Fungi role in crohns disease is a fascinating and complex area of research. The human gut is teeming with microorganisms, and fungi play a part in maintaining a healthy balance. But what happens when the balance shifts? This exploration delves into the intricate relationship between fungal overgrowth and the development of Crohn’s disease, examining the potential mechanisms, diagnostic methods, and therapeutic approaches.
We’ll explore the types of fungi commonly found in the gut microbiome, how dysbiosis might connect to Crohn’s, and current understanding of fungal overgrowth in Crohn’s patients. A critical look at the potential role of fungi in the inflammatory response will be presented.
This exploration will consider the specific fungal species and metabolites involved, and how they may trigger inflammatory responses in the gut. Different diagnostic techniques for detecting fungal overgrowth in Crohn’s patients will be detailed, including their advantages and disadvantages. Further, we’ll delve into existing antifungal therapies, their potential role in Crohn’s treatment, and potential challenges and limitations. A comprehensive look at future research directions, promising areas for study, and unanswered questions will complete the discussion.
Ultimately, this exploration aims to shed light on the intricate interplay between fungi and Crohn’s disease.
Fungi and Crohn’s Disease
The human gut harbors a complex ecosystem of microorganisms, including bacteria, archaea, viruses, and fungi. Fungi play a significant role in this ecosystem, contributing to both the normal functioning of the gut and potentially contributing to disease states. While some fungi are beneficial, others can cause issues, particularly in the context of inflammatory bowel diseases like Crohn’s disease.Fungi in the human gut, while often overlooked, are a critical component of the gut microbiome.
Their presence can impact digestion, immune responses, and overall health. An imbalance in the gut microbiome, known as dysbiosis, is increasingly recognized as a potential contributor to the development and progression of Crohn’s disease. Understanding the specific roles of fungi in this complex interplay is crucial for developing targeted therapeutic strategies.
Recent research suggests fungi might play a surprising role in Crohn’s disease, a condition impacting the digestive system. This fascinating area of study could lead to new treatments and a better understanding of the disease. Meanwhile, a new nonprofit dedicated to promoting diversity in diabetes research is making a significant impact, and it’s inspiring to see similar initiatives in other areas of health like new nonprofit to nurture diversity in diabetes did.
Hopefully, this kind of proactive approach to healthcare diversity will also be applied to understanding the complex relationship between fungi and Crohn’s disease.
Common Gut Fungi
The human gut microbiome contains a diverse range of fungal species. Some of the most prevalent fungi in the healthy gut include
- Candida albicans*,
- Saccharomyces cerevisiae*,
- Malassezia* species, and
- Aspergillus* species. These fungi typically exist in low numbers and are usually kept in check by the other components of the gut microbiome. Their presence is generally not considered harmful.
Dysbiosis and Crohn’s Disease
Dysbiosis, characterized by an imbalance in the gut microbiome composition, is strongly implicated in the development of Crohn’s disease. This imbalance can be caused by various factors, including antibiotic use, dietary changes, and genetic predisposition. In the context of Crohn’s disease, a shift in the relative abundance of fungal species towards potentially pathogenic strains, along with decreased populations of beneficial bacteria, may disrupt the normal immune response and contribute to chronic inflammation.
Fungal Overgrowth in Crohn’s Disease
Studies suggest that fungal overgrowth, specifically an increase in the abundance of certain fungi, is associated with Crohn’s disease. This overgrowth may be a consequence of the dysbiosis or a contributing factor. The exact mechanisms by which fungi contribute to the pathogenesis of Crohn’s disease are still under investigation, but it is believed that they may trigger an excessive inflammatory response, impacting the balance between the immune system and the gut microbiota.
Increased levels of fungi like
- Candida* and
- Aspergillus* have been observed in the intestinal tissues of Crohn’s patients.
