
Generalized pustular psoriasis images sets the stage for a deep dive into this complex skin condition. We’ll explore the visual characteristics of pustules, their location on the body, and how they differ from other skin conditions. From understanding the various stages of GPP to examining treatment responses, this guide provides a comprehensive visual overview.
This exploration of generalized pustular psoriasis images will delve into the clinical presentation, highlighting the visual differences between GPP and other dermatological conditions. The images will be crucial in aiding in accurate diagnosis and treatment planning.
Introduction to Generalized Pustular Psoriasis
Generalized pustular psoriasis (GPP) is a rare, severe, and sometimes debilitating form of psoriasis characterized by widespread, sterile pustules. It’s a significant concern for patients due to its potential for systemic complications and its impact on quality of life. Understanding its clinical presentation and differentiating it from other psoriasis types is crucial for prompt diagnosis and effective management.GPP is an acute or subacute inflammatory skin condition, typically presenting with numerous small, superficial, sterile pustules on an erythematous base.
The rapid onset and widespread nature of the pustular eruptions can lead to significant discomfort and impairment. Its distinct clinical features differentiate it from other, more common forms of psoriasis, like plaque psoriasis.
Clinical Features of GPP
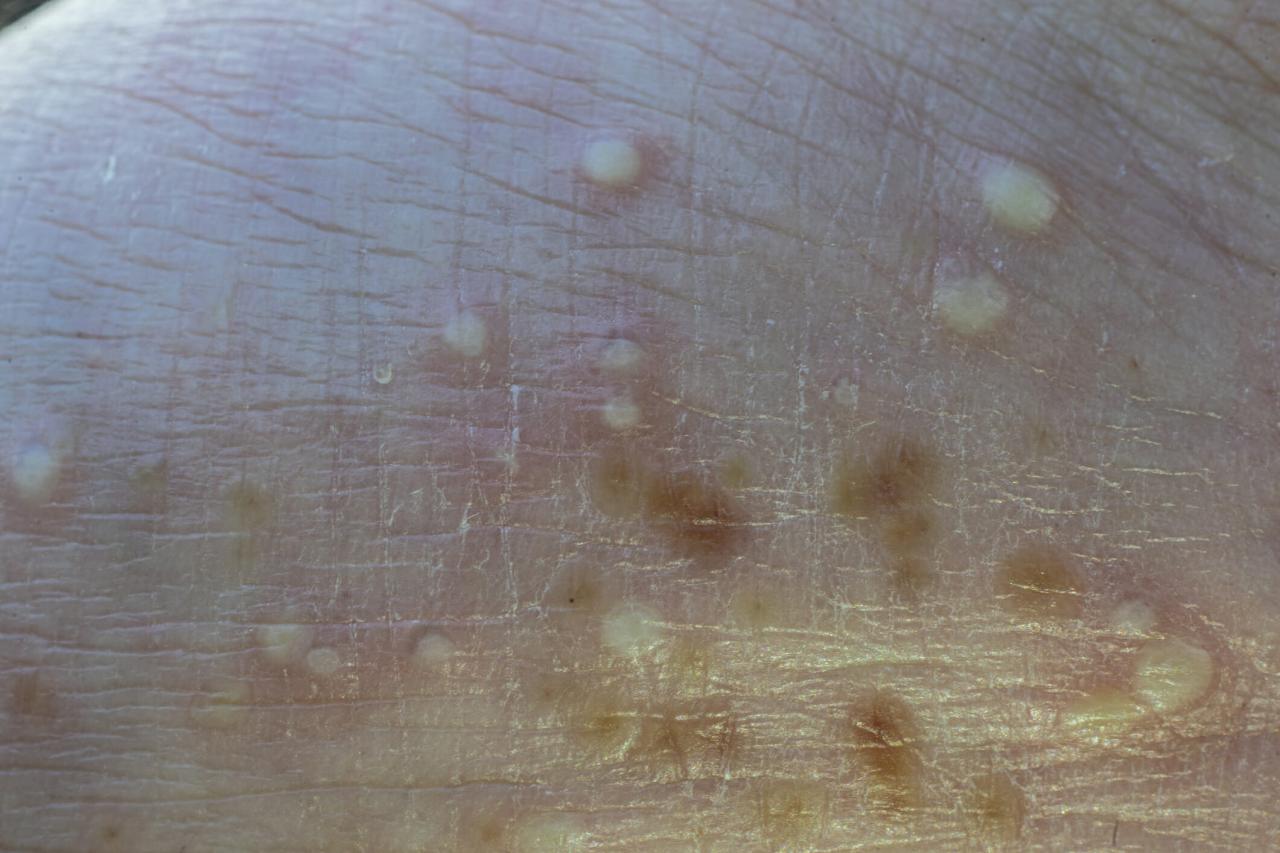
GPP is clinically characterized by widespread sterile pustules on erythematous skin. The pustules are typically small and superficial, often coalescing to form larger areas of involvement. The underlying skin shows varying degrees of inflammation, which may appear red and swollen.
