Gut microbiota and children with type 1 diabetes are deeply intertwined. The gut’s microscopic inhabitants play a crucial role in immune system development, and an imbalance, or dysbiosis, is suspected to contribute to autoimmune diseases like type 1 diabetes. This exploration delves into the complex relationship between the gut microbiota, the immune system, and the development of type 1 diabetes in children, examining everything from the composition of the gut microbiota in affected children to potential environmental factors and therapeutic strategies.
This article will investigate the composition and diversity of gut microbiota in children with type 1 diabetes, contrasting it with healthy children. We will also examine how environmental factors, such as diet and antibiotic use, might influence the gut microbiota and subsequently the risk of developing type 1 diabetes. Furthermore, the intricate interactions between the gut microbiota and the immune system, and potential therapeutic strategies to modulate the gut microbiota will be discussed.
Introduction to Gut Microbiota and Type 1 Diabetes in Children
The human gut is teeming with trillions of microorganisms, collectively known as the gut microbiota. This complex ecosystem plays a crucial role in human health, influencing everything from digestion and nutrient absorption to immune system development and overall well-being. A delicate balance within this ecosystem, known as eubiosis, is essential for optimal function. Disruptions to this balance, called dysbiosis, have been linked to various health issues, including autoimmune diseases.The gut microbiota significantly shapes the developing immune system.
It interacts with the immune cells in the gut lining, educating them to distinguish between harmless food components and potentially harmful pathogens. This interaction helps establish tolerance to food antigens and prevents inappropriate immune responses. This process is critical for preventing the development of autoimmune diseases, like type 1 diabetes. Disruptions in this interaction can lead to a dysregulated immune response, increasing the risk of developing autoimmune diseases.
Gut Microbiota and Immune System Development
The gut microbiota plays a pivotal role in shaping the immune system, starting early in life. Infants acquire their microbiota through various sources, including the mother during birth and breastfeeding, and from the environment. This acquisition of diverse microbial communities is crucial for the maturation of the immune system. The interactions between the immune system and the gut microbiota are complex and bidirectional.
