Half of opioid prescriptions go to people with depression mood disorders. This alarming statistic highlights a critical intersection between mental health and substance use. People experiencing depression and other mood disorders often face significant challenges, sometimes turning to opioids for relief. This complex issue necessitates a nuanced understanding of the factors driving this connection, the potential risks, and ultimately, the strategies for improved care and support.
Understanding the prevalence of depression and mood disorders, alongside the trends in opioid prescription practices, is crucial. This includes examining potential biases in prescription practices, analyzing current guidelines, and comparing regional differences. We will explore the overlapping health issues, looking at potential risk factors and comorbidity. Different treatment approaches and interventions will also be considered, from integrated care models to collaborative care strategies.
The public health implications and policy recommendations will be discussed, alongside illustrative case studies that emphasize the importance of individualized treatment plans.
Prevalence and Impact of Depression and Mood Disorders
Depression and mood disorders are significant public health concerns, impacting millions worldwide. These conditions affect not only the individual but also their families, communities, and the economy. Understanding their prevalence, impact, and contributing factors is crucial for developing effective prevention and treatment strategies.Understanding the scale of depression and mood disorders is vital for allocating resources and shaping public health initiatives.
Numerous studies have consistently shown a substantial burden on individuals and society. The impact extends far beyond the immediate experience of distress, affecting relationships, work productivity, and overall well-being.
Prevalence of Depression and Mood Disorders
Depression and mood disorders are prevalent across various demographics. Studies consistently indicate that a significant portion of the population experiences these conditions at some point in their lives. Estimates suggest that approximately 10-20% of adults will experience a depressive episode within a given year. Furthermore, the lifetime prevalence of mood disorders, including major depressive disorder and bipolar disorder, is considerably higher, affecting a substantial portion of the population throughout their lives.
Impact of Depression and Mood Disorders
The impact of depression and mood disorders is multifaceted, affecting individuals’ lives in various ways. These conditions can significantly impair daily functioning, impacting individuals’ ability to perform at work or school. The social consequences are also substantial, potentially leading to strained relationships, social isolation, and diminished quality of life. The economic burden is substantial, with lost productivity, increased healthcare costs, and reduced economic output.
Contributing Factors to Depression and Mood Disorders
Several factors contribute to the development of depression and mood disorders. Genetic predisposition plays a role, with individuals having a higher risk if family members have a history of these conditions. Environmental factors, including stressful life events, traumatic experiences, and social isolation, can also increase vulnerability. Chronic medical conditions, substance abuse, and certain medications can also contribute to the development of mood disorders.
For example, individuals experiencing chronic pain conditions often have an increased risk of developing depression, illustrating the complex interplay between physical and mental health.
Successful Interventions and Support Systems
Numerous interventions and support systems are available to help individuals with depression and mood disorders. Cognitive Behavioral Therapy (CBT) is a widely recognized and effective approach, helping individuals identify and modify negative thought patterns. Medication, when appropriate, can be a crucial component of treatment, especially in severe cases. Support groups provide a platform for individuals to connect with others experiencing similar challenges, offering valuable peer support and a sense of community.
Early intervention and access to mental healthcare are critical in improving outcomes and preventing the long-term impact of these conditions. Examples include community-based programs, school-based mental health initiatives, and increased awareness campaigns aimed at destigmatizing mental health issues.
Correlation Between Opioid Prescription Rates and Demographics
The relationship between opioid prescription rates and demographic factors is complex and requires careful consideration. While correlating opioid prescription rates with demographics can offer insights into potential risk factors, it’s crucial to understand that correlation does not imply causation.
| Demographic Factor | Potential Correlation with Opioid Prescription Rates | Example |
|---|---|---|
| Age | Higher rates among middle-aged adults, potentially related to chronic pain conditions | A study in a specific region found a higher rate of opioid prescriptions among individuals aged 45-64. |
| Gender | Potential differences in reported pain levels and treatment approaches | Some studies suggest that women may be more likely to receive opioid prescriptions for chronic pain. |
| Location | Regional variations in healthcare access and prescribing practices | Rural areas might have lower access to mental healthcare, potentially leading to higher rates of opioid prescriptions for pain management, even when mental health concerns exist. |
Opioid Prescription Practices and Trends: Half Of Opioid Prescriptions Go To People With Depression Mood Disorders
The overprescription of opioids, a significant public health concern, has led to a crisis of addiction and overdose deaths. Understanding the factors contributing to this trend, the biases within prescribing practices, and the efficacy of current guidelines is crucial for mitigating this crisis. This exploration delves into the complexities surrounding opioid prescriptions, examining regional variations, monitoring methods, and the need for comprehensive solutions.High opioid prescription rates are often attributed to various factors.
