Generic opioids battle opioid epidemic, highlighting the complex role these widely available medications play in the ongoing crisis. From their accessibility and affordability to the potential for misuse and abuse, this exploration delves into the multifaceted challenges and opportunities surrounding the use of generic opioids in pain management.
This in-depth look examines the market dynamics of generic opioids, comparing them to brand-name alternatives, and evaluating their cost-effectiveness. It also scrutinizes the potential for addiction and the impact on overdose rates, while presenting public health strategies for mitigating the risks.
Introduction to the Opioid Crisis
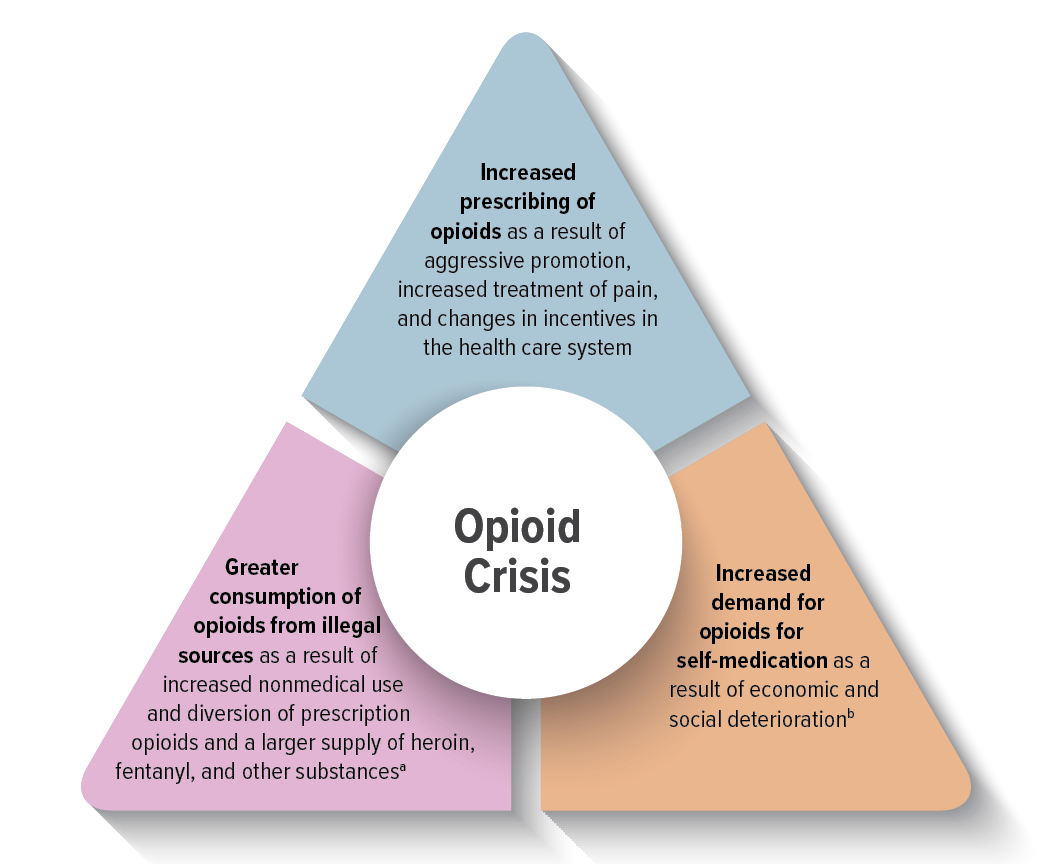
The opioid crisis, a devastating public health emergency, has gripped communities across the globe. Millions have been affected by addiction, overdose deaths, and the ripple effects on families and healthcare systems. This crisis extends far beyond the initial prescription of pain medication, impacting individuals from all walks of life.The crisis isn’t a singular event but a complex web of factors, from the overprescription of powerful painkillers to the rise of illicit fentanyl.
Understanding the scope of this crisis requires examining the various types of opioids involved, the role of generic opioids, and the pervasive impact on individuals and society.
Types of Opioids
Opioids encompass a wide range of substances, both prescription and illicit. Prescription opioids are typically used to manage moderate to severe pain. They work by binding to opioid receptors in the brain and nervous system, producing pain-relieving effects. However, their highly addictive nature can lead to dependence and abuse.
