Having type 2 diabetes and heart disease doubles the risk of dementia, highlighting the crucial connection between these conditions. This isn’t just about numbers; it’s about understanding the complex interplay of factors affecting brain health. We’ll delve into the science behind this link, exploring risk factors, potential prevention strategies, and the latest research. This exploration aims to equip readers with knowledge to make informed choices about their well-being.
The link between type 2 diabetes, heart disease, and dementia is becoming increasingly clear. This blog post explores the underlying mechanisms, examines the risk factors, and discusses potential strategies to mitigate the risk of cognitive decline. Understanding these factors can help individuals and healthcare professionals alike to adopt preventative measures and support better outcomes.
Understanding the Link Between Type 2 Diabetes, Heart Disease, and Dementia
Type 2 diabetes, heart disease, and dementia are interconnected health issues that share common risk factors and underlying mechanisms. This exploration delves into the specific ways these conditions are linked, emphasizing the importance of understanding and managing risk factors for a healthier life.Type 2 diabetes is a chronic metabolic disorder characterized by elevated blood sugar levels. The body either doesn’t produce enough insulin or the body’s cells don’t respond properly to insulin, which is essential for transporting glucose from the bloodstream into cells for energy.
Over time, persistently high blood sugar damages blood vessels and nerves throughout the body, impacting various organs.
Mechanisms of Type 2 Diabetes Impact on the Body
High blood sugar damages blood vessels, leading to atherosclerosis, a condition where plaque builds up in the arteries. This buildup can narrow the arteries, reducing blood flow to vital organs. The impact on the heart, brain, and other organs is significant, leading to complications like heart disease, stroke, and kidney disease. Diabetic neuropathy, nerve damage caused by high blood sugar, can cause pain, numbness, and other symptoms.
Furthermore, poor blood circulation due to vascular damage can impact wound healing and increase the risk of infections.
Mechanisms of Heart Disease Development and Relationship to Diabetes
Heart disease, primarily coronary artery disease, involves the buildup of plaque in the arteries that supply blood to the heart. This plaque, comprised of cholesterol, fats, and cellular debris, gradually hardens and narrows the arteries, reducing blood flow to the heart muscle. Type 2 diabetes significantly accelerates the development of atherosclerosis. Elevated blood sugar levels promote inflammation and damage to blood vessel walls, making them more susceptible to plaque buildup.
High blood pressure, often associated with diabetes, further contributes to the stress on the heart and the progression of heart disease. The risk of heart attack and stroke is dramatically increased in individuals with both type 2 diabetes and heart disease.
Neurological Effects of Cardiovascular Disease, Having type 2 diabetes and heart disease doubles the risk of dementia
Cardiovascular disease, including heart disease and stroke, has profound neurological consequences. Reduced blood flow to the brain due to narrowed arteries can lead to stroke, a sudden interruption of blood supply to the brain, causing cell death and neurological deficits. Chronic hypertension, often a feature of both diabetes and heart disease, can damage blood vessels in the brain, increasing the risk of cognitive decline.
Inflammation, a key player in the development of both cardiovascular disease and some forms of dementia, contributes to neuronal damage and dysfunction. These effects can range from mild cognitive impairment to full-blown dementia.
Concept of “Doubled Risk”
The “doubled risk” refers to a significant increase in the likelihood of developing a specific condition when two risk factors are present. In the case of dementia, the presence of both type 2 diabetes and heart disease significantly elevates the risk of developing dementia compared to individuals with either condition alone. This multiplicative effect highlights the importance of addressing both conditions proactively.
Did you know that having type 2 diabetes and heart disease simultaneously doubles your risk of dementia? It’s a sobering statistic, especially when you consider how tempting those Super Bowl feasts can be. And let’s be honest, those “unhealthy pig outs” during the big game often involve a lot of high-fat, high-sodium foods that can contribute to both type 2 diabetes and heart disease.
This is a great reminder that checking out how unhealthy pig out during super bowl can reveal the detrimental impact of those celebratory meals. Ultimately, careful food choices can greatly influence your health, and this includes lowering the risk of dementia.
