How does immunotherapy work melanoma? This exploration delves into the fascinating world of immunotherapy, a revolutionary approach to battling melanoma. We’ll uncover the intricacies of how this treatment method harnesses the power of the immune system to target and destroy cancerous melanoma cells. From understanding the different types of immunotherapy to examining clinical trials and patient outcomes, we’ll provide a comprehensive overview of this promising field.
Melanoma, a particularly aggressive form of skin cancer, poses significant challenges. Traditional cancer treatments often fall short, but immunotherapy offers a new hope by stimulating the body’s natural defenses to fight the disease. We’ll analyze the mechanisms behind these treatments, highlighting the advantages and disadvantages of each approach. Tables and flowcharts will illustrate the processes involved, providing a clear picture of how immunotherapy works on a cellular level.
Introduction to Immunotherapy for Melanoma
Melanoma, the most dangerous form of skin cancer, arises from melanocytes, specialized cells producing melanin, the pigment that gives skin its color. Its progression can be aggressive, with the potential to spread rapidly to other parts of the body if not detected and treated early. Early detection and prompt intervention are crucial in improving patient outcomes.Immunotherapy, a revolutionary approach in cancer treatment, harnesses the body’s own immune system to fight cancer cells.
It differs significantly from conventional treatments like surgery, chemotherapy, and radiation, which directly target and destroy cancer cells, often with significant side effects. Instead, immunotherapy empowers the immune system to recognize and destroy cancer cells, leading to a more targeted and often less toxic approach.
Conventional Cancer Treatments vs. Immunotherapy
Conventional cancer treatments often involve broad-spectrum attacks on rapidly dividing cells, leading to side effects impacting healthy cells. Immunotherapy, on the other hand, is designed to stimulate the immune system’s ability to distinguish between healthy and cancerous cells. This specificity results in a more targeted approach, often with fewer side effects. The choice of treatment depends on various factors, including the stage of the cancer, the patient’s overall health, and the specific characteristics of the tumor.
| Treatment Type | Mechanism of Action | Advantages | Disadvantages |
|---|---|---|---|
| Surgery | Removal of the tumor and surrounding tissue. | Can be curative for localized melanoma. | May not be suitable for advanced stages. Potential for scarring. |
| Chemotherapy | Use of drugs to kill rapidly dividing cells, including cancer cells. | Effective in reducing tumor size and spread. | Significant side effects, including nausea, hair loss, and fatigue. |
| Radiation Therapy | Use of high-energy radiation to damage cancer cells. | Effective for localized tumors. | Potential for long-term side effects, like skin damage or fibrosis. |
| Immunotherapy | Stimulates the immune system to recognize and destroy cancer cells. | Targeted approach, potentially fewer side effects compared to chemotherapy. Can be effective in advanced stages. | May not be effective for all patients. Potential for immune-related side effects (immune-related adverse events, or irAE). |
Key Differences Between Conventional and Immunotherapy
The table above highlights the key distinctions between conventional cancer treatments and immunotherapy. Immunotherapy’s focus on leveraging the body’s natural defenses provides a unique approach to fighting cancer. While conventional methods directly attack cancer cells, immunotherapy works by empowering the immune system to identify and eliminate them. This targeted approach often results in fewer side effects and improved quality of life for patients.