The microbiota influences the development of immune cells, while the immune system regulates the composition and function of the microbiota.
Dysbiosis and Autoimmune Diseases
Dysbiosis, or an imbalance in the gut microbiota, has emerged as a potential contributor to the development of autoimmune diseases, including type 1 diabetes. This imbalance can result from various factors, including antibiotic use, diet, and environmental exposures. Dysbiosis is characterized by a reduction in beneficial bacteria and an overgrowth of potentially harmful ones, which can disrupt the normal immune response.
This disruption can lead to an inappropriate immune response targeting the body’s own tissues, a hallmark of autoimmune diseases.
Gut Microbiota and Type 1 Diabetes Etiology
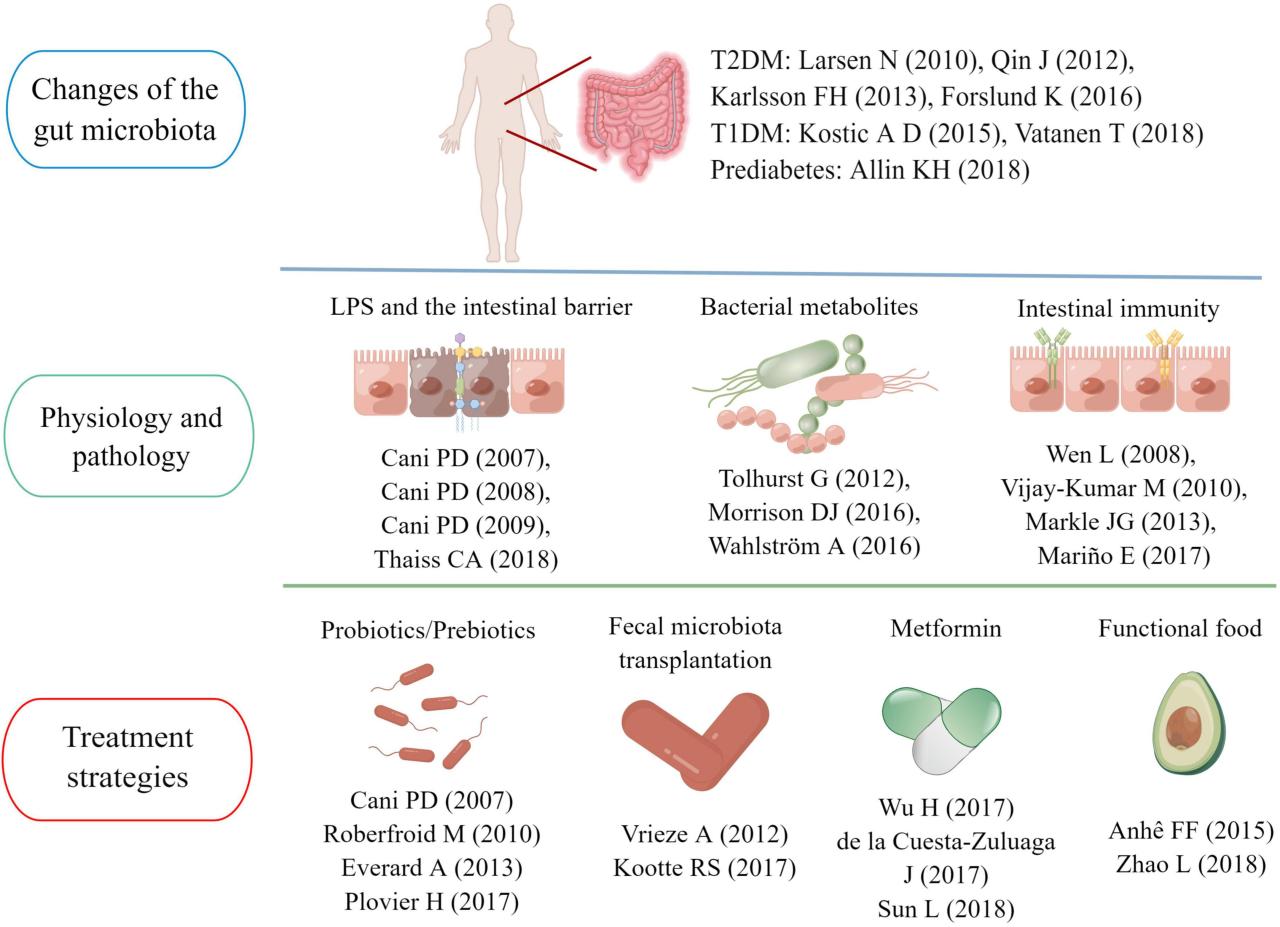
Research suggests that the gut microbiota may play a role in the etiology of type 1 diabetes in children. Studies have shown differences in the gut microbiota composition between children with type 1 diabetes and healthy controls. These differences are not fully understood, but they could indicate a potential link between the gut microbiota and the development of the disease.
Further research is needed to fully elucidate this relationship. The exact mechanisms through which the gut microbiota influences type 1 diabetes development remain unclear.
Comparison of Gut Microbiota Composition
| Feature | Healthy Children | Children with Type 1 Diabetes |
|---|---|---|
| Dominant Bacteria | Bacteroides, Prevotella, and Bifidobacterium species. | Potentially altered abundance of Bacteroides, Prevotella, and Bifidobacterium, possibly with increased levels of specific pathogenic bacteria. |
| Diversity | High diversity and richness of bacterial species. | Potentially reduced diversity and richness, leading to a less balanced microbial community. |
| Specific Microbial Groups | Presence of beneficial bacteria associated with immune regulation. | Potential decrease in beneficial bacteria and increase in bacteria associated with inflammation or immune dysregulation. |
Note: The composition and abundance of specific bacterial species can vary between individuals, making direct comparisons difficult.The table above provides a simplified comparison. Further research is needed to precisely determine the differences in the composition of gut microbiota in children with type 1 diabetes versus healthy controls. Understanding the specific microbial species and their interactions is critical for developing targeted interventions.