Scrolling through generalized pustular psoriasis images can be truly heartbreaking. Seeing the physical toll this condition takes is powerful, but it makes me wonder about the broader societal factors contributing to suffering. This brings me to the disturbing trend of despair deaths rising in the US. Why despair deaths continue to rise in the US is a complex issue, but it highlights a deeper need for support and resources.
Ultimately, looking at images like these reminds us of the importance of accessible healthcare and mental well-being initiatives for everyone, not just those with generalized pustular psoriasis.
Typical Presentation of GPP Lesions
GPP lesions typically begin as small, discrete, superficial pustules that quickly coalesce. The pustules are filled with a clear or slightly yellowish fluid and are often surrounded by an erythematous halo. The skin around the pustules may be edematous and painful. The skin may appear red, inflamed, and swollen, depending on the severity and duration of the condition. The pustules can vary in size from millimeters to centimeters.
Common Locations of GPP Lesions
GPP lesions can occur anywhere on the body, although some areas are more commonly affected. These include the palms and soles, which are often severely affected, as well as the extremities, trunk, and scalp. In some cases, the entire body surface can be involved.
Comparison of GPP to Other Psoriasis Types
| Feature | Generalized Pustular Psoriasis (GPP) | Plaque Psoriasis |
|---|---|---|
| Lesions | Small, superficial, sterile pustules, often coalescing; erythematous base | Raised, red, scaly plaques; silvery white scales |
| Distribution | Widespread, often affecting palms and soles; can involve the entire body | Usually localized; can be on elbows, knees, scalp, and other areas |
| Symptoms | Severe itching, pain, and tenderness; systemic symptoms possible | Itching, burning, and soreness; often minimal systemic symptoms |
| Severity | Highly variable; can range from mild to severe, potentially life-threatening | Variable; can range from mild to moderate, rarely life-threatening |
Image Characteristics of GPP
Generalized Pustular Psoriasis (GPP) presents a distinctive visual profile in its various stages. Recognizing these characteristics is crucial for accurate diagnosis and effective management. The characteristic pustules, often the most prominent feature, display a range of appearances, colors, and textures that vary with the disease’s progression. This detailed exploration will provide a comprehensive overview of the visual characteristics associated with GPP.The appearance of GPP lesions is highly variable, reflecting the dynamic nature of the disease.
Images often show widespread, erythematous (reddened) skin, covered with numerous small to large pustules. The pustules themselves are a key diagnostic indicator, providing insights into the severity and progression of the condition.
Visual Characteristics of GPP Lesions
GPP lesions are typically characterized by the presence of numerous, superficial pustules on an erythematous base. These pustules vary significantly in size, shape, and distribution across the affected skin surface. The distribution can be localized or generalized, and the intensity of the rash can fluctuate.
Appearance of Pustules in GPP, Generalized pustular psoriasis images
Pustules in GPP manifest in a range of shapes and sizes. They can be small and discrete, or large and confluent, coalescing to form extensive areas of pustular involvement. The shape can range from spherical to oval or irregular, depending on the depth and size of the pustule.
