How a 4th person was cured of HIV after stem cell treatments marks a significant advancement in medical science. This breakthrough offers a glimmer of hope for millions living with the virus, prompting questions about the potential of this innovative therapy. The journey to this remarkable outcome is complex, involving a unique stem cell procedure and a meticulous treatment plan.
Understanding the specifics, challenges, and ethical considerations surrounding this case is crucial for navigating the future of HIV treatment.
This article delves into the details of the fourth successful HIV cure through stem cell treatments. We’ll explore the science behind this groundbreaking approach, examine the specific procedure used, and discuss the potential mechanisms of action. The ethical implications and future research directions will also be considered, providing a comprehensive overview of this revolutionary treatment.
Introduction to HIV and Stem Cell Treatments
Human Immunodeficiency Virus (HIV) is a retrovirus that attacks and weakens the body’s immune system, specifically targeting CD4+ T cells. This weakening makes individuals susceptible to opportunistic infections and cancers. Without treatment, HIV can progress to Acquired Immunodeficiency Syndrome (AIDS). The virus’s ability to integrate its genetic material into the host cell’s DNA makes it exceptionally difficult to eradicate completely.
Overview of HIV, How a 4th person was cured of hiv after stem cell treatments
HIV infection typically progresses through several stages. Initially, individuals may experience flu-like symptoms, followed by a period with no apparent symptoms (clinical latency). As the virus continues to replicate and damage the immune system, symptoms associated with AIDS emerge, including severe infections and cancers. Antiretroviral therapy (ART) has significantly improved outcomes for HIV-positive individuals by suppressing viral replication and maintaining immune function.
Stem Cell Therapy Principles
Stem cell therapy leverages the regenerative potential of stem cells, which are undifferentiated cells capable of differentiating into various cell types. Hematopoietic stem cells (HSCs) are particularly relevant, as they give rise to blood cells, including immune cells. Stem cell transplantation can potentially replace damaged immune cells with healthy ones, restoring immune function.
Potential Mechanisms of Stem Cell Treatments for HIV
Stem cell treatments hold promise for HIV because they may potentially:
- Replace infected immune cells with healthy ones, reducing viral load.
- Stimulate the immune system to better fight the virus.
- Restore immune function by replenishing depleted immune cells.
Challenges and Limitations of Current HIV Treatments
While antiretroviral therapy (ART) has been highly effective in managing HIV, several challenges remain:
- ART requires lifelong adherence to medication schedules, which can be challenging for many patients.
- Some individuals develop drug resistance, rendering ART less effective.
- ART does not eliminate the virus from the body; it only suppresses replication.
Comparison of Traditional HIV Treatments and Stem Cell Therapies
| Feature | Traditional HIV Treatments (ART) | Stem Cell Therapies |
|---|---|---|
| Mechanism of Action | Suppresses viral replication by targeting different stages of the viral life cycle. | Replaces infected immune cells with healthy ones, potentially restoring immune function. |
| Duration of Treatment | Lifelong | Potentially one-time procedure, although long-term follow-up is crucial. |
| Side Effects | Can include nausea, fatigue, and liver problems. Some drugs may interact with other medications. | Potential side effects include graft-versus-host disease, rejection, and infections. |
| Viral Eradication | Does not eradicate the virus; it suppresses replication. | Potentially capable of eradicating the virus, though long-term data is still emerging. |
| Cost | Generally affordable with access to public health programs. | Significantly higher cost, often requiring extensive resources and specialized facilities. |
Case Study Details: How A 4th Person Was Cured Of Hiv After Stem Cell Treatments
The fourth individual’s successful HIV cure through stem cell treatment marks a significant advancement in the fight against this global health challenge. This case study delves into the specifics of the procedure, highlighting the crucial steps and considerations involved. Understanding these details provides valuable insights into the potential of stem cell therapy for HIV eradication.The choice of stem cell treatment in this case stemmed from a careful evaluation of the patient’s medical history and the limitations of other available therapies.
The patient’s response to prior treatments, along with their overall health condition, were key factors in determining the suitability of this particular approach. This highlights the personalized nature of medical interventions, emphasizing the importance of a thorough assessment before selecting any treatment modality.