Microbiota Composition and Diversity in Children with Type 1 Diabetes
The intricate relationship between the gut microbiota and the development of type 1 diabetes in children is a subject of intense research. Understanding the composition and diversity of gut bacteria in these children is crucial for identifying potential risk factors and developing targeted interventions. Differences in microbial communities could play a pivotal role in the immune system’s response to environmental triggers, ultimately impacting disease progression.Research suggests that the gut microbiota in children with type 1 diabetes may exhibit distinct characteristics compared to those without the condition.
This includes variations in the abundance of certain bacterial species and, importantly, differences in the overall diversity of the microbial community. These variations could be influenced by genetic predisposition, environmental factors, or a combination of both.
Differences in Bacterial Species Abundance
Variations in the abundance of specific bacterial species between children with and without type 1 diabetes have been observed. Some bacterial species may be more prevalent in the gut microbiota of children with the condition, while others might be less abundant. These differences could be indicative of altered metabolic pathways or immune responses within the gut. For instance, a study might show increased levels of
Bacteroides* species in children with type 1 diabetes, potentially impacting the production of metabolites that influence immune function.
Diversity of Gut Microbiota at Different Ages
The diversity of the gut microbiota in children with type 1 diabetes may also vary across different age groups. Early-life microbial colonization patterns are crucial, and these patterns could differ between children who eventually develop type 1 diabetes and those who do not. For example, a study might reveal that the diversity of the gut microbiota in children with type 1 diabetes is lower during infancy compared to healthy controls, indicating potential early dysbiosis.
Furthermore, shifts in microbial composition might occur as the child grows older.
Recent research suggests a fascinating link between gut microbiota and type 1 diabetes in children. It’s a complex area, but the idea that the balance of bacteria in the gut might play a role is definitely intriguing. Thinking about how that might relate to other health conditions, I’ve been reading a lot about the connection between chronic pain and gut health lately.
For instance, a recent blog post, “not flaky I have migraines” not flaky i have migraines , highlights the potential impact of gut health on migraines. Ultimately, understanding how gut microbiota influences the development of type 1 diabetes in kids is a crucial area of ongoing study.
Potential Mechanisms of Microbial Influence
Specific microbial taxa could influence the development of type 1 diabetes through various mechanisms. For example, some bacteria might produce metabolites that directly or indirectly affect immune cells, potentially leading to an autoimmune response. Furthermore, the interaction between the gut microbiota and the host’s immune system could be crucial. A possible mechanism involves the disruption of the normal gut-immune homeostasis, potentially triggering autoimmunity.
Recent research into gut microbiota and its connection to type 1 diabetes in children is fascinating. But as summer approaches, and with summer camps tightening rules on vaccinations, summer camps tightening rules on vaccinations raises interesting questions about the overall health and immunity of children. Ultimately, understanding the complex interplay between gut microbiota, vaccinations, and childhood diseases like type 1 diabetes is crucial for developing better preventative strategies.
Another possibility is that certain bacteria can induce the production of inflammatory molecules that could contribute to the development of type 1 diabetes.
Prevalence of Bacterial Species in Children with Type 1 Diabetes
| Bacterial Species | Potential Functions |
|---|---|
| *Bacteroides fragilis* | Modulation of the immune response |
| *Faecalibacterium prausnitzii* | Anti-inflammatory effects |
| *Escherichia coli* | Production of various metabolites |
| *Bifidobacterium bifidum* | Immunomodulatory effects |
| *Lactobacillus acidophilus* | Production of antimicrobial substances |
Key Differences in Gut Microbial Diversity by Ethnic Group, Gut microbiota and children with type 1 diabetes
Differences in gut microbial diversity have been observed among different ethnic groups of children with type 1 diabetes. These differences might reflect variations in dietary habits, environmental exposures, and genetic backgrounds. For example, a study might show that the gut microbiota of children of Asian descent with type 1 diabetes exhibits distinct patterns compared to those of European descent.