Color Variations of Pustules
The color of GPP pustules can vary, often starting as a pale yellow or whitish-yellow color, which may progress to a more opaque or creamy yellow. As the pustule matures, it may develop a slightly yellowish-brown tint, reflecting the evolution of the inflammatory process. In some cases, the surrounding skin can appear deeply erythematous or inflamed, further highlighting the pustules.
Texture of GPP Pustules
The texture of the pustules is another important visual feature. Early pustules may have a smooth, glistening surface, while more mature pustules might exhibit a slightly rough or crusted texture. The texture changes can provide insight into the stage of the pustular development. The degree of scaling or crusting around the pustules also varies with progression.
Stages of GPP Development
Understanding the progression of GPP can be crucial for treatment. Early-stage images might show small, scattered pustules on an erythematous base. As the disease progresses, pustules can coalesce, forming larger, confluent areas of inflammation. In advanced stages, the skin may appear intensely inflamed and covered with large, interconnected pustules, leading to significant discomfort and systemic symptoms.
Size Ranges of Pustules
| Stage | Approximate Size Range (mm) |
|---|---|
| Early | 1-5 mm |
| Intermediate | 5-10 mm |
| Advanced | >10 mm (often confluent) |
Types of Pustular Psoriasis
| Type | Description |
|---|---|
| Generalized Pustular Psoriasis (GPP) | Characterized by widespread pustules on erythematous skin, often affecting the entire body. |
| Localized Pustular Psoriasis | Limited to a specific area of the body, such as the hands or feet. |
| Acrodermatitis continua of Hallopeau | A rare, chronic form of pustular psoriasis, typically affecting the hands and feet. |
Differential Diagnosis
Generalized pustular psoriasis (GPP) can mimic other skin conditions, making accurate diagnosis crucial. Differentiating GPP from these similar entities relies on a thorough understanding of the clinical presentation, including the distribution, morphology, and duration of the lesions. Careful image analysis and consideration of patient history are vital for distinguishing GPP from other pustular dermatoses.
Comparison to Other Pustular Dermatoses
Pustular eruptions can arise from various causes, requiring careful differentiation from GPP. Key features in the visual analysis help distinguish GPP from other pustular skin conditions. Identifying the presence of acanthosis, parakeratosis, and spongiosis in skin biopsies can further aid in distinguishing GPP.
Pemphigus Vulgaris
Pemphigus vulgaris is a severe autoimmune blistering disease characterized by flaccid bullae, which are large, fluid-filled blisters. These bullae often arise in the oral mucosa and skin. In contrast to GPP, the lesions in pemphigus vulgaris are typically tense and filled with clear fluid. The presence of acantholysis, a breakdown of the epidermis, is a key microscopic finding in pemphigus vulgaris, which is absent in GPP.
The patient history often reveals a chronic, progressive course with skin and oral involvement.
Acute Generalized Exanthematous Pustulosis (AGEP)
AGEP is a drug-induced skin eruption, characterized by widespread erythema and pustules. The pustules in AGEP typically appear within 24-48 hours of exposure to a causative agent, like certain medications. In contrast to GPP, AGEP lesions are more superficial and less likely to be associated with significant nail changes. The abrupt onset and the history of drug exposure help distinguish AGEP from GPP.
Furthermore, AGEP pustules are often smaller and more superficial than those observed in GPP.
Ever seen images of generalized pustular psoriasis? It’s pretty striking, those inflamed, pus-filled bumps. While researching the condition, I stumbled upon an interesting article about how flushing a toilet can release viral droplets – flushing a toilet can release viral droplets what to know – which made me think about the importance of good hygiene practices in general, even when it comes to seemingly mundane things like using the restroom.
Knowing this, it’s even more crucial to understand how to safely handle and manage conditions like generalized pustular psoriasis.