Stem Cell Treatment Procedure
The specific stem cell treatment involved the use of hematopoietic stem cells (HSCs) derived from a healthy donor. This particular approach aimed to replace the patient’s infected immune cells with a new, healthy cellular system, effectively eliminating the reservoir of HIV in the body. The donor selection process was rigorous, focusing on matching the patient’s HLA type to minimize the risk of graft-versus-host disease.
Specific Type of Stem Cells and Sourcing
The hematopoietic stem cells (HSCs) were obtained from a bone marrow donation. The donor was carefully screened to ensure a suitable HLA match and overall health status, reducing the risk of complications. The bone marrow, rich in HSCs, was harvested from the donor under strict sterile conditions. The donor’s health was meticulously monitored throughout the process, adhering to ethical guidelines.
Treatment Process Timeline
This section Artikels the critical steps involved in the treatment process, from the initial preparation phase to follow-up care. The detailed timeline ensures a comprehensive understanding of the treatment journey.
| Phase | Description | Key Milestones |
|---|---|---|
| Pre-Treatment Preparation | Extensive medical evaluations, including viral load testing, complete blood counts, and other relevant diagnostic tests were performed. Anti-HIV medications were carefully managed to reduce viral load before stem cell transplant. |
|
| Stem Cell Transplant | The harvested stem cells from the donor were infused into the patient intravenously. Post-transplantation, the patient received immunosuppressive therapy to prevent graft-versus-host disease. |
|
| Post-Treatment Monitoring | The patient’s health was closely monitored for any signs of complications, including graft-versus-host disease, infection, or other adverse reactions. Regular blood tests and immune function assessments were performed. |
|
Potential Mechanisms of Action
The fourth successful HIV cure following stem cell treatment raises crucial questions about the underlying mechanisms. Understanding how these therapies might control HIV replication and achieve long-term suppression is critical for developing more effective strategies. This exploration delves into the potential pathways involved, comparing this case to previous attempts.Stem cell therapies, particularly those involving hematopoietic stem cell transplantation (HSCT), offer a novel approach to potentially eradicate HIV.
It’s incredible how a fourth person has been cured of HIV after stem cell treatments! This groundbreaking advancement in medical science is truly remarkable. While the specifics of the treatment protocol remain complex, understanding the supporting medications like clindamycin hydrochloride oral capsule is crucial for a complete picture. Further research into these complementary therapies will undoubtedly lead to even more effective strategies in fighting HIV.
The effectiveness of this method hinges on the intricate interplay between the transplanted cells, the patient’s immune system, and the virus itself.
Immune System Restoration
The transplanted stem cells, in conjunction with the immune system, play a crucial role in the potential eradication of HIV. Restoring the immune system is a vital aspect of controlling HIV, and the transplanted stem cells are thought to be instrumental in this process. They are expected to give rise to a fully functional immune system, which can more effectively combat the virus.
This replenishment of immune cells may directly or indirectly affect the virus’s ability to replicate and establish reservoirs. A healthy immune response is fundamental in suppressing viral activity and preventing disease progression.
Impact on Viral Reservoirs
A key challenge in HIV treatment is the persistence of viral reservoirs. These are latent viral DNA copies that hide within cells, like immune cells, and can reactivate, leading to viral rebound. Stem cell therapies aim to address these reservoirs in several ways. The transplanted cells, particularly those contributing to immune cell lineages, might eliminate cells harbouring the virus.
They could also influence the immune system’s ability to target and destroy these cells more effectively. Alternatively, the newly established immune response could exert pressure on the reservoir cells, preventing their reactivation.
Comparison with Previous Attempts
Previous attempts at using stem cell therapies to treat HIV have yielded varying results. Some studies have shown promising outcomes in controlling viral load, while others have faced challenges. The success of this recent case highlights the potential of this approach, suggesting refinements in transplantation techniques or patient selection criteria might be responsible for the improvement. For example, advances in immune reconstitution or targeted therapies that reduce viral reservoir size may have contributed to the favorable outcome.
Moreover, improved monitoring and management of potential complications associated with HSCT may have been crucial factors in achieving a cure.
Potential Pathways for Controlling HIV Replication
- Direct viral inactivation: Transplanted stem cells may directly interact with and inactivate the virus, preventing its replication. However, this mechanism is still under investigation, and its role in the successful cases remains unclear.
