk of complications. Proper rest periods can contribute to improved blood sugar control.
Monitoring Tools and Techniques
The effectiveness of an exercise plan can be assessed using a variety of tools and techniques. This table provides a summary of various monitoring methods and their applications.
| Monitoring Tool/Technique | Description | Application |
|---|---|---|
| Blood Glucose Monitoring | Regularly measuring blood glucose levels before, during, and after exercise | Assessing immediate and long-term effects of exercise on blood sugar |
| Exercise Log | Detailed record of exercise sessions, including duration, intensity, type, and blood glucose levels | Identifying patterns and trends in blood sugar responses to different exercises |
| Mobile Health Apps | Apps designed for diabetes management, often incorporating exercise tracking and blood glucose logging | Streamlining the data collection and analysis process, providing visual representations of trends |
| Continuous Glucose Monitoring (CGM) | Real-time monitoring of blood glucose levels | Provides a comprehensive view of blood glucose fluctuations during and after exercise, enabling quick adjustments to exercise or insulin regimen |
Wrap-Up: First Ever Guidelines Safe Exercising Type 1 Diabetes
In conclusion, these first ever guidelines offer a practical and empowering approach to exercise for individuals with type 1 diabetes. By understanding the interplay between exercise, blood sugar management, and personalized plans, you can safely and effectively incorporate physical activity into your life. Remember, consistency and careful monitoring are key to success. This guide serves as a valuable resource for navigating the journey towards a healthier and more active lifestyle.