Risk Factor Comparison
| Risk Factor | Type 2 Diabetes | Heart Disease | Dementia |
|---|---|---|---|
| High Blood Sugar | High | Moderate | Moderate |
| High Blood Pressure | High | High | Moderate |
| High Cholesterol | Moderate | High | Moderate |
| Smoking | Moderate | High | Moderate |
| Obesity | High | High | Moderate |
| Lack of Physical Activity | Moderate | Moderate | Moderate |
Risk Factors and Protective Measures
Understanding the interplay between type 2 diabetes, heart disease, and dementia is crucial for developing effective preventative strategies. This section dives into the common risk factors associated with these conditions and highlights lifestyle modifications that can significantly reduce the likelihood of developing them. We’ll also explore potential protective measures and discuss how managing these conditions can potentially mitigate dementia risk.This exploration will cover a spectrum of risk factors, from modifiable lifestyle choices to underlying genetic predispositions.
Recent studies show that having type 2 diabetes and heart disease simultaneously doubles the risk of dementia, a truly concerning finding. Fortunately, there are fantastic resources available for those navigating similar health challenges. For those interested in learning more about fostering, exploring blogs like best foster parent blogs can offer valuable insights and support. Ultimately, understanding these health risks is crucial, and taking proactive steps to manage these conditions remains paramount.
By understanding these elements, individuals can proactively take steps to safeguard their health and well-being.
Common Risk Factors for Type 2 Diabetes and Heart Disease
Several factors contribute to the development of both type 2 diabetes and heart disease. These conditions often share overlapping risk factors, emphasizing the importance of a holistic approach to preventative care. A sedentary lifestyle, poor diet, and obesity are major contributors.
- Sedentary Lifestyle: A lack of physical activity reduces metabolism, increases insulin resistance, and contributes to weight gain, all of which increase the risk of developing both type 2 diabetes and heart disease. For example, individuals who spend prolonged periods sitting are more susceptible to these conditions.
- Poor Diet: A diet high in processed foods, saturated fats, and added sugars contributes to weight gain and insulin resistance, increasing the risk of type 2 diabetes. Similarly, a poor diet can lead to high cholesterol and blood pressure, increasing the risk of heart disease.