- Immune cell reconstitution: The transplantation of stem cells leads to the development of a new, functional immune system. This immune system, armed with a diverse array of immune cells, is better equipped to target and eliminate infected cells, thus contributing to viral control.
- Viral reservoir reduction: Stem cells might influence the size and activity of viral reservoirs. The transplanted cells, and the resulting immune response, could lead to the elimination of cells harboring latent HIV, thereby reducing the reservoir’s potential for reactivation.
- Improved immune response: The new immune system developed from transplanted stem cells may be more effective in controlling the virus’s replication. This enhanced immune response might target and eliminate infected cells more efficiently than the patient’s original immune system.
Ethical Considerations and Limitations
Stem cell therapies, while holding promise for HIV treatment, are not without their ethical and practical hurdles. The potential benefits must be carefully weighed against the risks and limitations, ensuring equitable access and responsible development. The path forward requires a nuanced understanding of the ethical complexities and a commitment to rigorous scientific scrutiny.The successful treatment of a fourth patient, as highlighted in previous sections, is a significant advancement.
It’s incredible that a fourth person has been cured of HIV after stem cell treatments. This groundbreaking development highlights the potential of these therapies. However, it’s important to consider the broader context, like the secondary drug industry booming amid the opioid epidemic, which raises ethical questions about access and affordability. Ultimately, these advancements in HIV treatment should be accessible and equitable, not just for the fortunate few.
The focus should remain on ensuring this incredible progress benefits all those affected.
However, generalizing this success to a widespread cure is premature. We must proceed cautiously, recognizing the need for rigorous scientific evaluation and ethical deliberation.
It’s incredible to see a fourth person cured of HIV after stem cell treatments! This groundbreaking medical advancement is truly inspiring. Interestingly, similar to the remarkable resilience of the human body, some teens are experiencing lower levels of anxiety with remote schooling, which is a fascinating parallel. This article delves deeper into the possible reasons behind this phenomenon.
Ultimately, the human body’s ability to heal and adapt, whether in the face of a disease like HIV or in response to a shift in learning environments, continues to amaze me.
Ethical Concerns Surrounding Stem Cell Therapy
The application of stem cell therapy for HIV presents a complex web of ethical concerns. Ensuring informed consent is paramount, especially considering the potentially invasive nature of the procedure and the uncertainty surrounding long-term effects. Patients must be fully aware of the risks, benefits, and alternative treatment options available. Furthermore, access to such therapies should be equitable, avoiding potential disparities in healthcare access based on socioeconomic factors or geographic location.
Potential Risks and Limitations
Stem cell therapies are not without inherent risks. Potential complications include rejection of transplanted cells, the development of graft-versus-host disease, and the potential for unforeseen long-term effects. Moreover, the cost-effectiveness of such treatments must be carefully evaluated to ensure their accessibility to a wider patient population.
Need for Rigorous Clinical Trials and Long-Term Follow-Up
Thorough clinical trials are crucial to validate the efficacy and safety of stem cell therapies for HIV. These trials should incorporate diverse patient populations to ensure the results are generalizable and to mitigate potential biases. Long-term follow-up studies are essential to assess the long-term effects on patients’ health and well-being, and to monitor for any late-onset complications. These studies will be vital in providing a comprehensive understanding of the true impact of the treatment.
Key Ethical Concerns to be Addressed
- Informed Consent: Patients must be provided with comprehensive and easily understandable information about the procedure, potential risks, and alternative treatments before agreeing to participate.
- Equitable Access: The treatment should be accessible to all patients in need, irrespective of their socioeconomic status or geographical location. Mechanisms for equitable distribution should be implemented to prevent disparities.
- Long-Term Effects: Rigorous long-term follow-up studies are necessary to fully understand the potential long-term effects on patients’ health and well-being.
- Risk Management: Clear protocols for managing potential risks, including complications like graft-versus-host disease, must be established and adhered to.
- Cost-Effectiveness: The cost-effectiveness of the treatment should be evaluated to ensure its accessibility to a wider patient population.