Immunotherapy Mechanisms in Melanoma
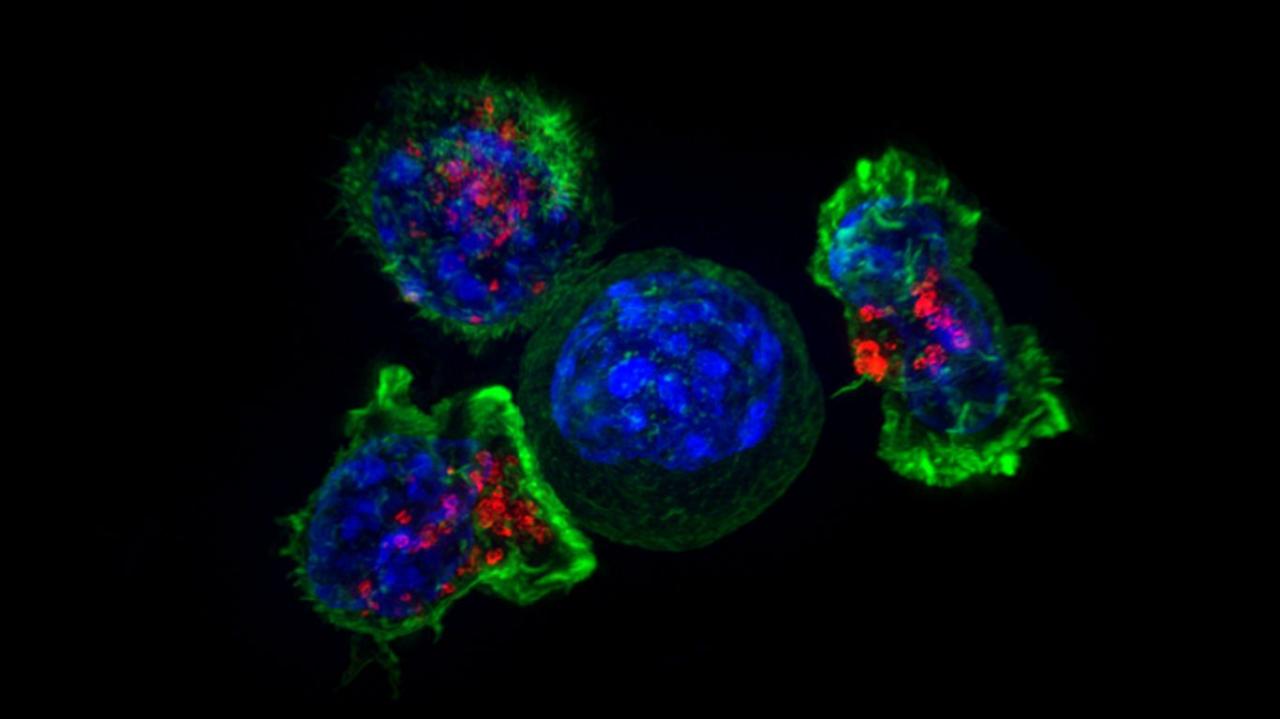
Immunotherapy works by triggering the body’s immune system to recognize and attack melanoma cells. This can occur through various mechanisms, such as checkpoint inhibitors, adoptive cell therapies, and cancer vaccines. Checkpoint inhibitors block proteins that normally prevent the immune system from attacking cancer cells. Adoptive cell therapies involve extracting immune cells from the patient, modifying them to target melanoma cells, and then infusing them back into the patient.
Cancer vaccines train the immune system to recognize and attack melanoma cells. Each mechanism has its own unique strengths and weaknesses.