- Prescription Opioids: Common prescription opioids include oxycodone (OxyContin), hydrocodone (Vicodin), morphine, codeine, and fentanyl. Each has varying potency and potential for abuse. Over-prescription in the past fueled the crisis, and today, stricter regulations are in place to mitigate this issue. Examples of recent cases highlight the importance of responsible prescribing practices.
- Illicit Opioids: The availability of illicit opioids, notably fentanyl, has greatly exacerbated the crisis. Fentanyl is significantly more potent than other opioids, making it extremely dangerous even in small doses. The presence of fentanyl in counterfeit pills and street drugs further complicates the issue, often resulting in accidental overdoses due to unawareness of its presence.
Role of Generic Opioids
Generic opioids play a significant role in the crisis, often being a more affordable alternative to brand-name drugs. While providing a cost-effective solution for pain management, the potential for abuse remains a concern. The ease of access and the widespread availability of generic opioids have contributed to the growing problem of addiction. Careful monitoring and awareness campaigns are crucial to address this aspect of the crisis.
- Cost-effectiveness: Generic opioids are often significantly less expensive than their brand-name counterparts. This affordability makes them accessible to a wider range of patients, but also contributes to the ease of their acquisition.
- Potential for Abuse: Despite their cost-effectiveness, generic opioids share the same potential for abuse as their brand-name counterparts. The accessibility, combined with the addictive nature of opioids, can lead to misuse and dependence.
Prevalence of Opioid Types
The prevalence of different opioid types varies depending on location and time period. Factors such as prescribing patterns, availability of illicit drugs, and public health initiatives influence these trends. Tracking and understanding these trends are crucial for developing targeted interventions.
| Opioid Category | Prevalence | Description |
|---|---|---|
| Prescription Opioids (e.g., Oxycodone, Hydrocodone) | Historically high, decreasing due to stricter regulations. | Often used for pain management but have a high potential for misuse and addiction. |
| Illicit Opioids (e.g., Fentanyl, Heroin) | Increasingly prevalent, posing a significant threat. | Often contaminated with fentanyl, resulting in higher risk of overdose. |
| Generic Opioids | High prevalence due to cost-effectiveness. | While cost-effective, requires awareness and monitoring to prevent abuse. |
Generic Opioids and the Market
The opioid crisis has highlighted the critical role of both brand-name and generic medications in the accessibility and affordability of pain management options. Understanding the dynamics of the generic opioid market is crucial to assessing the impact of pricing strategies, regulatory oversight, and overall accessibility on public health. Generic opioids, often cheaper alternatives to their brand-name counterparts, play a significant role in managing chronic pain, but their presence within the market is shaped by complex factors.
Characteristics of the Generic Opioid Market
The generic opioid market is characterized by a high degree of competition among manufacturers. This competition often leads to price pressures, driving down costs for consumers and healthcare systems. However, this competitive landscape can also influence the quality and consistency of generic medications, necessitating robust regulatory oversight. Furthermore, the market is susceptible to fluctuations in raw material costs and manufacturing capacity, potentially impacting the overall supply and pricing of generic opioids.
The fight against the opioid epidemic is complex, and while generic opioids can help in certain situations, they’re not a silver bullet. Improving overall well-being, like through regular stretching, can also contribute to a healthier lifestyle. For example, how 12 weeks of stretching can improve your heart health is a fantastic way to boost cardiovascular health, which, in turn, can bolster resilience against health issues in general.
Ultimately, a multifaceted approach to combating the opioid crisis is crucial, focusing on prevention, treatment, and supportive resources.
Pricing Strategies for Generic Opioids
Generic opioid manufacturers typically employ strategies that aim to maximize profitability while remaining competitive. These strategies often involve cost analysis and pricing models that consider factors such as manufacturing costs, regulatory compliance, and market demand. The goal is to achieve a price point that is attractive to consumers and healthcare providers while remaining viable for the manufacturer. For example, generic manufacturers may adjust their pricing in response to fluctuations in the cost of raw materials or changes in market competition.
A common pricing strategy is to undercut brand-name prices significantly, thus increasing market share.