Physicians may prescribe opioids due to perceived efficacy in managing pain, a desire to avoid litigation, or a lack of alternative pain management options. Furthermore, patient expectations and demands for pain relief, along with inadequate pain assessment and management training, play a significant role in the issue.
Factors Contributing to High Opioid Prescription Rates
Several factors contribute to the high rates of opioid prescriptions in the general population. These include a tendency to favor quick fixes over long-term pain management strategies, and a lack of readily available, effective non-opioid alternatives. Further, patient expectations and demands for immediate relief often influence prescribing decisions.
- Physicians’ perception of efficacy: Physicians may overestimate the effectiveness of opioids for chronic pain, particularly when faced with limited knowledge of non-opioid treatments. This perception is often influenced by pharmaceutical marketing and limited access to comprehensive pain management education.
- Patient expectations and demands: Patients often expect opioids to provide immediate and significant pain relief, contributing to the demand for these medications. The lack of awareness about potential side effects and long-term consequences further fuels this demand.
- Lack of alternative pain management options: Limited access to non-opioid pain management options, such as physical therapy, counseling, or alternative therapies, often results in opioids being the primary solution. This lack of alternative options may be due to financial constraints or geographical limitations.
Potential Biases and Inaccuracies in Opioid Prescription Practices
Several biases and inaccuracies can influence opioid prescribing practices. These include implicit biases in physicians’ decision-making, misdiagnosis of chronic pain conditions, and the influence of pharmaceutical industry marketing. Inaccurate pain assessment and the failure to address underlying mental health conditions can also lead to overprescription.
- Implicit bias in physician decision-making: Unconscious biases can lead to variations in opioid prescriptions based on patient demographics or perceived risk factors. For instance, physicians may be more likely to prescribe opioids to patients who are perceived as less likely to misuse them, or who are perceived as being in more need of pain relief.
- Misdiagnosis of chronic pain conditions: Inaccurate diagnosis of chronic pain conditions can result in inappropriate opioid prescriptions. A thorough evaluation of the patient’s medical history and pain characteristics is essential for proper diagnosis and treatment planning.
- Influence of pharmaceutical industry marketing: Pharmaceutical marketing efforts can influence physicians’ prescribing habits and lead to overprescription. It is important for healthcare providers to be aware of potential biases stemming from these marketing efforts.
Current Opioid Prescription Guidelines and Regulations
Current opioid prescription guidelines and regulations aim to minimize risks and promote safe prescribing practices. These guidelines often emphasize comprehensive pain assessment, the use of non-opioid alternatives, and patient education.
It’s alarming that half of opioid prescriptions end up with people struggling with depression and mood disorders. This highlights a serious need for alternative pain management strategies. Considering how bogus some of the advertised remedies were, like those how bogus were trump vitamins , it makes one wonder about the effectiveness of the current approach. Ultimately, addressing the underlying mental health issues alongside proper pain management is crucial for a healthier society.
- Comprehensive pain assessment: Guidelines emphasize the importance of thoroughly assessing a patient’s pain, considering both physical and psychological factors. This involves evaluating the nature and severity of pain, as well as the patient’s overall health.
- Use of non-opioid alternatives: Guidelines recommend utilizing non-opioid pain management strategies whenever possible. This includes physical therapy, counseling, and other non-pharmacological interventions.
- Patient education and monitoring: Guidelines emphasize the importance of educating patients about the risks and benefits of opioid therapy, and monitoring for signs of misuse or addiction.