Types of Immunotherapy for Melanoma
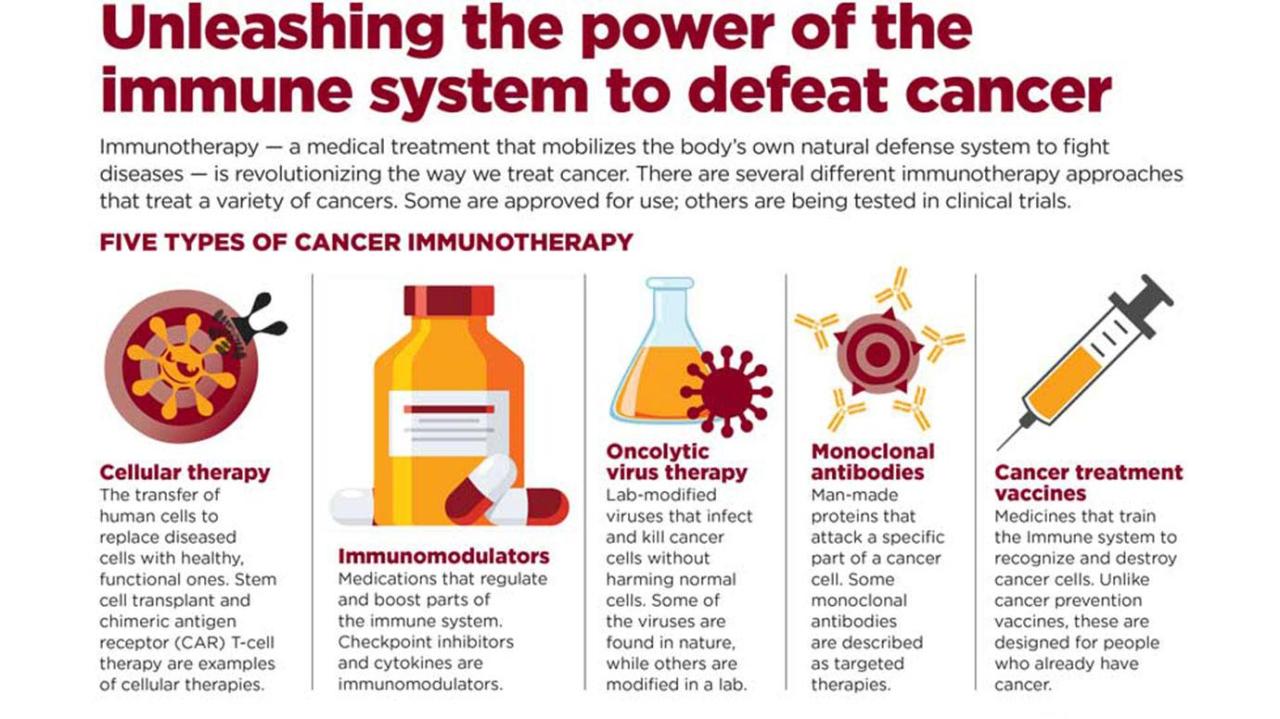
Immunotherapy for melanoma has revolutionized treatment strategies, offering a more targeted and often more effective approach compared to traditional methods. This approach harnesses the body’s own immune system to fight the cancer cells, leading to significant improvements in patient outcomes. Understanding the different types of immunotherapy and their mechanisms is crucial for comprehending the advancements in melanoma treatment.
Checkpoint Inhibitors
Checkpoint inhibitors are a prominent class of immunotherapy that work by releasing the brakes on the immune system. These drugs block proteins, known as checkpoints, that normally suppress immune responses. By removing these roadblocks, the immune system can recognize and attack melanoma cells more effectively. This targeted approach minimizes side effects compared to nonspecific chemotherapy.
- Mechanism of Action: Checkpoint inhibitors, such as ipilimumab and nivolumab, target specific proteins like PD-1 and CTLA-4, which normally prevent immune cells from attacking cancer cells. By blocking these checkpoints, the immune system is freed to recognize and destroy melanoma cells.
- Effectiveness: Checkpoint inhibitors have shown remarkable success in treating advanced melanoma, leading to improved survival rates and quality of life for many patients. They are often used in combination with other therapies to enhance their effectiveness.
- Limitations: While highly effective, checkpoint inhibitors can cause immune-related side effects, such as colitis, skin rashes, and fatigue. These side effects, although generally manageable, can affect treatment duration and require careful monitoring.
Adoptive Cell Therapies
Adoptive cell therapies represent a more advanced approach, directly manipulating the patient’s own immune cells to fight the cancer. These therapies typically involve extracting immune cells, modifying them in the laboratory to enhance their anti-tumor activity, and then reintroducing them into the patient.
- Mechanism of Action: Adoptive cell therapies, like CAR T-cell therapy, involve extracting T cells from the patient’s blood. These T cells are then genetically engineered to express a chimeric antigen receptor (CAR). The CAR allows the T cells to specifically recognize and target melanoma cells. The modified T cells are then multiplied in the lab and reinfused into the patient.