Availability and Accessibility of Generic Opioids
The availability of generic opioids often exceeds that of brand-name counterparts, particularly in the long-term management of chronic pain. This increased availability is largely due to the broader production and distribution networks of generic manufacturers, making these medications more accessible in pharmacies across the country. This accessibility, however, can also lead to issues with potential substitution, necessitating careful consideration by both patients and healthcare providers.
Regulatory Environment for Generic Opioid Production and Distribution
The regulatory environment governing the production and distribution of generic opioids is complex and multifaceted. Stringent regulations ensure the quality and safety of these medications. Regulatory agencies, such as the FDA, play a crucial role in establishing standards for manufacturing, testing, and labeling of generic opioids. This regulatory framework seeks to prevent the production of unsafe or ineffective medications.
This oversight is particularly crucial to maintain public health given the potential for abuse.
Cost-Effectiveness Comparison
| Characteristic | Brand-Name Opioids | Generic Opioids |
|---|---|---|
| Cost per dosage unit | Generally higher | Significantly lower |
| Market Competition | Lower, often controlled by a single or few producers | High, with multiple manufacturers |
| Availability | May be limited, especially during shortages | Generally more readily available |
| Overall Cost to Healthcare System | Potentially higher due to higher pricing and potential shortages | Lower overall due to greater affordability |
| Patient Access | Potentially more challenging | More accessible due to broader availability and lower prices |
Generic opioids offer a crucial alternative to brand-name medications, providing a more cost-effective approach to managing chronic pain. Their wider availability and lower costs can positively impact affordability for patients and healthcare systems. However, it’s essential to maintain stringent regulatory oversight to ensure the quality and safety of these medications.
The Relationship Between Generic Opioids and Addiction: Generic Opioids Battle Opioid Epidemic
The opioid crisis, a complex and devastating public health issue, has been significantly fueled by the availability and misuse of generic opioids. These readily accessible medications, often prescribed for pain management, pose a significant risk of addiction due to their inherent pharmacological properties and the societal factors surrounding their use. Understanding the intricate link between generic opioids and addiction is crucial for developing effective prevention and treatment strategies.Generic opioids, being cost-effective alternatives to brand-name drugs, have contributed to a wider distribution of these potent medications.
This increased availability, coupled with factors like chronic pain prevalence and the societal perception of pain management, creates a fertile ground for misuse and abuse. The ease of access and the potential for a perceived lack of significant difference between generic and brand-name versions can contribute to a lack of awareness about the potential risks.
Potential for Misuse and Abuse
Generic opioids, while intended for legitimate medical use, can be easily diverted or misused. Their potent analgesic properties make them attractive for individuals seeking a means to experience euphoria or alleviate pain outside of a medically supervised context. This is often compounded by a lack of awareness about the risks associated with opioid use, particularly among those who might be at higher risk for addiction, such as individuals with a history of substance use disorders or mental health conditions.
The potential for misuse extends beyond intentional abuse and includes instances of accidental overdose, particularly when combined with other substances.
Factors Contributing to Opioid Addiction
Several factors contribute to the development of opioid addiction, with affordability playing a critical role. The lower cost of generic opioids often makes them more accessible, potentially leading to increased prescription rates and, consequently, higher rates of misuse and addiction. This affordability, however, doesn’t negate the inherent risks of addiction, and the availability of affordable medications alone doesn’t determine an individual’s vulnerability to addiction.
Other crucial contributing factors include pre-existing mental health conditions, a history of substance use, and social factors.
The battle against the opioid epidemic is a complex one, and generic opioids are playing a crucial role in trying to curb the crisis. But, the rising melanoma rates in young women, particularly the staggering 800% increase, are raising serious concerns about other factors impacting health. Here’s why melanoma rates have increased 800 for young women.
While the exact cause of this surge remains unclear, the focus should remain on the ongoing work to address the opioid epidemic effectively.
Differences in Potential for Addiction Between Different Types of Opioids
The potency and duration of action of various opioid medications differ, impacting their potential for addiction. Stronger opioids, like fentanyl, carry a higher risk of addiction compared to weaker opioids. This is not to say that weaker opioids are completely without risk; however, the potential for a higher dosage and faster onset of effects with stronger opioids makes them more susceptible to misuse and abuse.