Opioid Prescription Practices Across Different Regions or Populations
Opioid prescription practices vary across different regions and populations. These variations stem from factors such as cultural norms, access to healthcare, and the prevalence of chronic pain conditions. Understanding these variations is crucial for developing targeted interventions and strategies.
Monitoring and Tracking Opioid Prescriptions
Various methods are employed to monitor and track opioid prescriptions. These include prescription drug monitoring programs (PDMPs) and reporting systems, which help to identify patterns of misuse and overprescription.
It’s a sobering statistic: half of opioid prescriptions go to people with depression or mood disorders. This highlights the complex interplay between mental health and physical pain. And while we’re on the topic of unhealthy habits, consider how much of a nutritional disaster a Super Bowl food fest can be; check out how unhealthy pig out during super bowl for a deeper dive.
Ultimately, the connection between mental health struggles and the need for effective pain management remains a significant concern.
- Prescription Drug Monitoring Programs (PDMPs): PDMPs are state-level databases that track opioid prescriptions and other controlled substances. They allow healthcare providers to check for potential misuse and overprescription.
- Reporting Systems: Reporting systems track and analyze data on opioid-related adverse events, such as overdose deaths and hospitalizations. This data is used to identify trends and inform policy decisions.
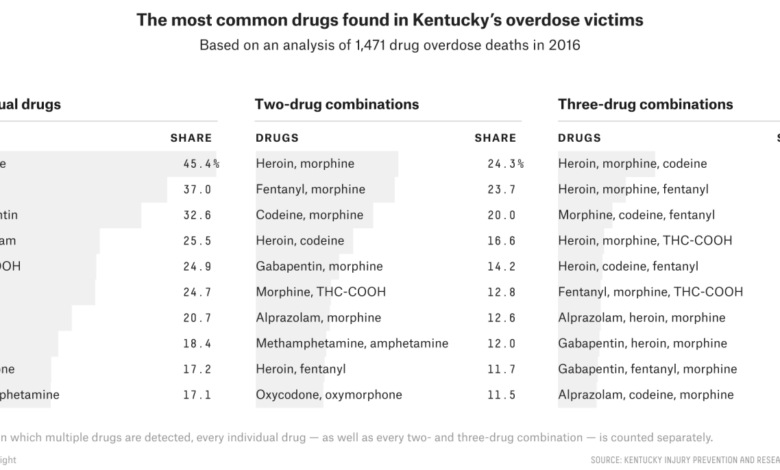
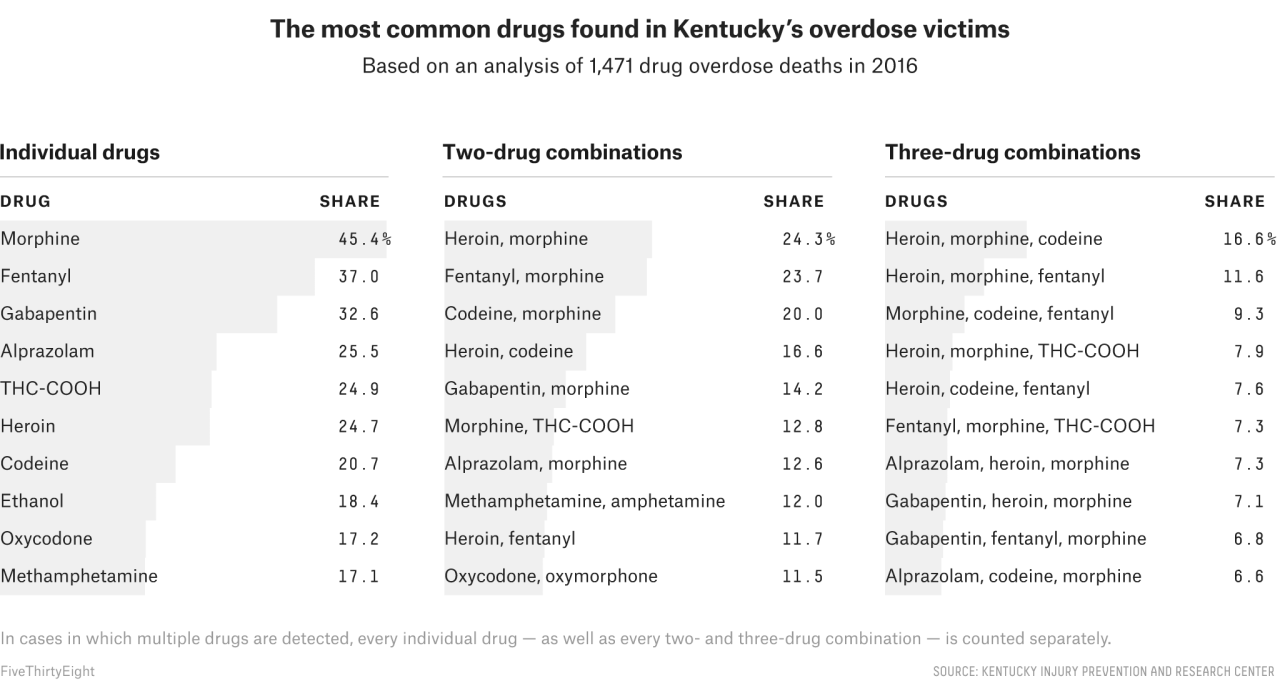
Opioid Prescription Types and Frequency
| Opioid Type | Frequency (Estimated, hypothetical example) |
|---|---|
| Hydrocodone | 40% |
| Oxycodone | 30% |
| Morphine | 15% |
| Fentanyl | 10% |
| Other | 5% |
Note: The table provides a hypothetical example of estimated frequency; actual figures may vary based on location and time period. Frequency can be influenced by factors like availability and regulations.
Overlapping Health Issues and Potential Linkages

The intersection of mental health conditions, particularly depression and mood disorders, and substance use disorders, including opioid misuse, is a complex and often overlooked area. Understanding the potential for co-occurrence is crucial for effective prevention and treatment strategies. The overlap between these conditions is not simply coincidental; rather, there are often interwoven biological and psychological factors that contribute to both.This complex interplay necessitates a multifaceted approach to care, acknowledging the interconnectedness of mental and physical health.