This suggests that genetic and environmental factors interact in shaping the gut microbiota and its association with the development of type 1 diabetes.
| Ethnic Group | Key Differences in Gut Microbial Diversity |
|---|---|
| European Descent | Higher abundance of
|
| Asian Descent | Distinct patterns in
|
| African Descent | Potential variations in
|
Environmental Factors Influencing Gut Microbiota and Type 1 Diabetes: Gut Microbiota And Children With Type 1 Diabetes
The intricate relationship between the gut microbiota and type 1 diabetes in children is a burgeoning area of research. Understanding how environmental factors shape this microbiota is crucial for potentially preventing or managing this autoimmune disease. Environmental exposures, from diet to antibiotic use, can profoundly influence the composition and function of the gut microbiota, which in turn may impact the risk of developing type 1 diabetes.Environmental factors exert a powerful influence on the gut microbiota’s composition and diversity.
These factors interact with genetic predispositions, creating a complex interplay that contributes to the development of type 1 diabetes. Dietary choices, antibiotic exposure, and early-life experiences like breastfeeding all play pivotal roles in this intricate relationship.
Diet’s Impact on Gut Microbiota in Children
Dietary patterns significantly impact the gut microbiota in children. A diet rich in processed foods, sugar, and saturated fats is often associated with a less diverse and potentially less beneficial gut microbiota composition. Conversely, a diet rich in fiber, fruits, and vegetables can foster a more diverse and potentially healthier gut microbiota. The types and amounts of nutrients ingested directly influence the growth and activity of different bacterial species in the gut.
Antibiotic Use and Gut Microbiota
Antibiotic use, while crucial for treating infections, can disrupt the delicate balance of the gut microbiota. Antibiotics kill not only harmful bacteria but also beneficial bacteria, leading to a shift in the gut microbiota composition. This disruption can potentially increase the risk of developing type 1 diabetes, although the exact mechanisms are still being investigated. Frequent or prolonged antibiotic use in early childhood might contribute to a less robust and less diverse gut microbiota, which could potentially increase the risk of developing autoimmune diseases.
Early-Life Exposures and Gut Microbiota Development
Early-life exposures, particularly breastfeeding duration, significantly impact gut microbiota development in children. Breast milk provides a unique source of nutrients and prebiotics that promote the growth of beneficial bacteria. The longer a child is breastfed, the more established and diverse their gut microbiota is likely to be, which could have a protective effect against type 1 diabetes. The unique composition of breast milk can also help to create a microenvironment that is conducive to the growth of beneficial bacteria and inhibit the growth of potentially harmful ones.
Correlation Between Dietary Patterns and Gut Microbiota Composition
| Dietary Pattern | Gut Microbiota Composition | Potential Impact on Type 1 Diabetes Risk |
|---|---|---|
| High in processed foods, sugar, and saturated fats | Less diverse, potentially less beneficial bacteria | Potentially increased risk |
| High in fiber, fruits, and vegetables | More diverse, potentially more beneficial bacteria | Potentially decreased risk |
| Mediterranean diet (rich in fruits, vegetables, whole grains, and olive oil) | High diversity, presence of beneficial bacteria | Potentially decreased risk |
The table above highlights potential correlations between dietary patterns and gut microbiota composition. Further research is necessary to confirm these associations and establish causal relationships.
Environmental Factors and Type 1 Diabetes Risk
Environmental factors, including diet and antibiotic use, likely interact with genetic predisposition to influence the risk of developing type 1 diabetes. For instance, a child with a genetic predisposition to type 1 diabetes might be more susceptible to developing the disease if exposed to environmental factors that disrupt their gut microbiota, such as frequent antibiotic use or a diet low in fiber.