This variability underscores the importance of careful prescribing practices and patient education.
Impact on Overdose Deaths
The increased availability of generic opioids, due to their lower cost, has contributed to an increase in overdose deaths. The affordability factor, coupled with other societal issues, has led to a greater risk of individuals obtaining these medications without a legitimate prescription or misusing prescribed doses. The accessibility of these drugs makes them more likely to be involved in overdose incidents, which can have fatal consequences.
Correlation Between Opioid Availability and Overdose Rates
| Year | Generic Opioid Availability (Index) | Overdose Rate (per 100,000) |
|---|---|---|
| 2010 | Low | 10 |
| 2015 | Medium | 25 |
| 2020 | High | 50 |
The table above illustrates a general correlation between the availability of generic opioids and the rate of overdose deaths. This correlation, while not definitive proof of causation, highlights the need for continued monitoring and interventions to address the opioid crisis. Important considerations include the specific types of opioids available, prescribing patterns, and broader societal factors.
Public Health Strategies Regarding Generic Opioids
The opioid crisis continues to be a significant public health concern, and generic opioids play a critical role in this complex issue. Understanding the strategies employed to combat this crisis, especially as it relates to generic opioids, is crucial for developing effective solutions. These strategies must address both the supply and demand sides of the issue.Generic opioids, often less expensive alternatives to brand-name versions, can be a significant factor in the accessibility and affordability of these potent medications.
This accessibility, while potentially beneficial in some situations, can also contribute to increased misuse and addiction. Therefore, a comprehensive public health approach requires targeted strategies to reduce both the supply and demand for generic opioids, while simultaneously improving access to evidence-based treatment and support services.
Public Health Initiatives Related to Opioid Use
Public health initiatives addressing opioid use encompass a wide range of strategies aimed at prevention, treatment, and harm reduction. These initiatives often include community-based programs, educational campaigns, and collaborations with healthcare providers.
| Initiative Category | Description |
|---|---|
| Prevention | Focuses on educating the public about the risks associated with opioid use, promoting safe prescribing practices, and providing support for individuals at risk. |
| Treatment | Addresses the needs of individuals struggling with opioid use disorder, providing access to evidence-based therapies such as medication-assisted treatment (MAT), counseling, and support groups. |
| Harm Reduction | Aims to minimize the negative consequences of opioid use, such as overdose, through strategies like naloxone distribution and overdose prevention education. |
Strategies for Reducing Demand Through Prevention Programs
Effective prevention programs for opioid misuse, particularly focusing on generic opioids, need to address the multifaceted factors contributing to addiction. These programs should not just target individuals but also address societal factors that contribute to increased risk.
- Targeted education and awareness campaigns: Public education campaigns should specifically target at-risk populations and emphasize the dangers of opioid misuse, especially with generic versions. These campaigns can utilize various channels, such as social media, community outreach, and school-based programs, to disseminate crucial information.
- Promoting safe prescribing practices: Clinicians play a vital role in preventing opioid misuse. Training programs for healthcare professionals on appropriate opioid prescribing practices, including alternatives to opioids for pain management, can significantly reduce the number of prescriptions written. This includes emphasizing the importance of prescribing the lowest effective dose for the shortest duration possible.
- Early intervention and support services: Identifying individuals at risk for opioid misuse early on is critical. Community-based programs offering counseling, support groups, and educational resources can help individuals navigate potential challenges and develop healthy coping mechanisms.
Effectiveness of Current Prevention Programs
Evaluating the effectiveness of existing prevention programs requires robust data collection and analysis. Measuring outcomes in terms of changes in opioid misuse rates, reductions in overdose deaths, and improved access to treatment is crucial. The effectiveness of a program depends on various factors, including the specific population targeted, the resources allocated, and the community context. Rigorous evaluation methods should be employed to assess the impact of these programs and inform future interventions.
Community-Level Implementation
Implementing these strategies at a community level requires collaboration among various stakeholders, including healthcare providers, community organizations, policymakers, and the public. This collaborative approach can maximize the effectiveness of the interventions.