Immunotherapy for melanoma works by boosting your immune system to fight the cancer cells. This often involves giving your body tools to recognize and attack the melanoma, a complex process. Getting in shape for surgery getting in shape for surgery is crucial for a successful outcome, and the same kind of preparation and focus on overall health can benefit immunotherapy treatments.
Stronger physical health can make your body better equipped to handle the immunotherapy’s work in combating the melanoma.
- Effectiveness: These therapies have shown remarkable success in treating certain types of melanoma, particularly in cases where other treatments have failed. The high specificity and potent anti-tumor activity of CAR T cells hold promise for personalized and highly effective melanoma treatment.
- Limitations: Adoptive cell therapies are still relatively new and require sophisticated laboratory procedures. Potential side effects, including cytokine release syndrome (CRS) and neurotoxicity, can be severe and require intensive monitoring and management. The cost of these therapies is also a significant factor.
Other Immunotherapies
Other immunotherapy approaches are also being explored for melanoma treatment, including oncolytic viruses and vaccines.
- Mechanism of Action: Oncolytic viruses are engineered viruses that selectively target and kill cancer cells. These viruses replicate within tumor cells, causing their destruction and releasing signals that stimulate an anti-tumor immune response. Cancer vaccines aim to stimulate the immune system to recognize and attack melanoma-specific antigens.
- Effectiveness: These therapies are still under investigation, with some promising early results. Their long-term effectiveness and safety profiles are not yet fully understood. Their use is often in clinical trials to evaluate efficacy and safety.
- Limitations: The development of these approaches is still in progress, with ongoing clinical trials to evaluate their effectiveness and safety in various patient populations. The specific mechanisms and long-term outcomes require further research.
Comparison of Immunotherapy Types
| Immunotherapy Type | Target Molecules | Clinical Trials | Patient Outcomes |
|---|---|---|---|
| Checkpoint Inhibitors | PD-1, CTLA-4 | Extensive clinical trials demonstrating efficacy in various melanoma stages | Improved survival rates, reduced tumor burden, and improved quality of life in many patients |
| Adoptive Cell Therapies | CAR T-cells targeting melanoma-specific antigens | Ongoing trials focusing on optimizing safety and effectiveness | Potential for durable responses and remission in selected patients, but significant side effect profiles |
| Other Immunotherapies | Oncolytic viruses, cancer vaccines | Early-stage trials evaluating safety and efficacy | Preliminary results are promising but require further investigation |
Mechanisms of Action in Melanoma Immunotherapy
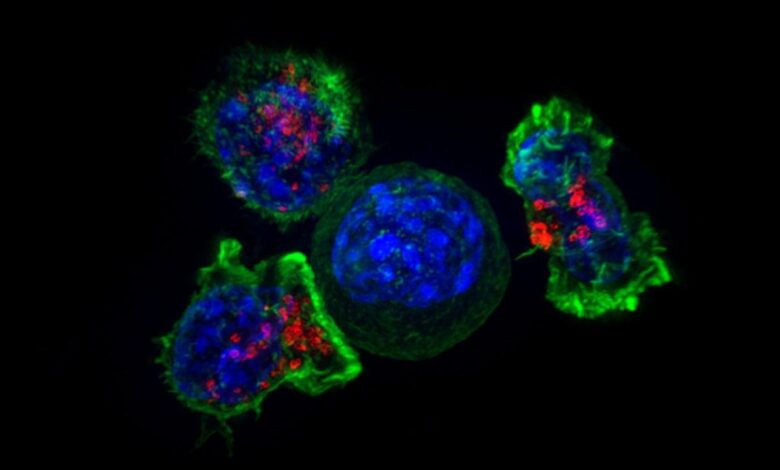
Immunotherapy for melanoma harnesses the power of the body’s own immune system to fight the cancer. Understanding how these therapies work is crucial for appreciating their potential and limitations. These treatments essentially re-educate or re-activate the immune system to recognize and destroy melanoma cells, often with impressive results.The immune system, in its normal state, has the remarkable ability to identify and eliminate abnormal cells, including those that are cancerous.