Early-life exposures can profoundly affect the development of a healthy gut microbiota, which could potentially reduce the risk of developing type 1 diabetes later in life. The evidence suggests that environmental factors, particularly those that impact the gut microbiota, play a significant role in the development of type 1 diabetes in susceptible individuals.
Gut Microbiota-Immune System Interactions in Type 1 Diabetes
The intricate relationship between the gut microbiota and the immune system is crucial for maintaining overall health. In the context of type 1 diabetes, this interaction becomes even more critical, as disruptions in this delicate balance can contribute to the development of the autoimmune disease. Understanding these interactions is essential for developing targeted therapies and preventive strategies.The gut microbiota plays a vital role in shaping the immune system, particularly during early life.
It educates the immune system to distinguish between harmless and harmful substances, promoting tolerance and preventing inappropriate immune responses. A dysregulated immune response, triggered by an imbalanced gut microbiota, can lead to the destruction of insulin-producing beta cells in the pancreas, a defining feature of type 1 diabetes.
Mechanisms of Gut Microbiota-Immune System Interaction
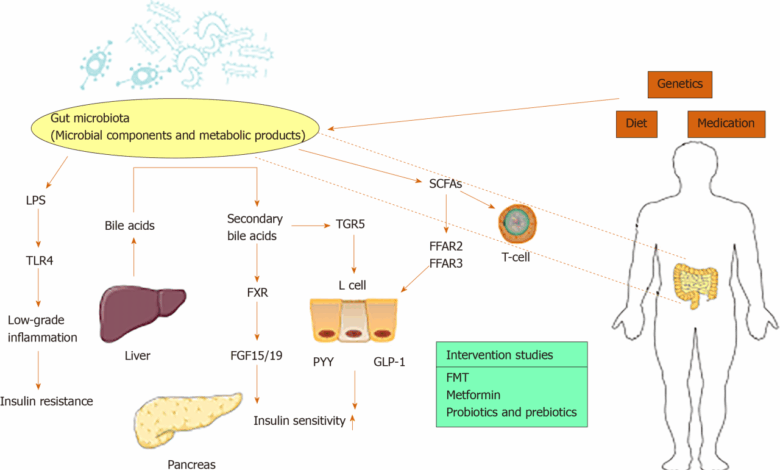
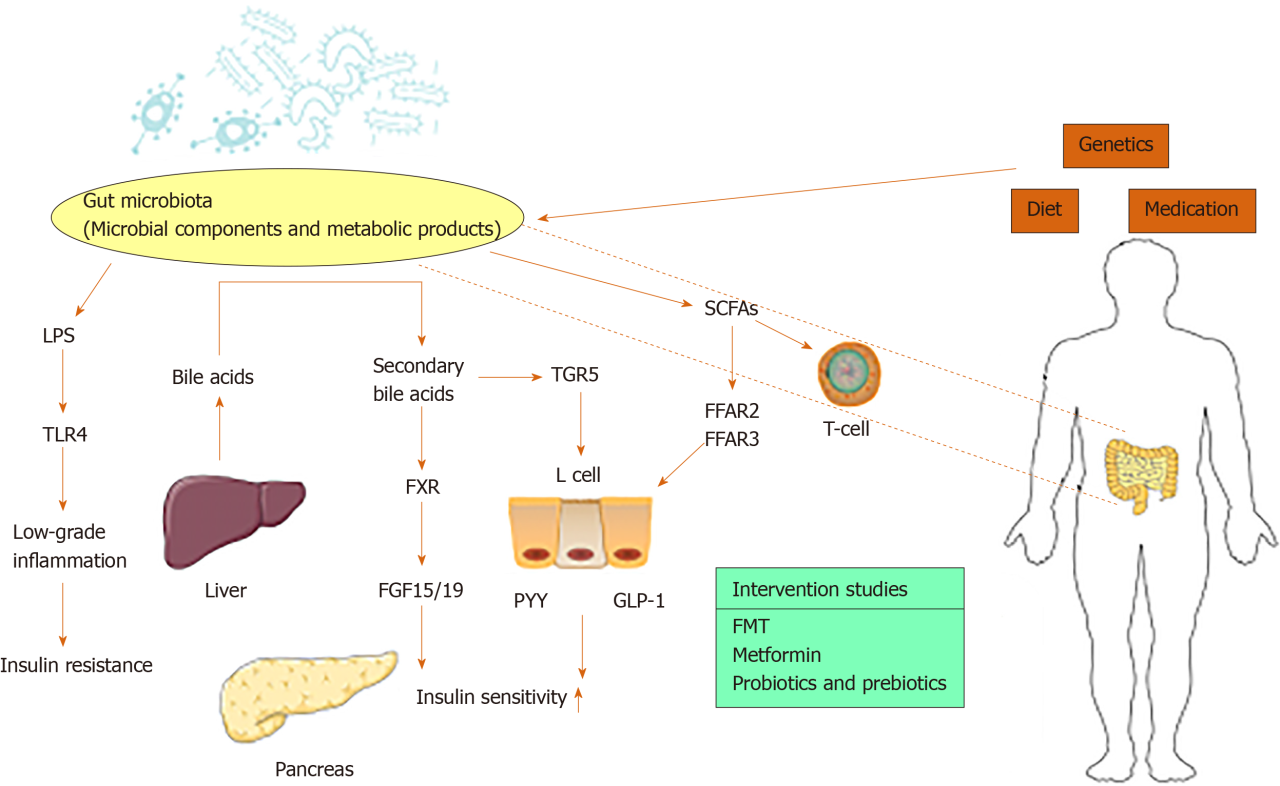
The gut microbiota interacts with the immune system through various mechanisms. These include direct contact with immune cells in the gut lining, the production of microbial metabolites, and the modulation of immune cell development and function. These interactions influence the development of immune tolerance, impacting the body’s ability to distinguish between self and non-self, ultimately affecting the risk of autoimmune diseases like type 1 diabetes.
Role of Microbial Metabolites in Modulating Immune Responses