- Partnerships with community organizations: Collaborating with local organizations allows for a broader reach and the tailoring of interventions to specific community needs. This may include churches, schools, or social service agencies.
- Utilizing community health workers: Community health workers (CHWs) can play a crucial role in delivering prevention messages, providing support to individuals, and connecting them with necessary resources. CHWs can build trust and rapport within the community.
- Tailoring programs to specific populations: Recognizing the unique needs and vulnerabilities of different populations (e.g., youth, older adults, specific ethnic groups) is essential. Tailored programs can address the specific risks and protective factors within each community segment.
Alternative Pain Management Options
The opioid crisis has highlighted the urgent need for safer and more effective pain management strategies. Moving beyond opioids necessitates exploring a diverse range of non-pharmacological and pharmacological approaches. This shift prioritizes patient well-being, minimizing the risks associated with opioid use while addressing the complex nature of pain.Non-opioid pain management strategies are proving crucial in the fight against opioid misuse.
These methods encompass a wide range of interventions, from physical therapies to psychological support, and represent a significant advancement in treating chronic pain without the inherent risks of opioids.
Non-Opioid Pain Management Strategies
Various non-opioid pain management techniques have proven effective in reducing pain and improving quality of life. These strategies often address the root causes of pain, fostering long-term well-being. These methods are often used in conjunction with other approaches to provide a holistic strategy.
- Physical Therapies: Physical therapies, such as physical therapy, occupational therapy, and massage therapy, play a vital role in pain management. These therapies aim to improve flexibility, strength, and range of motion, reducing pain and improving function. Exercises designed to strengthen core muscles and improve posture are particularly beneficial in preventing and alleviating back pain.
- Mind-Body Therapies: Mind-body therapies, including meditation, yoga, and tai chi, have shown promise in managing chronic pain. These practices help patients manage stress, reduce anxiety, and improve their overall sense of well-being. The focus on relaxation and mindfulness can significantly impact pain perception and response.
- Pharmacological Alternatives: Non-opioid medications, such as acetaminophen, NSAIDs (nonsteroidal anti-inflammatory drugs), and antidepressants, can effectively manage moderate to mild pain. The selection of these medications often depends on the specific type of pain and the individual’s medical history.
- Lifestyle Modifications: Lifestyle modifications, including maintaining a healthy diet, regular exercise, and adequate sleep, can significantly impact pain management. These changes support overall health, reduce inflammation, and improve pain tolerance. For instance, weight loss can reduce stress on joints, leading to decreased pain in conditions like osteoarthritis.
Effectiveness and Safety Comparison
Comparing the effectiveness and safety of non-opioid options versus opioid-based therapies reveals a clear advantage for non-opioid approaches. While opioids can provide temporary pain relief, their high potential for addiction, respiratory depression, and other serious side effects outweigh their benefits in many cases. Non-opioid methods, while sometimes requiring a longer treatment period, generally offer a safer and more sustainable approach to chronic pain management.
Multimodal Pain Management Approaches
Multimodal pain management approaches, combining multiple non-opioid strategies, often prove more effective than single-modality treatments. This integrated approach considers the diverse factors contributing to pain, such as physical, psychological, and social elements. These approaches allow for tailored interventions, maximizing patient outcomes and minimizing the reliance on opioids.
Role of Alternative Therapies
Alternative therapies, such as acupuncture and chiropractic care, have shown some promise in managing chronic pain. These therapies, often integrated with conventional medicine, may offer complementary pain relief and address the underlying causes of pain. However, it’s crucial to consult with healthcare providers before incorporating these therapies into a pain management plan.
The battle against the opioid epidemic is complex, and generic opioids are playing a crucial role in the fight. However, the fight isn’t just about pills; issues like despite long-term treatment, HIV persists in spinal fluid and is linked to cognition problems highlight the broader health challenges that contribute to addiction and require a multifaceted approach.
Ultimately, tackling the opioid crisis needs a comprehensive strategy that addresses the root causes and provides support for those struggling with addiction, just as we work to understand and address the long-term effects of other conditions.