A deeper understanding of these relationships is vital for tailoring treatment plans that address both the opioid use disorder and the underlying mental health concerns.
Potential for Co-occurring Mental Health Conditions and Substance Use Disorders
Co-occurring disorders, also known as comorbidity, are prevalent in individuals with substance use disorders, including opioid use disorders. This overlap frequently involves mental health conditions like depression, anxiety, and post-traumatic stress disorder (PTSD). Individuals struggling with depression or mood disorders may turn to opioids for temporary relief from emotional distress, leading to a cycle of substance use and worsening mental health.
The use of opioids, in turn, can exacerbate existing mood disorders, creating a challenging feedback loop.
Underlying Biological and Psychological Factors
Biological factors such as genetic predisposition and neurochemical imbalances can increase vulnerability to both depression/mood disorders and opioid use disorders. Psychological factors, including prior trauma, stressful life events, and coping mechanisms, also play a crucial role in the development and maintenance of these conditions. For example, individuals with a history of trauma may be more susceptible to both depression and substance use disorders.
Potential for Comorbidity
Comorbidity, the simultaneous presence of two or more disorders, can significantly impact an individual’s overall health and treatment response. When depression or mood disorders co-occur with opioid use disorder, the treatment plan must address both conditions simultaneously to achieve optimal outcomes. The complexity of comorbidity necessitates a comprehensive assessment and treatment plan, involving collaboration among mental health professionals, addiction specialists, and other healthcare providers.
Potential Risk Factors for Opioid Use and Mental Health Disorders
| Potential Risk Factor | Opioid Use Disorder | Mental Health Disorders (e.g., Depression/Mood Disorders) |
|---|---|---|
| Family history of substance use disorders | High | Moderate |
| History of trauma or abuse | High | High |
| Chronic pain | High | Moderate |
| Social isolation | Moderate | High |
| Access to opioids | High | Low |
| Stressful life events | Moderate | High |
| Pre-existing mental health conditions | Moderate | High |
Note: The table illustrates potential risk factors. The presence of one factor does not guarantee the development of either condition.