Specific microbial metabolites, such as short-chain fatty acids (SCFAs), play a critical role in modulating immune responses. SCFAs, produced by certain gut bacteria, can influence the activity of immune cells, such as T regulatory cells (Tregs), which play a key role in suppressing immune responses. Disruptions in the production or utilization of SCFAs can lead to an imbalance in immune regulation, potentially increasing the risk of autoimmunity.
Recent research highlights the fascinating connection between gut microbiota and children with type 1 diabetes. It’s a complex area, but the interplay of these gut bacteria and the immune system seems crucial. Interestingly, similarly, it’s important to remember that RA patients need to be screened for ear problems, as detailed in this excellent article ra patients need to be screened for ear problems.
This emphasizes the broader need for comprehensive health checks across various conditions, which, in turn, has implications for the research into the gut microbiota and its role in type 1 diabetes in children.
Potential Pathways for Gut Microbiota Dysbiosis and Autoimmunity
Gut microbiota dysbiosis, characterized by an imbalance in the composition and diversity of gut bacteria, could trigger autoimmunity in type 1 diabetes through various pathways. For example, an overgrowth of certain bacteria or a decrease in beneficial bacteria can lead to the production of pro-inflammatory molecules, increasing the likelihood of immune system activation against pancreatic beta cells. Furthermore, altered metabolic activity of the microbiota can result in the production of antigens that resemble self-antigens, leading to the development of autoreactive T cells.
Influence of Gut Microbiota on Immune Cell Development and Function
The gut microbiota influences the development and function of immune cells, particularly in the gut-associated lymphoid tissue (GALT). Changes in the gut microbiota composition can affect the maturation and differentiation of various immune cells, including T cells and B cells. These altered immune cell populations can contribute to the development of an autoimmune response against pancreatic beta cells.