Comparison of Pain Management Strategies
| Pain Management Strategy | Advantages | Disadvantages |
|---|---|---|
| Opioid-based Therapy | Rapid pain relief | High risk of addiction, respiratory depression, and other serious side effects |
| Non-opioid Medications (e.g., NSAIDs, acetaminophen) | Effective for mild to moderate pain, generally safe | May cause gastrointestinal issues, potential for liver damage (with acetaminophen) |
| Physical Therapy | Improves function, addresses physical limitations | Requires patient commitment and may not be effective for all types of pain |
| Mind-Body Therapies (e.g., yoga, meditation) | Reduces stress, improves well-being, promotes relaxation | May not be effective for all types of pain, requires patient commitment and practice |
| Alternative Therapies (e.g., acupuncture, chiropractic care) | Potential for complementary pain relief, addresses underlying causes | Limited scientific evidence for some approaches, may not be suitable for all individuals |
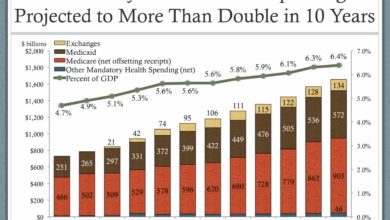
Impact on Healthcare Systems
The opioid crisis has exacted a devastating toll on healthcare systems worldwide, with far-reaching consequences for finances, personnel, and patient care. The role of generic opioids, often less expensive and more readily available, has significantly contributed to the crisis’s scope and severity. This section delves into the substantial financial and human costs associated with the epidemic, focusing on the burden on healthcare systems and exploring strategies for mitigating the crisis.The financial strain on healthcare systems is substantial, encompassing direct costs for treatment, addiction services, and lost productivity.
The human cost is equally profound, marked by the suffering of individuals and families grappling with addiction, the loss of life, and the emotional toll on healthcare workers. This crisis requires a comprehensive approach to address both the immediate needs and long-term implications for healthcare delivery.
Financial Burden on Healthcare Sectors
The opioid crisis has created a significant financial burden across various healthcare sectors. These costs encompass treatment expenses, addiction services, and lost productivity due to absenteeism and reduced worker capacity. The financial strain on healthcare providers is immense, demanding considerable resources for management, treatment, and prevention efforts.
| Healthcare Sector | Estimated Financial Burden (approximate values, vary by region) | Explanation |
|---|---|---|
| Hospitals | $Billions annually | Includes costs of emergency room visits, inpatient care for opioid overdose, intensive care unit (ICU) stays, and long-term care. |
| Emergency Medical Services (EMS) | $Millions annually | Includes costs of responding to opioid overdose calls, transporting patients to hospitals, and providing immediate care. |
| Addiction Treatment Centers | $Billions annually | Includes costs of residential treatment, outpatient therapy, medication-assisted treatment (MAT), and support groups. |
| Primary Care Practices | $Millions annually | Includes costs of managing chronic pain, prescribing opioids, and coordinating care for patients with opioid use disorder (OUD). |
| Public Health Departments | $Millions annually | Includes costs of prevention programs, public awareness campaigns, and surveillance of opioid-related deaths. |
Managing Opioid Prescriptions
Effective strategies for managing opioid prescriptions are crucial to mitigate the crisis. Healthcare providers can implement various measures to minimize risks.
- Prescribing Practices: A crucial aspect of mitigating opioid crisis-related issues involves limiting the duration and quantity of opioid prescriptions, prioritizing non-opioid pain management strategies, and thoroughly assessing patient risk factors. This approach necessitates meticulous documentation and close monitoring of patients’ pain levels, response to treatment, and potential for misuse.
- Patient Education: Patient education is paramount in preventing misuse and addiction. Patients must understand the risks associated with opioids, the importance of adherence to prescribed regimens, and the availability of alternative pain management options. Clear communication about potential side effects and the importance of reporting concerns is essential.
- Collaboration with Other Healthcare Professionals: Collaboration among healthcare professionals, including physicians, pharmacists, and mental health specialists, is essential to ensure comprehensive care for patients with chronic pain and those at risk of opioid misuse. Regular communication and shared decision-making processes are vital to coordinate treatment strategies and address individual patient needs.
Impact on Healthcare Worker Well-being
The opioid crisis takes a substantial toll on healthcare workers, contributing to increased stress, burnout, and compassion fatigue. Witnessing the suffering of patients struggling with addiction, dealing with overdose cases, and the emotional toll of these experiences profoundly impact their well-being. Creating supportive environments and providing resources for healthcare professionals are vital.