- Obesity: Excess body weight, particularly abdominal fat, is strongly linked to insulin resistance and increased risk of type 2 diabetes and heart disease. Obesity is a significant factor in the development of both conditions, highlighting the importance of maintaining a healthy weight.
- Family History: A family history of type 2 diabetes or heart disease increases an individual’s genetic predisposition to these conditions. If a parent or sibling has either of these conditions, the risk is elevated for the individual.
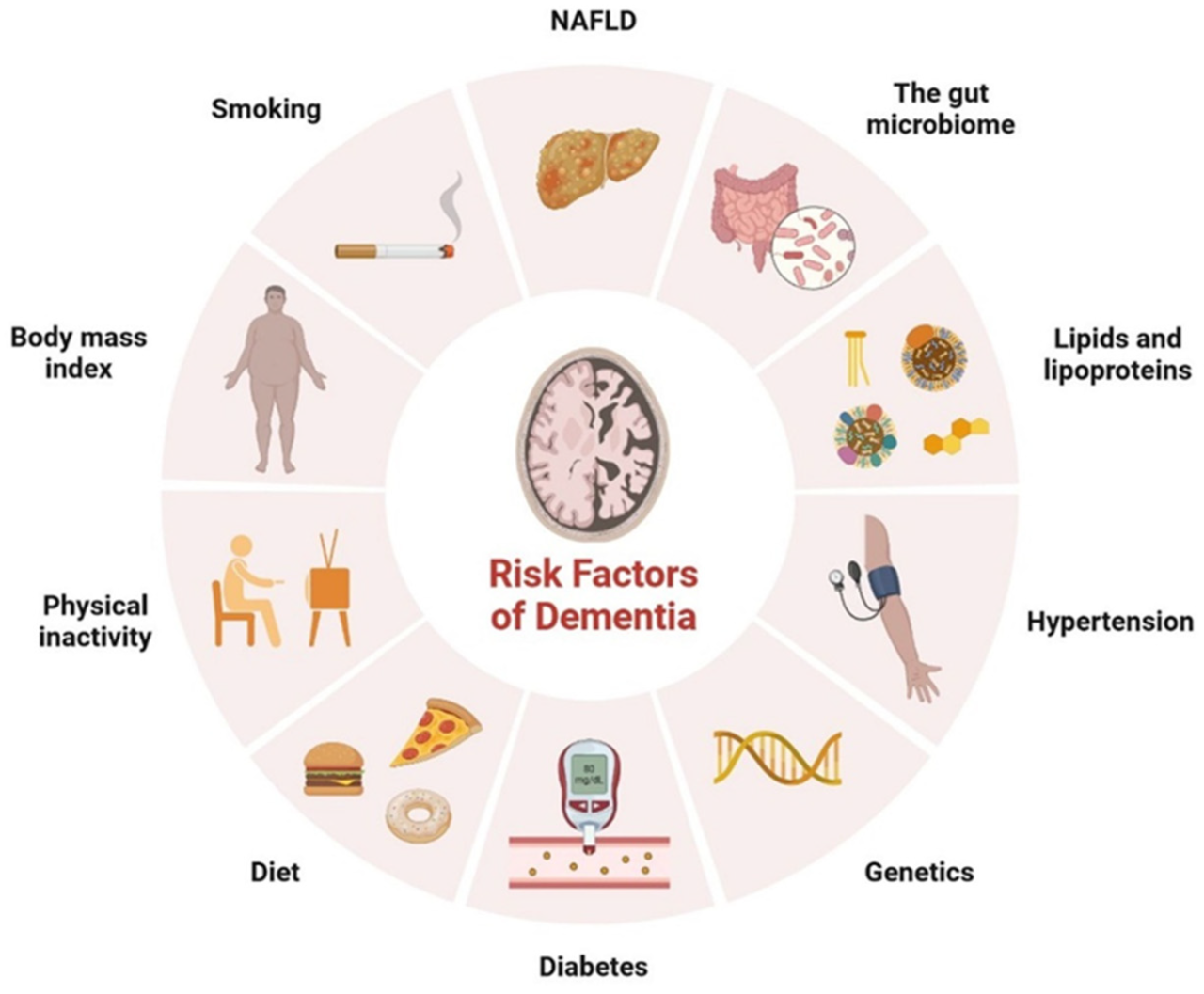
Potential Risk Factors for Dementia
Several factors can contribute to the development of dementia. While some risk factors are unavoidable, many are modifiable, offering opportunities for proactive health management.
- Age: The risk of dementia generally increases with age. While age is a non-modifiable risk factor, maintaining a healthy lifestyle throughout life can help mitigate its impact.
- Cardiovascular Disease: Conditions like high blood pressure, high cholesterol, and stroke significantly increase the risk of dementia. A history of heart disease or stroke puts an individual at greater risk of cognitive decline.
- Diabetes: Type 2 diabetes has been linked to a higher risk of cognitive decline and dementia. Individuals with poorly managed type 2 diabetes may experience increased risk of dementia.
- Smoking: Smoking is associated with increased risk of cardiovascular disease and stroke, both of which are associated with a higher risk of dementia.
- Unhealthy Diet: A diet lacking in essential nutrients or high in unhealthy fats, processed foods, and refined sugars can contribute to dementia risk. A poor diet impacts cognitive function.
Comparing Risk Factors for Type 2 Diabetes and Heart Disease
Type 2 diabetes and heart disease share several common risk factors, such as obesity, a sedentary lifestyle, and poor diet. However, some risk factors are more directly linked to one condition than the other. For example, high blood pressure and high cholesterol are more closely associated with heart disease.
Strategies for Managing Conditions to Potentially Reduce Dementia Risk
Managing type 2 diabetes and heart disease effectively can potentially reduce the risk of dementia. These strategies often involve similar lifestyle modifications.