Comparison of Gut Fungal Flora
| Fungi Type | Normal Gut | Crohn’s Disease | Description |
|---|---|---|---|
| *Candida albicans* | Present in low numbers | Potentially increased abundance | A common yeast-like fungus; can cause opportunistic infections in immunocompromised individuals. |
| *Saccharomyces cerevisiae* | Present in low numbers | Potentially increased abundance | A type of yeast, often found in food products; its role in Crohn’s is still being studied. |
| *Malassezia* species | Present in low numbers | Potentially increased abundance | A group of lipid-metabolizing fungi; their involvement in Crohn’s disease is a focus of research. |
| *Aspergillus* species | Present in low numbers | Potentially increased abundance | A group of filamentous fungi; implicated in allergic reactions and potentially inflammatory responses. |
Fungal Mechanisms in Crohn’s Disease: Fungi Role In Crohns Disease
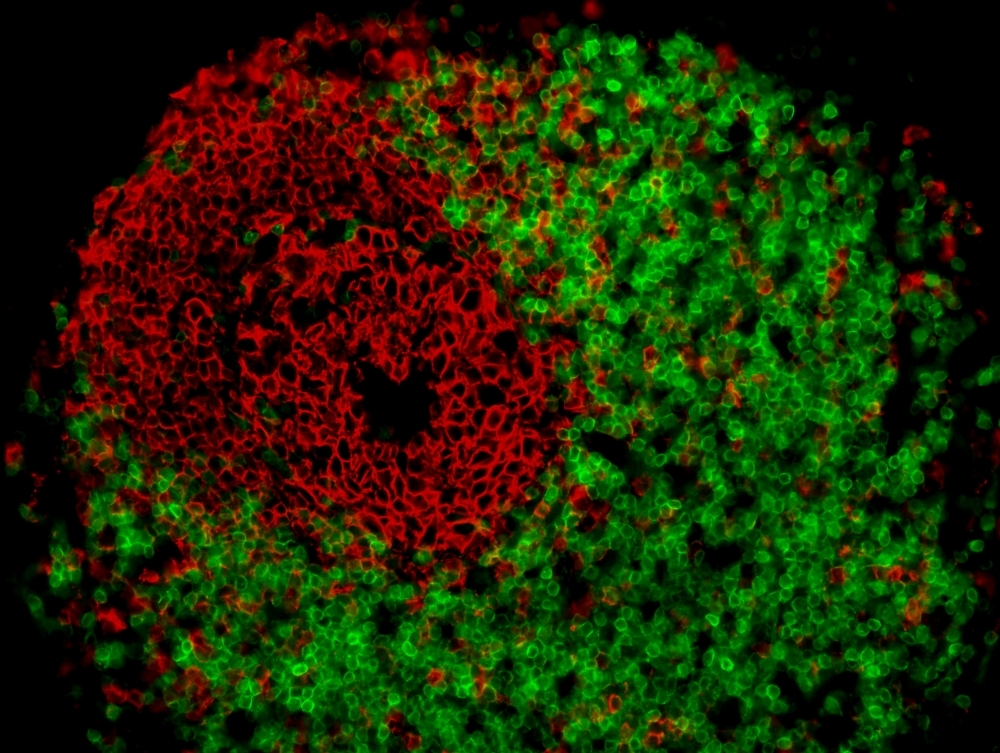
Fungi are increasingly recognized as potential contributors to the complex pathogenesis of Crohn’s disease. While the precise role of fungi in this inflammatory bowel disease remains an area of active research, evidence suggests a multifaceted interaction between specific fungal species, the host immune system, and the gut environment. This intricate interplay can influence the development and progression of Crohn’s disease, leading to a deeper understanding of the disease’s mechanisms.Fungal species can reside in the gut, potentially triggering immune responses that exacerbate inflammation.
The specific mechanisms by which fungi contribute to Crohn’s disease pathogenesis involve various factors, including immune responses, fungal metabolites, and the presence of specific virulence factors. These interactions, though not fully understood, suggest that fungi are not mere bystanders in the gut but active participants in the disease process.
Potential Mechanisms of Fungal Contribution
Fungal species residing in the gut can trigger immune responses that either resolve or exacerbate inflammation. This response varies significantly depending on the individual’s genetic predisposition and the specific fungal species involved. For example, certain fungal species, like
Candida albicans*, are more commonly associated with gut dysbiosis and subsequent inflammation.
Inflammatory Responses Triggered by Specific Fungal Species
Different fungal species elicit varying inflammatory responses. For example,
- Aspergillus fumigatus*, a common airborne fungus, can trigger allergic reactions in susceptible individuals, potentially contributing to chronic inflammation in the gut. The inflammatory response to
- Candida* species is often characterized by an initial Th17-biased response, but this can shift to a Th1 or Th2 response, depending on the context and individual. These complex responses can lead to chronic inflammation, which could be a factor in the development of Crohn’s disease.