- Recognizing and Addressing Burnout: Healthcare systems must proactively recognize and address burnout among healthcare workers. This includes providing access to mental health resources, fostering a supportive work environment, and implementing strategies to manage workload and stress.
- Training and Support: Investing in training programs for healthcare workers on opioid misuse prevention, addiction treatment, and crisis intervention can significantly enhance their ability to provide effective care. Continued support and mentorship are crucial for maintaining their well-being.
- Establishing Support Systems: Healthcare facilities must establish support systems for healthcare workers, providing opportunities for peer support, counseling, and de-escalation strategies to address the emotional toll of working in this challenging environment.
Policy and Regulatory Changes
The opioid crisis, fueled by the widespread availability of generic opioids, necessitates a multifaceted approach to curtail misuse and addiction. Policy changes must address the entire supply chain, from manufacturing and distribution to prescribing and patient care. Effective strategies require a comprehensive understanding of the current regulatory landscape and its shortcomings, along with innovative solutions for preventing and treating opioid-related harm.
Potential Policy Changes to Address Generic Opioid Misuse
A critical aspect of combating the opioid crisis involves tightening regulations surrounding the production, distribution, and prescribing of generic opioids. Policy changes should focus on strengthening existing regulations and implementing new ones that address the unique challenges presented by generic opioids. This includes greater transparency in the manufacturing process and stricter controls on distribution channels.
- Restricting the marketing and promotion of generic opioids. Aggressive marketing campaigns, often targeting primary care physicians, can contribute to overprescribing. A move to restrict these campaigns, similar to regulations on other pharmaceuticals, can help curb the misuse and addiction crisis.
- Implementing stricter controls on the distribution of generic opioids. Increased scrutiny on the distribution network, including wholesalers and pharmacies, is crucial. This may involve mandatory reporting requirements for suspicious orders and the implementation of real-time tracking systems. A similar approach has proven successful in controlling the distribution of other controlled substances.
- Promoting alternative pain management strategies. Encouraging the use of non-opioid pain management techniques through educational programs and financial incentives can help shift the paradigm from opioid-first to a broader range of pain management options. This will decrease reliance on opioids and empower patients to explore healthier treatment avenues.
Improving Prescribing Practices and Patient Education, Generic opioids battle opioid epidemic
Prescribing practices and patient education are crucial elements in mitigating the opioid crisis. Effective strategies must include clear guidelines for prescribing opioids, including the use of lower dosages and shorter durations, as well as robust patient education programs.
- Establishing clear guidelines for opioid prescribing. Implementing standardized guidelines, such as the use of lower dosages and shorter durations for opioid prescriptions, can help curb over-prescription. This should be accompanied by rigorous training for physicians on safe prescribing practices.
- Developing comprehensive patient education programs. Educating patients about the risks of opioid misuse and addiction is essential. This education should encompass the potential side effects, risks of overdose, and alternative pain management strategies. These programs can also emphasize the importance of responsible medication storage and disposal. This approach aligns with similar initiatives for other prescription medications.
Comparing Existing Regulations on Opioid Prescriptions with Other Controlled Substances
Comparing existing regulations on opioid prescriptions with those on other controlled substances highlights the need for stronger controls. A critical review reveals significant differences in the stringency of regulations, which can contribute to the higher rates of opioid misuse and addiction.
- Identifying regulatory gaps. Analyzing the regulatory framework for opioid prescriptions reveals potential gaps compared to regulations on other controlled substances. This comparison may highlight specific areas needing strengthening to prevent misuse.
- Adopting stricter regulations on opioid prescribing. A closer look at existing regulations on other controlled substances, such as stimulants and depressants, reveals more stringent requirements for prescribing, dispensing, and tracking. These stricter regulations might offer valuable models for adjusting opioid prescription practices.
The Need for Stronger Regulations on Opioid Distribution
The current regulatory framework for opioid distribution needs substantial strengthening. A more robust system is required to prevent diversion and illicit trafficking. Current regulations frequently fail to account for the complex interplay between various stakeholders in the opioid distribution chain.