Interactions Between Specific Bacterial Species and Immune Cells
The table below summarizes the known interactions between specific bacterial species and immune cells in the gut. This information highlights the complex relationship between bacterial communities and immune responses in the gut, and how these can be altered in individuals with type 1 diabetes.
| Bacterial Species | Immune Cell Type | Interaction |
|---|---|---|
| Bacteroides fragilis | T regulatory cells (Tregs) | Production of anti-inflammatory metabolites, promoting immune tolerance |
| Escherichia coli | Various immune cells | Production of pro-inflammatory molecules, potentially triggering immune responses |
| Lactobacillus species | Various immune cells | Production of anti-inflammatory metabolites, promoting immune tolerance |
Therapeutic Strategies Targeting Gut Microbiota in Type 1 Diabetes
The intricate interplay between the gut microbiota and the immune system is increasingly recognized as a crucial factor in the development and progression of type 1 diabetes (T1D) in children. Understanding the composition and function of the gut microbiota, along with identifying potential therapeutic strategies to modulate it, is vital for improving outcomes and potentially preventing the onset of T1D.
This exploration focuses on potential interventions to influence the gut microbiota in children with T1D, emphasizing prebiotics, probiotics, and fecal microbiota transplantation.Current research suggests that an imbalance in the gut microbiota, often referred to as gut dysbiosis, might contribute to the autoimmune response leading to T1D. Restoring a healthy gut microbiota composition could potentially mitigate the disease’s progression or even prevent its onset.
The following sections delve into potential therapeutic strategies to achieve this goal.
Potential Strategies to Modulate Gut Microbiota Composition
Strategies for modifying gut microbiota composition aim to shift the balance towards a healthier profile. These strategies can include the use of prebiotics, probiotics, and even fecal microbiota transplantation. These interventions offer the potential to influence the immune system, reduce inflammation, and promote a more balanced gut microbial environment.
Prebiotics and Probiotics in Modifying Gut Microbiota
Prebiotics are non-digestible food ingredients that selectively stimulate the growth and/or activity of beneficial bacteria in the colon. Probiotics are live microorganisms, which, when administered in adequate amounts, confer a health benefit to the host. Both prebiotics and probiotics have shown promise in modifying gut microbiota composition and potentially mitigating the risk of T1D development. For example, certain prebiotic fibers, like inulin, have been associated with improved gut health in various studies.
Similarly, specific probiotic strains, like Lactobacillus and Bifidobacterium species, have demonstrated potential to reduce inflammation and improve immune responses.
Role of Fecal Microbiota Transplantation
Fecal microbiota transplantation (FMT) involves transferring fecal material from a healthy donor to a recipient with a dysbiotic gut. This approach aims to introduce beneficial microbes into the recipient’s gut, potentially restoring a more balanced microbiota. Early studies suggest that FMT may be a promising strategy for treating gut dysbiosis in children with T1D, although more research is needed to fully understand its efficacy and safety in this specific population.
Comparison of Prebiotic and Probiotic Interventions
| Intervention | Mechanism of Action | Potential Benefits | Potential Drawbacks |
|---|---|---|---|
| Inulin-type fructans | Stimulate growth of beneficial bacteria, like Bifidobacteria and Lactobacilli | Improved gut health, reduced inflammation | Potential for gas production, bloating |
| Lactobacillus rhamnosus GG | Modulate immune response, reduce inflammation | Improved gut barrier function, reduced intestinal permeability | Potential for mild side effects in some individuals |
| Bifidobacterium bifidum | Enhance immune system, promote a healthier gut environment | Improved gut health, reduced inflammation, potentially modulate immune responses | Potential for mild side effects in some individuals |
Potential Strategies to Restore a Healthy Gut Microbiota Composition
Restoring a healthy gut microbiota composition in children with T1D involves multiple approaches, including dietary interventions, prebiotic and probiotic supplementation, and in some cases, FMT. These interventions aim to shift the gut microbiota towards a more balanced and beneficial composition. For instance, a diet rich in fiber and diverse fruits and vegetables can potentially promote the growth of beneficial bacteria.