Symptoms Indicating a Need for Further Assessment and Treatment
Individuals experiencing both opioid use disorder and mental health conditions may exhibit a range of symptoms. These symptoms may include persistent sadness, loss of interest in activities, changes in sleep patterns, appetite changes, fatigue, feelings of hopelessness, suicidal ideation, and increased opioid use. These symptoms may also include physical symptoms, such as decreased motor function, constipation, and nausea, which are often linked to opioid use.
Early identification and intervention are crucial to prevent worsening of symptoms and complications associated with the conditions.
Treatment Approaches and Interventions
Treating individuals with both depression/mood disorders and opioid use disorders requires a multifaceted approach. These co-occurring conditions often worsen each other, creating a vicious cycle that demands comprehensive and integrated care strategies. Effective treatment targets both the underlying mental health issues and the substance use disorder, aiming for long-term recovery and improved quality of life.Addressing these intertwined challenges necessitates a shift from siloed treatment models to integrated care approaches.
This holistic perspective recognizes the interconnectedness of mental health and substance use, acknowledging that one condition significantly impacts the other. By working collaboratively, healthcare providers can tailor treatment plans to address the unique needs of each patient, leading to more successful outcomes.
Integrated Care Approaches
Integrated care approaches recognize the importance of coordinating care between mental health specialists and addiction specialists. This collaborative effort is crucial for developing personalized treatment plans that address both the mood disorder and the opioid use disorder simultaneously. Such plans often involve a combination of therapies, medications, and support systems tailored to the individual’s specific needs and circumstances. This approach prioritizes patient-centered care, empowering individuals to actively participate in their recovery process.
Collaborative Care Models
Collaborative care models, often involving primary care physicians, mental health professionals, and addiction specialists, can significantly improve treatment outcomes for patients with co-occurring conditions. These models emphasize shared decision-making, where clinicians work together to develop and implement treatment plans that address both the immediate and long-term needs of the patient. The benefit of collaborative care is that it fosters a stronger support network, allowing for continuous monitoring and adjustments to the treatment plan as needed.
For example, a patient experiencing a relapse might receive immediate support from multiple specialists working together, rather than being left to struggle alone.
Effective Treatment Strategies
Effective treatment strategies for patients with both depression/mood disorders and opioid use disorders encompass various modalities. These strategies prioritize a combination of therapies, medications, and support services, tailored to each individual’s unique needs. Evidence-based therapies like cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), and motivational interviewing are often utilized to address underlying mental health issues and substance use behaviors.
Examples of Effective Treatment Strategies
- Medication-Assisted Treatment (MAT): This approach combines medications, such as buprenorphine or naltrexone, with counseling and behavioral therapies to reduce cravings and withdrawal symptoms, making it easier for patients to engage in other treatments.
- Cognitive Behavioral Therapy (CBT): CBT helps patients identify and change negative thought patterns and behaviors associated with both depression and opioid use. This therapy equips individuals with coping mechanisms to manage cravings and triggers.
- Dialectical Behavior Therapy (DBT): DBT focuses on emotional regulation, distress tolerance, and interpersonal effectiveness, helping patients cope with intense emotions and improve relationships, which are often strained by both conditions.
- Support Groups: Support groups, such as Narcotics Anonymous or Alcoholics Anonymous, provide a safe space for individuals to share experiences, receive encouragement, and build a supportive community.
Treatment Modalities Table
| Treatment Modality | Description | Potential Benefits |
|---|---|---|
| Medication-Assisted Treatment (MAT) | Combines medications with counseling and behavioral therapies to reduce cravings and withdrawal. | Reduces cravings, eases withdrawal symptoms, improves engagement in other treatments. |
| Cognitive Behavioral Therapy (CBT) | Identifies and changes negative thought patterns and behaviors associated with depression and opioid use. | Develops coping mechanisms for cravings and triggers, improves emotional regulation. |
| Dialectical Behavior Therapy (DBT) | Focuses on emotional regulation, distress tolerance, and interpersonal effectiveness. | Improves emotional regulation, reduces impulsive behaviors, enhances relationships. |
| Support Groups | Provides a safe space for sharing experiences, encouragement, and building a supportive community. | Reduces isolation, fosters a sense of belonging, provides peer support. |
Public Health Implications and Policy Recommendations
The high rate of opioid prescriptions for individuals with depression and mood disorders presents a significant public health challenge. This intersection necessitates a multifaceted approach, addressing the underlying mental health needs while mitigating the risks associated with opioid use. The potential for addiction and overdose, coupled with the burden on healthcare systems, underscores the importance of proactive strategies.This necessitates a shift from simply treating symptoms to understanding the complex interplay between mental health conditions and substance use.