- Implementing stricter controls on opioid distribution. Implementing real-time tracking systems and stricter regulations on opioid wholesalers and pharmacies is necessary to curtail diversion and illicit trafficking. These measures aim to minimize the availability of opioids for misuse.
Potential Changes to the Regulatory Landscape of Generic Opioids
The regulatory landscape of generic opioids needs a comprehensive overhaul. Changes must address the specific challenges presented by the high volume of generic opioids, including their role in the opioid crisis. This includes measures to control the manufacturing and distribution of these drugs.
- Revisiting the approval process for generic opioids. Strengthening the approval process for generic opioids to include stricter scrutiny of potential risks and a more comprehensive evaluation of their potential for misuse can help prevent the widespread distribution of dangerous drugs.
- Establishing stricter quality control measures for generic opioids. This includes auditing manufacturing processes, tracking raw materials, and rigorously testing finished products for quality and purity. This will help guarantee that the products meet the required standards and reduce the likelihood of substandard or counterfeit drugs entering the market.
Public Awareness Campaigns

Raising public awareness about the risks of opioid misuse, particularly with generic opioids, is crucial in combating the epidemic. Effective campaigns can significantly impact individual choices and contribute to a safer community. Educating the public about the dangers of addiction, the potential for overdose, and the availability of alternative pain management strategies is paramount. By empowering individuals with knowledge, we can foster a culture of prevention and promote responsible use of prescription medications.
Campaign Design and Content
Public awareness campaigns need a multi-faceted approach, targeting diverse audiences with tailored messages. This includes leveraging various media channels to maximize impact and ensure accessibility. The core message should emphasize the potential dangers of generic opioid misuse and the availability of safer alternatives. Emphasizing the importance of responsible prescribing practices and patient education is also vital.
Campaign Materials
The campaign materials should be visually appealing and easy to understand. Printed materials, such as brochures and posters, can be distributed in community centers, pharmacies, and doctor’s offices. Online platforms, such as social media and websites, can reach a broader audience with engaging videos, infographics, and interactive tools. Community events, such as health fairs and workshops, can provide opportunities for direct interaction and education.
The language used should be clear, concise, and accessible to the general public. Avoiding medical jargon is essential for effective communication.
Effective Public Service Announcements (PSAs)
Effective PSAs should be short, impactful, and emotionally resonant. A PSA focusing on the personal stories of individuals who have struggled with opioid misuse can be highly effective. These stories can illustrate the devastating consequences of addiction and the importance of seeking help. Emphasizing the availability of treatment options and support services is crucial. Another effective approach is showcasing the impact of the epidemic on families and communities, highlighting the ripple effect of opioid misuse.
For example, a PSA could feature a family grappling with the loss of a loved one to an opioid overdose, emphasizing the importance of prevention and support.
Community Involvement
Community involvement is essential for the success of any public awareness campaign. Engaging community leaders, local organizations, and healthcare providers can amplify the message and ensure widespread reach. Collaborating with local businesses and schools can further expand the campaign’s reach. Partnering with organizations that already have established community connections can increase the campaign’s credibility and effectiveness. Involving community members in the development and implementation of the campaign can ensure that the message resonates with local needs and concerns.
Target Audience and Communication Strategies
| Target Audience | Communication Strategies |
|---|---|
| Young adults (18-25) | Social media campaigns, targeted online ads, partnerships with universities and colleges |
| Parents and caregivers | Community events, workshops, printed materials, collaborations with schools |
| Healthcare professionals | Educational materials, webinars, continuing medical education (CME) opportunities |
| Individuals with chronic pain | Information on alternative pain management options, resources for support groups, emphasis on safe medication use |
| First responders and emergency personnel | Training programs, educational materials on recognizing opioid overdose and administering naloxone |
End of Discussion
In conclusion, the generic opioids battle opioid epidemic is a multifaceted issue demanding comprehensive strategies. While affordability and accessibility of generic opioids are undeniable factors, their potential for misuse and the subsequent impact on addiction and overdose rates are critical concerns. Ultimately, effective solutions require a holistic approach, incorporating prevention strategies, alternative pain management options, and policy changes to ensure responsible use and minimize harm.