- Regular Exercise: Physical activity helps manage blood sugar levels, improves cardiovascular health, and promotes overall well-being, potentially reducing dementia risk.
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean protein is essential for managing blood sugar, blood pressure, and cholesterol, all of which are crucial for preventing or managing type 2 diabetes, heart disease, and potentially dementia.
- Blood Pressure and Cholesterol Management: Maintaining healthy blood pressure and cholesterol levels is critical for both cardiovascular health and cognitive function. Regular monitoring and appropriate medication, when necessary, can significantly reduce the risk of dementia.
- Weight Management: Maintaining a healthy weight through diet and exercise can reduce the risk of developing type 2 diabetes, heart disease, and possibly dementia.
Lifestyle Changes for Prevention
Implementing lifestyle changes is crucial for preventing the development of type 2 diabetes, heart disease, and potentially dementia. The following table Artikels key lifestyle changes that can help in achieving this.
| Lifestyle Change | Description |
|---|---|
| Regular Exercise | Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities twice a week. |
| Balanced Diet | Prioritize whole grains, fruits, vegetables, and lean protein. Limit processed foods, saturated fats, and added sugars. |
| Stress Management | Practice stress-reducing techniques like yoga, meditation, or deep breathing exercises. |
| Smoking Cessation | Quit smoking to reduce the risk of cardiovascular disease and improve overall health. |
Dietary Recommendations
A healthy diet is essential for managing type 2 diabetes, heart disease, and potentially reducing dementia risk. These recommendations emphasize a balanced approach.
- Fruits and Vegetables: Incorporate a wide variety of fruits and vegetables into your daily diet. These provide essential vitamins, minerals, and antioxidants.
- Whole Grains: Choose whole grains over refined grains. Whole grains provide fiber, which helps regulate blood sugar levels.
- Lean Protein: Include lean protein sources like fish, poultry, beans, and lentils in your diet.
- Healthy Fats: Choose healthy fats like avocados, nuts, and olive oil. Limit saturated and trans fats.
- Limit Processed Foods: Minimize consumption of processed foods, sugary drinks, and excessive sodium intake. These foods can negatively impact health.
Research and Studies: Having Type 2 Diabetes And Heart Disease Doubles The Risk Of Dementia
Unraveling the intricate connection between type 2 diabetes, heart disease, and dementia requires a deep dive into the scientific literature. Numerous studies have meticulously investigated this triad of conditions, shedding light on the shared risk factors and underlying mechanisms. Understanding these research findings is crucial for developing effective preventative strategies and targeted interventions.
Summary of Relevant Studies
Research examining the link between type 2 diabetes, heart disease, and dementia employs a variety of methodologies. These studies often focus on identifying the factors that contribute to the increased risk of dementia in individuals with both conditions. The studies analyze the relationship between these diseases, focusing on common pathways and risk factors.
Study Methodologies
Several methodologies are employed in these studies. Observational studies, which follow a group of people over time, are frequently used to identify correlations between lifestyle factors, medical history, and the development of dementia. These studies can track the progression of the diseases and examine the impact of various risk factors. Furthermore, randomized controlled trials (RCTs) are employed to assess the effectiveness of interventions, such as lifestyle changes or medications, in reducing the risk of dementia.
The rigorous design of RCTs helps establish cause-and-effect relationships. For example, a cohort study might track individuals with type 2 diabetes and heart disease for a decade to observe the incidence of dementia.
Study Designs
Various study designs are employed to investigate this complex relationship. Prospective cohort studies follow individuals over time, monitoring their health and observing the development of dementia. Retrospective studies examine existing data to identify potential correlations. Meta-analyses combine data from multiple studies to draw broader conclusions. Each design has its strengths and limitations.
Recent studies show that having type 2 diabetes and heart disease simultaneously doubles the risk of dementia. It’s a sobering statistic, and as I’ve been researching this, it made me think about the countless families who are waiting to see if a certain chip will continue its development. Millions of families wait to see if chip will continue their hope for a healthier future, and unfortunately, these health concerns can significantly impact that hope.