Immune Responses to Fungi in Healthy vs. Crohn’s Patients
The immune responses to fungal species differ significantly between healthy individuals and Crohn’s patients. Healthy individuals typically mount a balanced immune response, effectively controlling fungal overgrowth and preventing excessive inflammation. In contrast, Crohn’s patients often exhibit an impaired or dysregulated immune response, leading to uncontrolled fungal growth and persistent inflammation. This suggests that the dysregulation of immune pathways in Crohn’s patients may contribute to fungal overgrowth.
Role of Fungal Metabolites in Gut Inflammation
Fungal metabolites can influence the gut environment and contribute to inflammation. For example, certain fungal metabolites can disrupt the delicate balance of the gut microbiota, potentially leading to an overgrowth of pathogenic bacteria or dysbiosis. These metabolites can also directly stimulate immune cells, leading to inflammatory responses. Further research is needed to understand the specific metabolites involved and their precise mechanisms of action.
Fungal Virulence Factors and Exacerbation of Inflammation
Specific fungal virulence factors can exacerbate inflammation in Crohn’s disease. These virulence factors can include enzymes that damage the intestinal lining or proteins that evade the immune system. For instance,C. albicans*, possesses various virulence factors, including adhesion molecules that allow it to colonize the gut and secrete enzymes that degrade host tissues, potentially contributing to tissue damage and inflammation. The precise contribution of individual virulence factors to inflammation in Crohn’s patients requires further investigation.
Recent research suggests a fascinating link between certain fungi and Crohn’s disease, though the exact mechanisms are still being explored. Interestingly, despite vocal anti-vaccine movements, more Americans now seem to trust the measles vaccine, according to this recent study. This highlights a broader trend of scientific understanding and public health, which hopefully will also bring more clarity to the complex role of fungi in inflammatory bowel diseases like Crohn’s.
Diagnostic Methods for Fungal Involvement
Identifying fungal overgrowth in Crohn’s disease patients is crucial for targeted treatment. Precise diagnosis is essential to differentiate fungal infections from other inflammatory processes, avoiding unnecessary antifungal therapy and ensuring appropriate management of the underlying Crohn’s disease. Accurate diagnosis also allows for better monitoring of disease progression and response to treatment.Unfortunately, detecting fungal involvement in Crohn’s is complex.
There’s no single definitive test, and methods often yield inconclusive results, requiring a combination of approaches. The complexity arises from the fact that the gastrointestinal tract, particularly in Crohn’s patients, often has a diverse fungal flora. Identifying pathogenic overgrowth amidst this natural microbial community is a challenge.
Common Diagnostic Methods
Several methods are employed to detect fungal overgrowth in Crohn’s patients. These methods range from traditional culture techniques to advanced molecular approaches. Understanding the strengths and limitations of each is vital for accurate interpretation of results.
Fungal Culture
Fungal culture is a traditional method for identifying fungal species. Samples are collected from affected areas and cultured under controlled conditions. The growth of specific fungi indicates potential infection. However, this method has limitations. It can take several days or weeks to obtain results, and not all fungal species grow easily in culture.
Furthermore, it can be difficult to differentiate between commensal and pathogenic fungi using this method alone.
Polymerase Chain Reaction (PCR)
PCR is a molecular technique that amplifies specific DNA sequences. By targeting fungal DNA, PCR can detect the presence of fungi even in low numbers. This method is more rapid than culture and can identify a broader range of fungal species. However, PCR tests may produce false positives if the sample contains non-viable fungal material. It’s crucial to ensure that the sample preparation and testing are done meticulously to minimize the risk of such false positives.
Histopathology
Histological examination of tissue biopsies can reveal fungal elements. Microscopic analysis of tissue sections allows visualization of fungal hyphae or yeast cells, providing direct evidence of fungal presence. However, the method requires a biopsy, which can be invasive and may not always represent the full extent of fungal colonization. Moreover, the sensitivity of histopathology is influenced by the location and severity of the fungal infection.
Other Diagnostic Tests
Other tests include serological assays to detect fungal antibodies and antigen detection. Serological tests, although helpful in some cases, might not always be indicative of active infection. Antigen detection tests focus on specific fungal molecules, providing more direct evidence of infection. However, these methods are not always readily available and may not be sensitive enough to detect low-level fungal overgrowth.