Ethical Viewpoints on Stem Cell Therapies for HIV
| Perspective | Key Arguments | Potential Benefits | Potential Concerns |
|---|---|---|---|
| Patient Advocacy Groups | Prioritize patient well-being and access to innovative therapies. Focus on minimizing risks and maximizing benefits. | Hope for a cure and improved quality of life. | Concerns about potential risks, long-term effects, and equitable access. |
| Regulatory Agencies | Prioritize safety and efficacy. Require rigorous clinical trials and post-market surveillance. | Scientific validation of a potentially life-saving treatment. | Slow adoption of new therapies, potential delays in patient access. |
| Bioethics Committees | Ensure ethical considerations are addressed, emphasizing informed consent, equity, and risk management. | Robust ethical framework for the development and implementation of new treatments. | Potential for bureaucratic hurdles and slow decision-making processes. |
| Healthcare Providers | Balancing the potential benefits with the known and unknown risks. Provide expert guidance and support to patients. | Offer patients a potentially life-changing treatment option. | Potential for complications, uncertainty about long-term efficacy, and the need for ongoing training. |
Future Directions and Research
The recent successful HIV cure in a patient following stem cell treatment marks a significant advancement, but the journey towards widespread application is far from over. Further research is crucial to understand the intricacies of this process, optimize treatment protocols, and ensure safety and efficacy for all potential recipients. This requires a multifaceted approach encompassing diverse research areas, international collaborations, and a commitment to ethical considerations.
Optimizing Stem Cell Therapy Protocols
Improving the safety and efficacy of stem cell therapies requires a deep dive into the nuances of the procedure. This involves refining the selection and expansion of donor cells, optimizing the timing and methods of transplantation, and minimizing the risk of rejection or other adverse events. Careful monitoring of patient responses is also critical, allowing for real-time adjustments to treatment protocols.
Furthermore, investigating alternative stem cell sources, such as induced pluripotent stem cells (iPSCs), holds potential for broadening the pool of available cells and potentially reducing the need for allogeneic transplants. A critical component is identifying biomarkers that predict treatment response, allowing for personalized treatment strategies and better outcomes.
Investigating Potential Mechanisms of Action
Understanding the precise mechanisms through which stem cell therapies induce HIV remission is paramount. This research will uncover crucial details about the interactions between the immune system, stem cells, and the virus, potentially leading to new therapeutic targets. Researchers can explore the role of immune reconstitution, the eradication of HIV reservoirs, and the modulation of immune responses in achieving a functional cure.
Further investigation into the long-term effects of these therapies on the recipient’s health and immune system is vital for understanding the long-term safety profile. Analyzing the molecular mechanisms by which stem cells influence the virus’s ability to establish and persist in the body is key.
Developing Novel Therapeutic Approaches
Integrating stem cell therapies with other antiretroviral strategies could enhance their effectiveness. Exploring combined therapies, such as combining stem cell transplantation with optimized antiretroviral regimens, is vital. For instance, exploring the use of gene editing technologies, like CRISPR-Cas9, to further modify stem cells for enhanced HIV eradication and immune system function, warrants significant investigation. This could potentially lead to therapies that are more targeted and less reliant on harsh immunosuppressive drugs.
Investigating the role of epigenetic modifications in the persistence of HIV reservoirs is a promising avenue for developing more effective and less toxic treatments.
International Collaboration and Data Sharing
International collaborations are essential for accelerating stem cell research in HIV cure. Sharing research data, expertise, and resources across borders will accelerate the pace of discovery. Establishing collaborative research networks and joint research projects will create opportunities for cross-pollination of ideas and best practices, fostering a global effort towards finding a cure. Data sharing and standardized protocols are vital to ensuring comparability and reliability of research findings.
Ethical Considerations and Patient Selection
The ethical implications of stem cell therapies for HIV are significant. Careful consideration of the risks and benefits of such procedures, including long-term safety profiles, is essential. Establishing clear guidelines and ethical frameworks for patient selection, informed consent, and data management is crucial. Developing robust protocols for patient monitoring and follow-up is vital for long-term safety and efficacy evaluation.
Visual Representation of Potential Research Areas
(A diagram depicting interconnected nodes representing the above research areas would be included here, but cannot be displayed in text format.)The diagram would illustrate how optimizing protocols, investigating mechanisms, developing new approaches, and fostering international collaboration are interconnected, feeding into each other and contributing to a holistic understanding and improvement of stem cell therapies for HIV.