Syphilis
Syphilis, a sexually transmitted infection, can present with pustular lesions. Primary syphilis manifests as a painless chancre, a sore at the site of infection. Secondary syphilis can manifest as a widespread skin rash, often with pustules. However, syphilis often involves other systemic symptoms and a specific history of sexual exposure, helping distinguish it from GPP. Syphilis may also show systemic symptoms like fever, malaise, and lymphadenopathy, which are less common in GPP.
Table: Distinguishing Features of GPP from Other Pustular Dermatoses
| Feature | GPP | Pemphigus Vulgaris | AGEP | Syphilis |
|---|---|---|---|---|
| Lesion Morphology | Large, coalescing pustules, often erythematous base | Flaccid bullae, clear fluid | Small, superficial pustules, erythematous | Pustules, often in a diffuse rash |
| Distribution | Generalized, involving large areas of the skin | Oral mucosa and skin, often symmetrical | Generalized, widespread | Generalized rash, may involve palms and soles |
| Duration | Acute, often lasting weeks to months | Chronic, potentially relapsing | Acute, typically resolving within a few weeks | Chronic, with stages |
| Associated Symptoms | Fever, malaise, erythroderma | Fever, malaise, oral lesions | Fever, malaise, sometimes preceding medication | Fever, malaise, lymphadenopathy |
| Etiology | Psoriatic | Autoimmune | Drug-induced | Infectious |
Patient Presentation and Symptoms: Generalized Pustular Psoriasis Images
Generalized pustular psoriasis (GPP) presents with a distinctive and often distressing array of symptoms. Understanding these symptoms is crucial for accurate diagnosis and effective management. The visual characteristics of the skin lesions, coupled with systemic manifestations, provide key information for clinicians.The characteristic skin eruptions of GPP are typically widespread, leading to significant discomfort and impacting a patient’s quality of life.
The symptoms vary in intensity and presentation, reflecting the dynamic nature of the disease. This variability in symptoms highlights the importance of careful patient evaluation.
Typical Skin Symptoms
GPP is characterized by the sudden onset of numerous sterile pustules, which are small, fluid-filled blisters, on erythematous (reddened) skin. These pustules are often densely clustered and can coalesce, forming large, weeping areas. The skin involvement is typically widespread, affecting large portions of the body. The affected skin may be extremely inflamed, leading to intense pain and itching.
In severe cases, the skin can become thickened and cracked. A visual description of the pustules is essential for diagnosis.
Systemic Symptoms
GPP is frequently associated with systemic symptoms, including high fever, chills, and malaise. These systemic manifestations often accompany the skin eruptions and can significantly impact a patient’s overall well-being. The presence of these systemic symptoms necessitates careful monitoring and supportive care.
Severity Levels
GPP can range in severity from mild to severe. The severity is assessed based on the extent of skin involvement, the intensity of symptoms, and the presence of systemic manifestations.
Looking at generalized pustular psoriasis images can be really unsettling, but understanding the condition better is key. Fortunately, exploring alternative treatments can be equally enlightening. For instance, delving into resources like the best books on alternative medicine can provide valuable insights into different approaches to managing this condition. best books alternative medicine might offer practical advice and different perspectives on natural remedies.
Ultimately, researching generalized pustular psoriasis images and exploring various treatment options can empower you to make informed decisions about your health.
- Mild GPP: Characterized by a relatively limited number of pustules, confined to specific areas of the body. Systemic symptoms are usually absent or minimal.
- Moderate GPP: Displays a more extensive skin eruption with a wider distribution of pustules. Systemic symptoms such as fever and malaise may be present, but are not debilitating.
- Severe GPP: Involves almost the entire body surface with numerous pustules. Systemic symptoms are pronounced, including high fever, significant dehydration, and electrolyte imbalances. This form of GPP can be life-threatening and requires immediate medical attention.
Relationship Between Symptoms and Image Appearance
Images of GPP typically show a diffuse erythematous rash covered with numerous small, sterile pustules. The pustules may coalesce into larger areas of weeping skin. The severity of skin involvement is directly related to the extent and density of the pustular lesions. For example, images of mild GPP will demonstrate fewer pustules and less extensive skin involvement compared to images of severe GPP.