Diagnostic Test Summary
| Diagnostic Method | Advantages | Disadvantages |
|---|---|---|
| Fungal Culture | Can identify specific fungal species; relatively inexpensive | Slow turnaround time; may not detect all species; requires specialized lab equipment; potential for contamination |
| PCR | Rapid detection; can detect low fungal loads; wider range of species identification; potentially less invasive | False positives possible; may not always correlate with clinical significance; high cost compared to culture |
| Histopathology | Direct visualization of fungal elements; definitive diagnosis | Invasive; may not reflect the full extent of colonization; not always readily available; time-consuming |
| Serological Assays | Useful for monitoring immune response to infection; relatively inexpensive | May not always reflect active infection; not always sensitive; may be influenced by other immune factors |
| Antigen Detection | More direct evidence of infection; potentially rapid results | Limited availability; may not be sensitive to low-level colonization; expensive |
Interpreting Results
Interpreting results from fungal culture and PCR tests requires careful consideration of the clinical context. Positive fungal culture results, particularly when combined with clinical signs and symptoms, strongly suggest fungal overgrowth. However, the presence of fungi alone doesn’t definitively establish causality in Crohn’s disease. Negative results do not rule out fungal involvement entirely. PCR tests require careful interpretation to avoid false positives, and the results should be corroborated with other diagnostic methods.
Therapeutic Approaches Targeting Fungal Overgrowth
Fungal overgrowth, a contributing factor in Crohn’s disease, necessitates targeted therapeutic interventions. Understanding the mechanisms by which fungi interact with the intestinal environment is crucial for developing effective treatment strategies. These strategies must address the specific fungal species implicated and consider the complex interplay between the immune system, the gut microbiome, and the inflammatory processes in Crohn’s disease.Existing antifungal therapies, while available, often present challenges in effectively addressing the localized fungal overgrowth in Crohn’s disease.
This is primarily due to the unique intestinal environment, the potential for drug resistance, and the need to minimize systemic side effects. Furthermore, the precise role of fungi in individual patients’ disease progression warrants further research. Careful consideration of the potential risks and benefits of antifungal treatments is essential.
While researching the role of fungi in Crohn’s disease, I stumbled upon fascinating connections to decluttering. It got me thinking about how a tidy home, like a well-organized gut, might be linked to overall well-being. Just like a well-ordered space can reduce stress and boost productivity, following methods like Marie Kondo’s why tidying up like marie kondo is good for your health and your wallet can help manage stress and promote a sense of calm.
This could indirectly impact the gut microbiome, potentially influencing the complex interactions between fungi and the immune system in Crohn’s disease. Maybe a cleaner environment also helps prevent unwanted fungal overgrowth? The implications are intriguing, even for understanding fungi’s role in the disease.
Existing Antifungal Therapies
A variety of antifungal agents are used in clinical practice. Their effectiveness in Crohn’s disease, however, remains a subject of ongoing investigation. These therapies are often prescribed for localized infections, and their use in Crohn’s disease must be carefully evaluated.
Common Antifungal Drugs and Their Mechanisms
| Drug | Mechanism | Potential Side Effects |
|---|---|---|
| Fluconazole | Inhibits ergosterol synthesis, an essential component of fungal cell membranes. | Headache, nausea, vomiting, abdominal pain, skin rash. Liver dysfunction is a potential serious side effect. |
| Itraconazole | Similar to fluconazole, inhibiting ergosterol synthesis. It also exhibits activity against certain bacteria. | Nausea, vomiting, diarrhea, headache, abdominal pain, liver dysfunction. Cardiac effects, including arrhythmias, have been reported. |
| Voriconazole | Disrupts fungal cell membrane integrity by inhibiting cytochrome P450 enzymes. | Headache, nausea, vomiting, diarrhea, visual disturbances, skin rash, and liver injury. Potential for drug interactions with other medications. |
| Posaconazole | Disrupts fungal cell membrane function by inhibiting fungal enzymes. | Nausea, vomiting, diarrhea, headache, abdominal pain, liver dysfunction, and skin reactions. Possible drug interactions with other medications. |
Challenges and Limitations
Several factors pose challenges to the use of antifungal therapies in Crohn’s disease. First, the specific fungal species involved can vary significantly between individuals. Second, the precise location and extent of fungal overgrowth within the intestine can be difficult to determine. This makes targeted therapy difficult. Third, the complex interplay between fungi, the gut microbiome, and the immune system in Crohn’s disease is not fully understood.