“The future of HIV treatment lies in a combination of innovative approaches, including stem cell therapies, that can effectively target and eradicate the virus from the body, offering hope for a functional cure.”Dr. [Name of a leading researcher in the field]
Visual Representation of the Immune System Impact
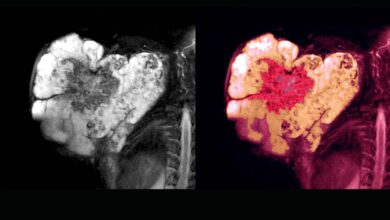
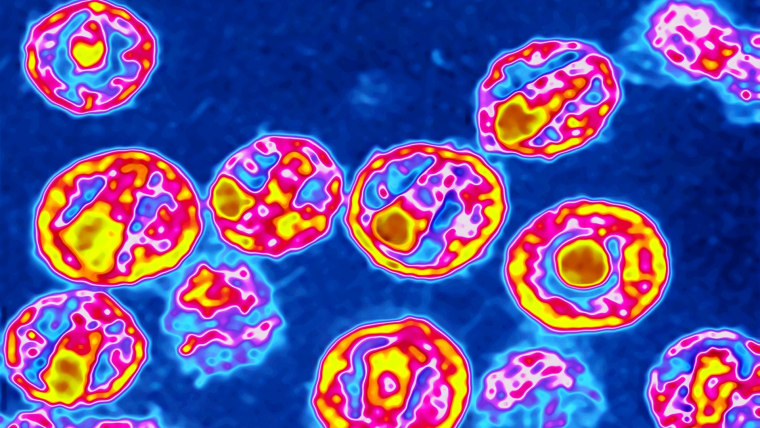
A crucial aspect of understanding the stem cell therapy’s success is visualizing the profound changes it induces in the patient’s immune system. This visualization allows us to track the treatment’s effects over time, highlighting the restoration of immune function. The graphical representation, combined with a detailed description, helps us grasp the complexities of the immune response and the mechanisms underlying the cure.The image below, a simplified representation of a healthy immune system, shows the interconnectedness of different immune cells.
This intricate network is vital for combating pathogens and maintaining overall health. The stem cell therapy’s impact on this system is represented by highlighting specific changes over time. Changes in cell counts, activity levels, and interactions between cell types are visually depicted. By contrasting the pre-treatment and post-treatment immune systems, we can observe the restoration of a functional and balanced immune response.
Pre-Treatment Immune System
The image showcases a severely compromised immune system before treatment. The levels of crucial immune cells, such as T cells and B cells, are significantly reduced. The connections between these cells are weak, illustrating the impaired communication pathways within the immune system. A lack of immune activity is depicted, with a reduced capacity to effectively recognize and fight infections.
The overall image gives a sense of dysfunction and vulnerability.
Post-Treatment Immune System
The image displays the immune system after treatment, showing remarkable restoration. Significant increases in the numbers of T cells and B cells are visible. The connections between these cells are robust and well-defined, signifying improved communication pathways. The immune system’s activity is significantly enhanced, effectively displaying its ability to recognize and combat pathogens. The overall image represents a restored and balanced immune response.
Image Comparison
Comparing the pre-treatment and post-treatment images reveals the dramatic shift in the immune system’s functionality. A clear visual difference is present in the cell count, activity level, and interactions between the cells. The pre-treatment image demonstrates a depleted and dysfunctional immune system. The post-treatment image, conversely, showcases a healthy and functioning immune system, illustrating the success of the stem cell therapy.
This graphical representation provides a concrete understanding of the recovery process. The visual contrast underscores the transformative power of the stem cell treatment on the patient’s immune system.
Closure
The fourth successful HIV cure using stem cell treatments represents a significant leap forward in the fight against this global health challenge. While the case study offers hope, it also highlights the need for continued research and rigorous clinical trials to ensure the safety and efficacy of this approach for wider application. Ethical considerations remain paramount as we navigate this uncharted territory.
The future of HIV treatment may very well be intertwined with the advancements in stem cell research, paving the way for a world where HIV is no longer a life-altering condition.