A comprehensive strategy encompassing prevention, early intervention, and accessible treatment options is crucial to effectively address this multifaceted issue.
Public Health Implications
The high rate of opioid prescriptions for those with depression and mood disorders has several significant public health implications. These include increased rates of opioid misuse, addiction, overdose deaths, and chronic health problems. This is exacerbated by the often overlapping symptoms of depression and chronic pain, leading patients to seek relief in opioids. The potential for misuse is significantly amplified by the nature of the conditions, and the accessibility of opioid prescriptions.
This emphasizes the need for a preventative approach.
Preventive Measures to Reduce Risk
Preventive measures are crucial in mitigating the risk of opioid misuse and addiction. Strategies that address the underlying mental health conditions are paramount. These strategies should prioritize early intervention and effective treatment options for depression and mood disorders. Educating both patients and healthcare providers about the risks of opioid misuse is also a vital aspect of preventative measures.
This should be accompanied by strategies for safe opioid prescribing practices and access to alternative pain management solutions.
Policy Recommendations, Half of opioid prescriptions go to people with depression mood disorders
- Strengthening Mental Health Care Access: Increased access to affordable and accessible mental health services is crucial. This includes expanding the availability of mental health professionals, increasing funding for community-based mental health programs, and implementing initiatives to destigmatize mental illness. This is vital to addressing the root causes of opioid use and ensuring appropriate management of pain and other symptoms without resorting to opioids.
- Promoting Non-Opioid Pain Management Options: Supporting the development and wider adoption of non-opioid pain management techniques is essential. This includes encouraging the use of physical therapy, cognitive behavioral therapy, and other evidence-based approaches. This reduces reliance on opioids as a primary treatment for chronic pain. Emphasis should be placed on education and training for healthcare professionals to utilize these alternative methods.
It’s alarming that half of opioid prescriptions go to those with depression and mood disorders. This highlights a serious need for alternative solutions, like exploring the benefits of better nutritional choices. A great system to consider is Europe’s food labeling system, specifically the nutri score the pros and cons of europes food labeling system , which might offer a framework for healthier food options that could potentially alleviate some of the mental health issues contributing to opioid use.
Ultimately, finding healthier ways to manage mental health alongside addressing the root causes of opioid dependency is crucial.
- Enhancing Prescribing Guidelines and Practices: Establishing stricter guidelines for opioid prescribing, particularly for patients with co-occurring mental health conditions, is necessary. These guidelines should emphasize shared decision-making between patients and healthcare providers, and should encourage the use of lower doses of opioids whenever possible. This should include strategies for monitoring patients and mitigating the risks of misuse.
- Expanding Substance Use Disorder Treatment Programs: Increasing access to and expanding the availability of evidence-based substance use disorder treatment programs is paramount. This includes ensuring the provision of comprehensive treatment options, including medication-assisted treatment (MAT), counseling, and support groups. These programs need to be readily available and tailored to meet the specific needs of individuals with co-occurring mental health conditions.
- Improving Patient Education and Awareness: Educational campaigns and public awareness initiatives are crucial to equip patients and the public with information about the risks associated with opioid misuse and addiction. This includes educating patients on safe opioid use, alternative pain management options, and the importance of seeking help for mental health concerns. This should target vulnerable populations, including those with depression and mood disorders.
Impact on Healthcare Systems
Implementing these recommendations will likely lead to reduced healthcare costs associated with opioid misuse and addiction. Reduced opioid-related hospitalizations, emergency room visits, and long-term care needs will contribute to financial savings. Additionally, improved mental health outcomes will lead to a decrease in the overall burden on healthcare systems. This can be achieved by prioritizing prevention and early intervention.