Comparison with Other Skin Conditions
| Symptom | GPP | Psoriasis (Plaque Type) | Eczema |
|---|---|---|---|
| Skin Lesions | Numerous sterile pustules, erythematous | Plaque-like lesions, erythematous, silvery scales | Erythematous, weeping, itchy lesions, often with lichenification (thickening) |
| Systemic Symptoms | Frequently present (fever, malaise) | Rarely present | Rarely present, but may be associated with allergic reactions |
| Distribution | Widespread | Patchy, often on extensor surfaces | Variable, may be localized or widespread |
Treatment Approaches and Outcomes
Generalized pustular psoriasis (GPP) presents a significant challenge for dermatologists due to its unpredictable course and often severe inflammatory response. Effective treatment aims to control the inflammatory process, reduce pustule formation, and prevent complications. Treatment decisions are often complex and require careful consideration of the individual patient’s presentation, disease severity, and potential side effects.Treatment strategies for GPP are multifaceted and typically involve a combination of approaches, recognizing that a single therapy may not be sufficient.
A thorough understanding of the diverse treatment options and their potential outcomes is crucial for achieving optimal patient care. The efficacy of different treatments can vary considerably, and factors like disease duration, severity, and patient response influence the success of a particular intervention.
Diverse Treatment Modalities
Various therapeutic approaches are employed to manage GPP, ranging from topical agents to systemic medications. The selection of appropriate treatment strategies is guided by the severity and extent of the disease, and the patient’s overall health status. The goal is to achieve rapid control of the inflammatory response and reduce the burden of the disease.
Systemic Therapies
Systemic therapies are often necessary for managing severe or recalcitrant cases of GPP. These treatments target the systemic inflammatory response and can be highly effective in reducing the pustular eruption and improving overall patient well-being. Corticosteroids, for example, can rapidly suppress inflammation but are often associated with potential side effects. Methotrexate, an immunosuppressant, is frequently used in severe GPP and can effectively control the disease process.
Cyclosporine, another immunosuppressant, can also be considered in refractory cases. Biologics targeting specific inflammatory pathways are emerging as important treatment options. Their efficacy in GPP is frequently demonstrated in clinical trials and case reports.
Topical Treatments
Topical treatments play a crucial role in managing GPP, particularly in milder cases or as adjunctive therapy to systemic medications. Topical corticosteroids can help reduce inflammation and itching, while topical calcineurin inhibitors can effectively control the inflammatory process. These agents often provide localized relief and can be particularly useful in managing localized flares. The choice of topical agent is based on the severity of the pustular involvement and the patient’s response to previous treatments.
Phototherapy
Phototherapy, such as UVB or PUVA, can be effective in managing GPP, particularly in cases where other treatments have been less successful. The precise mechanisms through which phototherapy works in GPP are not fully understood, but the ability to control inflammation and reduce pustule formation is well-documented. Phototherapy often involves a gradual increase in the dose of UV light to optimize efficacy and minimize adverse effects.
Image-Based Treatment Response Assessment
Image analysis plays a vital role in assessing the response to treatment. Early clinical trials have documented the use of dermatoscopic images to evaluate the pustular count, size, and distribution before and after treatment. Such data analysis can provide objective metrics for evaluating the effectiveness of various therapeutic strategies. The reduction in pustular lesions and improvement in skin integrity can be visually observed through before-and-after images, providing a direct measure of treatment success.
Treatment Decision-Making Process
Treatment decisions in GPP are based on a multifaceted evaluation of the patient’s condition, including the severity of the disease, the extent of skin involvement, the patient’s response to previous therapies, and potential side effects. The physician considers the risks and benefits of each treatment option and selects the most appropriate approach to achieve the best possible outcome. Image analysis can help to track the response to treatment, allowing the physician to adjust the treatment plan as needed.