This highlights the critical need for preventative measures and further research into these intertwined health risks.
For instance, a retrospective study can identify trends but might not be able to establish causality as definitively as a prospective study.
Populations Studied
The populations studied in these investigations often include individuals with a history of type 2 diabetes and/or heart disease. Some studies may focus on specific subgroups, such as those with particular genetic predispositions or those exhibiting certain lifestyle patterns. For example, a study might focus on middle-aged individuals with a family history of diabetes, heart disease, and dementia.
Outcomes Observed
Observed outcomes in these studies include the incidence of dementia, cognitive function scores, and markers of cardiovascular health. Changes in these factors over time are meticulously recorded and analyzed to establish correlations. For instance, a study might demonstrate a correlation between HbA1c levels (a measure of blood sugar control) and the rate of cognitive decline.
Contribution to Understanding Risk Factors
These studies have significantly contributed to our understanding of the risk factors for dementia in individuals with type 2 diabetes and heart disease. Researchers have identified specific factors, such as poor blood sugar control, high blood pressure, and elevated cholesterol levels, as crucial contributors to the development of both conditions and their link to dementia.
Key Findings from Different Studies
| Study | Methodology | Population | Outcomes | Contribution to Risk Factors |
|---|---|---|---|---|
| Study 1 (Example) | Prospective cohort study | Individuals with type 2 diabetes and heart disease | Increased incidence of dementia | Poor blood sugar control, high blood pressure, and elevated cholesterol levels |
| Study 2 (Example) | Meta-analysis | Diverse populations with both conditions | Strong correlation between cardiovascular risk factors and cognitive decline | Lifestyle interventions and medications to improve cardiovascular health |
Potential Mechanisms
The intricate relationship between type 2 diabetes, heart disease, and dementia isn’t a simple cause-and-effect chain. Instead, a complex web of biological pathways contributes to the increased risk of cognitive decline in individuals with these conditions. Understanding these mechanisms is crucial for developing targeted interventions and preventative strategies.The development of these conditions often involves shared biological pathways, highlighting the importance of addressing them holistically.
This section delves into the potential biological connections, focusing on the roles of inflammation, oxidative stress, vascular damage, specific proteins/molecules, and the impact of insulin resistance on brain health.
Inflammation
Chronic inflammation is a key player in the progression of type 2 diabetes, heart disease, and dementia. It’s a systemic response that can lead to cellular damage throughout the body, including the brain. Inflammation triggers the release of inflammatory molecules, which can damage blood vessels, impair insulin signaling, and contribute to cognitive decline. These inflammatory processes contribute to a cascade of events, eventually affecting the brain’s structure and function.
Oxidative Stress
Oxidative stress, characterized by an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to neutralize them, plays a critical role in the development of these conditions. ROS damage cellular components, including DNA, proteins, and lipids, leading to cellular dysfunction and inflammation. In the context of diabetes and heart disease, this damage can extend to the brain, contributing to cognitive decline.
Vascular Damage
Impaired blood flow and vascular damage are directly linked to the development of type 2 diabetes and heart disease. This damage, often caused by high blood glucose and high blood pressure, can restrict blood flow to the brain. Reduced blood flow deprives the brain of essential nutrients and oxygen, leading to neuronal damage and cognitive impairment. This connection highlights the importance of maintaining healthy blood vessels for overall brain health.
Specific Proteins/Molecules
Several proteins and molecules play critical roles in the interplay between these conditions. For example, the protein amyloid-beta, implicated in Alzheimer’s disease, has been shown to accumulate in the brains of individuals with type 2 diabetes. Furthermore, the inflammatory response, mediated by cytokines, may exacerbate the damage caused by vascular dysfunction.
Insulin Resistance
Insulin resistance, a hallmark of type 2 diabetes, has far-reaching effects beyond blood sugar regulation. This resistance affects the brain’s ability to utilize glucose for energy, which is essential for optimal cognitive function. Sustained insulin resistance can potentially disrupt neuronal signaling and contribute to cognitive decline, linking diabetes to dementia.