This hinders the development of tailored treatment approaches.
Combination Therapies
The potential for combination therapies with other Crohn’s disease treatments, such as immunomodulators or anti-inflammatory drugs, warrants exploration. For instance, combining antifungals with immunomodulators might enhance the effectiveness of both therapies, potentially reducing the severity of inflammation and controlling fungal overgrowth. However, such approaches require rigorous clinical trials to assess safety and efficacy.
Future Research Directions
Unraveling the complex relationship between fungi and Crohn’s disease requires further investigation. Current research highlights the potential role of fungi in the disease’s pathogenesis, but many questions remain unanswered. Further research is crucial to fully understand the mechanisms involved and develop targeted therapies. Future research must focus on the intricate interactions within the gut microbiome and explore novel therapeutic strategies.
Promising Areas for Future Research
Further investigation into the specific fungal species implicated in Crohn’s disease is paramount. Identifying the dominant fungal species and their interactions with the gut microbiota will provide crucial insights into the disease’s progression. The role of fungal metabolites and their impact on host immune responses needs careful examination. Moreover, exploring the long-term effects of fungal overgrowth on gut barrier function and inflammation is essential.
Interaction Between Fungi and Gut Microbiota
The intricate interplay between fungi and the gut microbiota is a significant area for future research. Understanding how fungal species interact with other microbial communities in the gut, including beneficial bacteria, is vital. The impact of this interaction on the overall gut microbial composition and its influence on the host immune response needs further exploration. Studies should investigate whether specific fungal species promote or inhibit the growth of beneficial bacteria, and how these changes affect the balance of the gut microbiome.
Unanswered Questions Regarding Fungal Involvement
Several critical questions remain regarding the specific mechanisms by which fungi contribute to Crohn’s disease. Determining the threshold for fungal overgrowth that triggers disease is an important area for research. Furthermore, understanding the genetic predisposition of individuals to fungal overgrowth and subsequent inflammatory responses is crucial. Identifying specific fungal virulence factors and their role in immune dysregulation requires further investigation.
Understanding the role of the host immune response to fungi in the context of Crohn’s disease is essential for developing effective treatments.
Need for Large-Scale Clinical Trials
The impact of antifungal treatments on Crohn’s disease warrants large-scale, well-designed clinical trials. These trials should evaluate the efficacy and safety of various antifungal agents, comparing their effects on disease activity, inflammation markers, and overall patient outcomes. Randomized controlled trials are essential to provide robust evidence of the benefits and potential side effects of antifungal interventions in patients with Crohn’s disease.
The selection of appropriate control groups and appropriate endpoints for measuring treatment efficacy is critical for the validity of these studies.
Potential Research Questions and Methods, Fungi role in crohns disease
| Research Question | Potential Methods |
|---|---|
| What is the correlation between specific fungal species and the severity of Crohn’s disease? | Comparative analysis of fecal samples from Crohn’s patients with different disease severities using metagenomic sequencing and culture-based methods. Further investigation into the presence of fungal species and their relative abundance. |
| How do fungal metabolites affect the gut barrier integrity in Crohn’s disease patients? | In vitro studies using human intestinal cell lines exposed to fungal metabolites. In vivo models using animal models of Crohn’s disease to evaluate the impact of fungal metabolites on gut permeability and inflammation. |
| Does antifungal therapy modulate the gut microbiota composition and influence the severity of Crohn’s disease? | Analysis of fecal microbiota composition before and after antifungal therapy using 16S rRNA gene sequencing. Monitoring changes in disease activity and inflammation markers during the course of the treatment. |
| What is the role of genetic predisposition in the development of fungal overgrowth and subsequent inflammation in Crohn’s disease? | Genome-wide association studies (GWAS) to identify genetic variants associated with fungal overgrowth and Crohn’s disease susceptibility. Case-control studies comparing the genetic profiles of Crohn’s patients with and without fungal overgrowth. |
Final Summary
In conclusion, fungi role in crohns disease is a significant area of investigation. While research suggests a potential link, much remains unknown. The complex interplay between fungi, the gut microbiome, and the immune system requires further exploration. Understanding the specific mechanisms, diagnostic tools, and therapeutic strategies will be crucial for improving treatment outcomes. Future research and clinical trials are essential to fully elucidate the role of fungi in Crohn’s disease and potentially develop targeted therapies.