Examples of Successful Policies
Several jurisdictions have implemented successful policies to address similar issues. For example, some states have implemented stricter regulations on opioid prescribing, which have been correlated with decreased opioid-related overdose deaths. Others have expanded access to MAT, leading to improved outcomes for individuals struggling with opioid use disorder. These examples demonstrate the potential for successful policy implementation to positively impact healthcare systems and public health.
Illustrative Case Studies and Examples
Navigating the complex interplay between opioid prescriptions and depression/mood disorders requires a nuanced understanding of individual patient experiences. A one-size-fits-all approach simply won’t work. Effective management hinges on a deep dive into each patient’s unique circumstances, their specific needs, and the interplay between their mental health and physical well-being. Case studies offer invaluable insights into the challenges and the potential for positive outcomes.Careful assessment and personalized treatment plans are paramount in addressing the intertwined nature of these conditions.
Simply addressing one issue without acknowledging the other can lead to ineffective, even harmful, results. Understanding the specific triggers, symptoms, and responses of each patient is crucial to developing a comprehensive strategy that fosters healing and recovery.
Patient Assessment and Individualized Treatment Plans
A comprehensive patient assessment is critical for identifying the specific needs of individuals with both opioid prescriptions and mood disorders. This involves gathering detailed information about the patient’s medical history, including past and current diagnoses, medications, substance use history, and any relevant family history. Psychosocial factors, such as social support systems, living situations, and coping mechanisms, are also essential to consider.
The assessment should incorporate standardized instruments to measure the severity of depressive symptoms and the degree of opioid dependence. This data informs the creation of a personalized treatment plan, which is not a one-time event but a dynamic process.
Successful Patient Outcomes Using Specific Treatment Strategies
Successful outcomes often involve a multidisciplinary approach, integrating medication management, psychotherapy, and support groups. For instance, cognitive behavioral therapy (CBT) can help patients identify and modify negative thought patterns and behaviors related to both their depression and opioid use. Similarly, motivational interviewing can empower patients to take an active role in their recovery journey, fostering self-efficacy and promoting adherence to treatment plans.
These strategies can reduce the likelihood of relapse and improve overall well-being.
Role of Patient Support and Education in Recovery
Patient support and education play a pivotal role in the recovery process. Educating patients about the potential risks of opioid use, especially when combined with mood disorders, empowers them to make informed decisions. Support groups offer a safe and confidential environment for individuals to connect with others facing similar challenges. Shared experiences, encouragement, and practical strategies for coping can significantly contribute to a sense of community and hope.
Hypothetical Case Study
A 32-year-old woman, Sarah, presented with a history of major depressive disorder and a recent prescription for opioid pain medication following a surgical procedure. Initially, her symptoms seemed to improve with the opioid, but her depressive symptoms worsened. Sarah experienced increased anxiety, insomnia, and a loss of interest in activities she once enjoyed. The opioid use also led to social isolation and withdrawal from her support network.Her treatment involved a multidisciplinary approach.
A psychiatrist prescribed an antidepressant medication to address her depression. A therapist utilized CBT to help her identify and challenge negative thought patterns, address her emotional responses to pain, and develop healthy coping mechanisms. A support group offered a sense of community and provided strategies for managing cravings and triggers. The opioid prescription was gradually reduced under close medical supervision, with the aim of minimizing withdrawal symptoms.
Sarah was also provided with education on the potential risks of opioid use, especially when combined with depression. Sarah’s progress was closely monitored. Over time, her depressive symptoms lessened, and she reported a greater sense of well-being. She re-engaged in social activities and demonstrated increased resilience in managing her pain. The gradual tapering of the opioid medication, coupled with her active participation in therapy and support groups, allowed her to achieve a more balanced and sustainable recovery.
Final Wrap-Up
In conclusion, the significant link between opioid prescriptions and depression/mood disorders demands a comprehensive approach. Addressing this complex issue requires a multifaceted strategy involving improved mental healthcare access, addressing biases in prescription practices, and promoting integrated care models. Ultimately, the goal is to provide comprehensive support and effective treatment options for individuals struggling with both conditions. This complex issue demands continued research, public awareness, and policy changes to improve outcomes.