Clinical Implications and Future Directions
Understanding the interconnectedness of type 2 diabetes, heart disease, and dementia has profound implications for clinical practice. Early detection and proactive management of these conditions can significantly reduce the risk of cognitive decline and improve overall quality of life. This knowledge allows healthcare providers to shift from reactive treatment to preventative strategies, empowering patients to take control of their health journeys.
Clinical Practice Implications
The strong link between these conditions necessitates a paradigm shift in clinical practice. Healthcare providers must now consider these conditions as interconnected rather than separate entities. Routine screenings for both diabetes and cardiovascular risk factors should be integrated into the primary care model, including cognitive function assessments. Early intervention and close monitoring are crucial to mitigating the progression of these conditions.
For example, a patient with pre-diabetes should receive intensive lifestyle modification counseling to prevent the development of type 2 diabetes.
Preventative Measures for Healthcare Providers
Implementing preventative measures involves a multifaceted approach. Healthcare providers can proactively advise patients on lifestyle modifications, including dietary changes, regular exercise, and stress management techniques. Close monitoring of blood sugar levels, blood pressure, and cholesterol is essential for early detection and intervention. This includes incorporating cognitive function assessments as part of routine checkups, especially in high-risk individuals.
The use of preventive medications, like statins to lower cholesterol, and anti-diabetic medications, can also be considered.
Targeted Interventions
Targeted interventions can be developed based on individual patient risk profiles. Patients with a family history of these conditions or existing risk factors require more intensive monitoring and interventions. This may include specialized diabetes education programs, cardiac rehabilitation programs, and cognitive training exercises. For instance, a patient with a history of stroke and type 2 diabetes should be prioritized for intensive cardiovascular risk management and cognitive rehabilitation programs.
Future Research Areas
Further research is crucial to unravel the complex mechanisms linking these conditions and developing more effective prevention strategies. Studies focusing on the role of inflammation, oxidative stress, and vascular dysfunction are needed. Research on the efficacy of specific lifestyle interventions, such as intermittent fasting or specific dietary patterns, could provide valuable insights. Additionally, exploring the use of novel biomarkers for early detection of cognitive decline could pave the way for personalized preventative measures.
Finally, studies evaluating the long-term effects of combined interventions for these conditions are critical.
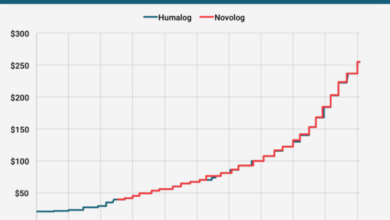
Current Treatment Options
| Condition | Treatment Options |
|---|---|
| Type 2 Diabetes | Lifestyle modifications (diet, exercise), oral medications (metformin, sulfonylureas), insulin therapy, and other injectable medications. |
| Heart Disease | Lifestyle modifications (diet, exercise), medications (statins, blood pressure medications, antiplatelet agents), cardiac rehabilitation, and surgical interventions (angioplasty, bypass surgery). |
| Dementia | Cognitive stimulation therapies, medications (in some cases), lifestyle interventions, and support groups. |
Potential Benefits of Early Intervention Strategies
| Intervention | Potential Benefits |
|---|---|
| Early detection and lifestyle modifications for prediabetes | Reduced risk of developing type 2 diabetes, improved cardiovascular health, and potentially reduced risk of cognitive decline. |
| Aggressive management of cardiovascular risk factors | Reduced risk of heart disease and stroke, improved cognitive function, and prolonged lifespan. |
| Cognitive stimulation programs | Improved cognitive function, reduced risk of dementia, and enhanced quality of life. |
Conclusive Thoughts
In conclusion, the link between type 2 diabetes, heart disease, and dementia is undeniable. This article has presented the current understanding of this complex relationship, emphasizing the importance of early detection, proactive management, and a holistic approach to well-being. By understanding the interconnectedness of these conditions, we can work towards preventative measures and improved patient outcomes.