Table of Common Treatment Options and Efficacy
| Treatment Option | Efficacy in GPP | Potential Side Effects |
|---|---|---|
| Systemic Corticosteroids | High efficacy in acute flares, but limited long-term use due to side effects. | Cushingoid features, osteoporosis, adrenal suppression |
| Methotrexate | Highly effective in controlling disease activity; can be associated with liver toxicity. | Hepatotoxicity, nausea, fatigue |
| Cyclosporine | Effective in severe cases, but potential for nephrotoxicity and hypertension. | Nephrotoxicity, hypertension, tremor |
| Biologics | Emerging as powerful tools; varies in efficacy and potential side effects. | Infections, malignancy |
| Topical Corticosteroids | Useful for localized relief; limited systemic effects. | Skin atrophy, telangiectasia |
| Phototherapy | Effective in some cases; requires careful monitoring. | Skin reactions, sunburn |
Impact on Quality of Life
Generalized pustular psoriasis (GPP) is more than just a skin condition; it significantly impacts a patient’s overall well-being. The chronic, often debilitating nature of GPP can lead to profound psychological distress and substantial limitations in daily activities. Understanding these impacts is crucial for providing comprehensive care and support to those affected.GPP profoundly affects a patient’s emotional state and daily routines.
The constant discomfort, pain, and appearance issues associated with the disease can lead to significant emotional distress, impacting self-esteem, body image, and social interactions. This often results in isolation and feelings of hopelessness. Managing these psychological effects is as important as treating the physical symptoms.
Psychological Effects of GPP
The chronic nature of GPP, coupled with the intense physical discomfort and the visible nature of the skin lesions, can lead to a range of psychological effects. Patients may experience feelings of anxiety, depression, and low self-esteem due to the appearance of the lesions. Social isolation and difficulty maintaining relationships are common consequences. The constant need for medical attention and the unpredictable nature of the disease can also contribute to feelings of stress and frustration.
Furthermore, the emotional toll of dealing with a chronic condition can significantly impact overall mental health.
Impact on Daily Activities
GPP can severely disrupt daily activities. The widespread skin involvement and intense itching can make simple tasks like showering, dressing, and even sleeping extremely difficult. Pain and discomfort can also limit mobility and participation in social activities. The impact extends beyond physical limitations. Work productivity can suffer, leading to financial hardship, and the need for frequent medical appointments can further restrict time and energy.
These limitations highlight the need for supportive strategies and accommodations.
Patient Stories
“I felt like I was invisible,” shares Sarah, a GPP patient. “The constant pain and discomfort made it hard to focus on anything else. I felt isolated, like no one could understand what I was going through.” Another patient, David, describes the difficulty in maintaining his job due to frequent flare-ups and the time required for medical appointments. These are just two examples of the numerous real-life stories that highlight the profound impact GPP has on patients’ lives.
Quality of Life Aspects Affected by GPP
| Aspect of Quality of Life | Description |
|---|---|
| Physical | Pain, discomfort, itching, difficulty with daily tasks, limitations in mobility |
| Emotional | Anxiety, depression, low self-esteem, body image issues, social isolation |
| Social | Difficulty maintaining relationships, social withdrawal, avoidance of social situations |
| Occupational | Reduced work productivity, potential job loss, financial hardship |
| Financial | Increased medical expenses, lost wages due to time off work |
| Psychological | Stress, frustration, feelings of hopelessness, difficulty concentrating |
Challenges Faced by GPP Patients
| Challenge | Explanation |
|---|---|
| Physical discomfort | Constant pain, itching, and widespread skin lesions hinder daily activities. |
| Emotional distress | Anxiety, depression, and low self-esteem are common due to the chronic nature and appearance of the condition. |
| Social isolation | Difficulty maintaining relationships and participation in social activities. |
| Occupational limitations | Reduced work productivity and potential job loss due to frequent flare-ups and medical appointments. |
| Financial hardship | Increased medical expenses and lost wages can strain financial resources. |
| Access to appropriate treatment | Finding effective treatment and managing the condition can be challenging for some patients. |
Preventive Measures and Prognosis

Generalized pustular psoriasis (GPP) is a severe and debilitating skin condition, often requiring intensive treatment and impacting quality of life significantly. While a definitive cure remains elusive, understanding preventative measures and the prognosis for individuals with GPP is crucial for effective management and improved patient outcomes. Prognosis, influenced by various factors, is a critical aspect of care planning, empowering patients and healthcare providers with a more comprehensive understanding of the disease trajectory.Understanding the factors influencing the prognosis of GPP is vital for tailoring treatment strategies and anticipating potential complications.