Furthermore, strategic use of prebiotics and probiotics could provide targeted support for the establishment of a healthier gut microbiome. Finally, ongoing research into the long-term effects of FMT on gut microbiota composition and immune function is crucial to fully understanding its potential in this context.
Future Research Directions
Unraveling the intricate connection between gut microbiota and type 1 diabetes in children requires a proactive approach to future research. Current knowledge, while providing valuable insights, leaves crucial gaps in our understanding. Further investigation into the dynamic interplay between diet, gut microbiota, and the development of the disease is essential. Exploring potential therapeutic interventions targeting gut microbiota composition holds promise for mitigating the progression and severity of type 1 diabetes.
Knowledge Gaps in Understanding Gut Microbiota’s Role
The complex interplay between the gut microbiota and the immune system in the context of type 1 diabetes remains largely unexplored. Specific mechanisms by which certain microbial species or metabolites influence immune cell development and function in children are not fully elucidated. Further research is needed to determine the precise timing of gut microbiota dysbiosis in relation to the onset of type 1 diabetes, as well as the specific microbial signatures associated with different disease stages.
Investigating Diet-Microbiota-Diabetes Interactions
Dietary patterns, particularly during early childhood, significantly impact gut microbiota composition. Investigating the impact of specific dietary components, such as prebiotics, probiotics, and dietary fibers, on gut microbiota modulation and its relationship to type 1 diabetes risk is crucial. A deeper understanding of the mechanisms linking specific dietary choices, gut microbiota alterations, and the development of autoimmune responses in children is essential.
Research Strategies for Modulating Gut Microbiota
Exploring various strategies for modulating gut microbiota in children with type 1 diabetes is a promising avenue for therapeutic interventions. These strategies could involve prebiotic and probiotic supplementation, fecal microbiota transplantation, or dietary interventions tailored to specific microbial imbalances. Assessing the safety and efficacy of these approaches in preventing or delaying disease onset requires rigorous clinical trials.
Potential Future Research Studies
| Research Area | Specific Research Question | Potential Methodology |
|---|---|---|
| Impact of Early-Life Diet | How does early introduction of specific foods impact the gut microbiota and subsequent risk of type 1 diabetes? | Longitudinal cohort study following children from infancy to adolescence, tracking dietary intake, gut microbiota composition, and disease development. |
| Prebiotic/Probiotic Interventions | Can specific prebiotic or probiotic supplements modify the gut microbiota and improve immune responses in children at high risk of type 1 diabetes? | Randomized controlled trials comparing intervention groups receiving prebiotics/probiotics to control groups receiving placebo or standard care. |
| Fecal Microbiota Transplantation | Is fecal microbiota transplantation a viable approach for restoring a healthy gut microbiota and mitigating disease progression in children with type 1 diabetes? | Pilot studies with a small number of participants to assess safety and preliminary efficacy. |
| Longitudinal Tracking of Changes | How do changes in gut microbiota composition correlate with changes in immune responses over time in children with type 1 diabetes? | Longitudinal studies tracking gut microbiota and immune markers over several years in a large cohort of children with type 1 diabetes. |
Importance of Longitudinal Studies
Longitudinal studies that follow children from birth or early childhood through the development of type 1 diabetes are crucial. These studies allow researchers to track changes in gut microbiota composition and immune responses over time. By examining these dynamic interactions, a more complete understanding of the causal pathways linking gut microbiota dysbiosis to type 1 diabetes can be achieved.
This approach is particularly valuable in identifying early biomarkers and potential intervention points.
Closure
In conclusion, the interplay between gut microbiota and type 1 diabetes in children is a fascinating and complex area of research. While we’ve learned a great deal about the potential role of gut microbiota dysbiosis in the development of the disease, much remains unknown. Future research is crucial to unraveling the precise mechanisms and developing targeted interventions, potentially including dietary modifications, prebiotics, and probiotics.
Further longitudinal studies are essential to track changes in gut microbiota and immune responses over time, helping us to understand the long-term impact of these factors on children with type 1 diabetes.