Prognosis prediction, although not always precise, can be enhanced through careful monitoring and the evaluation of various clinical markers. This allows for proactive interventions to mitigate disease progression and improve long-term outcomes.
Preventive Measures
Effective preventive measures for GPP are largely focused on managing triggers and maintaining overall health. While there’s no single preventative strategy guaranteed to prevent future flares, certain lifestyle choices and medical interventions can help mitigate the risk of recurrence. Avoiding known triggers, like stress, certain medications, and infections, can play a significant role in preventing flare-ups. Maintaining a healthy diet and regular exercise can also contribute to overall well-being and potentially reduce the frequency and severity of GPP episodes.
Prognosis Factors
GPP prognosis is complex, influenced by a variety of interconnected factors. Age at onset, disease duration, frequency of flares, and the presence of other comorbidities are key elements. The severity of the initial presentation and the response to initial treatments are also critical indicators of potential long-term outcomes. Genetic predisposition and the presence of other inflammatory conditions can also affect the course of the disease.
Image Analysis and Prognosis Prediction
While image analysis of GPP lesions doesn’t directly determine prognosis, it can provide valuable insights into disease activity and severity. Assessment of the extent and distribution of pustules, erythema, and scaling in images can assist in monitoring treatment effectiveness and predicting potential flare-ups. However, image analysis alone is insufficient for prognosis prediction; it must be combined with clinical assessment, patient history, and other diagnostic tools.
For example, a significant increase in the area affected by pustules, as evidenced in successive images, might suggest a worsening prognosis and necessitate a change in treatment strategy.
Importance of Regular Monitoring and Follow-up
Regular monitoring and follow-up care are crucial for managing GPP effectively. This involves frequent assessments of disease activity, evaluation of treatment response, and adjustments to the treatment plan as needed. Regular check-ups allow for early detection of potential complications, enabling timely interventions and minimizing the risk of long-term damage. Maintaining open communication between patients and healthcare providers is essential for successful long-term management.
Long-Term Outcomes
Long-term outcomes in GPP cases can vary significantly. Some patients experience infrequent flares and relatively stable disease control, while others experience more frequent and severe episodes, leading to significant functional impairment. Factors such as adherence to treatment, management of comorbidities, and overall health status play a crucial role in shaping long-term outcomes. Examples of successful long-term management often include individuals who have effectively managed their GPP through consistent treatment and lifestyle adjustments, achieving periods of remission or significantly reduced disease activity.
Table Summarizing Prognosis Factors
| Factor | Description | Influence on Prognosis |
|---|---|---|
| Age at Onset | Age at the initial diagnosis of GPP | Earlier onset often associated with more severe or chronic course |
| Disease Duration | Length of time since diagnosis | Longer duration may correlate with more frequent flares and increased risk of complications |
| Frequency of Flares | Number of flare-ups experienced | Higher frequency generally points to a more challenging prognosis |
| Comorbidities | Presence of other medical conditions | Presence of other inflammatory conditions may worsen prognosis |
| Treatment Response | Effectiveness of initial treatment | Rapid and sustained response to treatment often predicts a better prognosis |
| Severity of Initial Presentation | Intensity of initial symptoms | More severe initial symptoms may indicate a more challenging long-term course |
| Genetic Predisposition | Family history of GPP | Family history may increase the risk of developing GPP and influence prognosis |
Closing Summary
In conclusion, generalized pustular psoriasis images offer a valuable tool for understanding and diagnosing this challenging skin condition. By examining the visual characteristics, comparing them to other conditions, and observing treatment responses, we gain a more profound insight into the complexities of GPP. This detailed visual guide empowers readers to grasp the nuances of this condition.