However, melanoma cells often develop ways to evade detection and destruction by the immune system. Immunotherapies act by various mechanisms, either by directly boosting the immune response against the tumor, or by removing the obstacles that melanoma cells use to hide from the immune system. This direct or indirect approach allows the immune system to target and eliminate the cancer cells more effectively.
Immune Checkpoint Inhibitors
These therapies work by blocking proteins on immune cells (like T cells) and tumor cells that normally act as “brakes” on the immune response. By removing these brakes, the immune system is unleashed to attack the melanoma cells more aggressively. Examples include blocking PD-1 and CTLA-4, which are immune checkpoints that melanoma cells exploit to suppress the immune response.
Immune Cell-Based Therapies, How does immunotherapy work melanoma
These therapies use various immune cells to directly target and destroy melanoma cells. One example is adoptive cell transfer, where immune cells (like T cells) are extracted from a patient, modified in the lab to better target melanoma cells, and then reintroduced into the patient. These engineered T cells are armed with the knowledge of how to identify and eliminate the specific cancer cells.
Immunotherapy for melanoma essentially trains your immune system to recognize and attack cancer cells. It’s a fascinating area of research, but unfortunately, environmental factors like secondhand smoke in apartments and condos can significantly impact health, including the effectiveness of treatments like immunotherapy. Learning about the dangers of secondhand smoke in apartments and condominiums is crucial for anyone hoping to improve their chances of successful immunotherapy treatments.
So, while immunotherapy is powerful, a healthy lifestyle is essential for maximizing its potential.
Another example is chimeric antigen receptor (CAR) T-cell therapy. CAR T cells are engineered to recognize and attack cancer cells with a specific protein on their surface. These therapies are highly personalized and can have significant impacts on the patient’s outcome.
Immunotherapy for melanoma works by boosting the body’s own immune system to fight the cancer cells. A healthy immune system is crucial for overall well-being, and it’s interesting to consider how diet might play a role. For example, studies suggest that incorporating fermented foods into your diet might help reduce inflammation, which could potentially support a robust immune response.
Check out this article to learn more about can eating fermented foods help curb inflammation. Ultimately, a combination of treatment and a healthy lifestyle may be key to successful melanoma immunotherapy.
Other Immunotherapies
Other therapies include oncolytic viruses, which infect and destroy cancer cells, often triggering an immune response in the process. Cancer vaccines are designed to stimulate the immune system to recognize and attack melanoma cells, similar to how traditional vaccines work to prevent infectious diseases.
Flowchart of Immune Response Triggered by Immunotherapy

*Note: A visual representation of the flowchart is not available in this text format. A visual flowchart would show the following steps, connecting the different processes in a clear manner.*
1. Immunotherapy Agent Activation
The immunotherapy (e.g., checkpoint inhibitor) is administered.
2. Immune Checkpoint Blockade (if applicable)
The immunotherapy targets and blocks immune checkpoints (e.g., PD-1/PD-L1).
3. Immune Cell Activation
Immune cells (e.g., T cells) are activated and released from regulatory mechanisms.
4. Tumor Cell Recognition
Activated immune cells recognize and bind to melanoma cells.
5. Tumor Cell Destruction
Activated immune cells release cytotoxic molecules and directly destroy the melanoma cells.
6. Anti-Tumor Immune Response
A cascade of immune responses, including the recruitment of other immune cells, is triggered to effectively eliminate the tumor.
Clinical Trials and Research: How Does Immunotherapy Work Melanoma
The journey of melanoma immunotherapy has been a fascinating one, marked by significant breakthroughs and continuous refinement. From initial skepticism to widespread adoption, the field has evolved rapidly, driven by rigorous clinical trials and a deep understanding of the immune system’s intricate role in fighting cancer. This section delves into the historical context, key milestones, and the ongoing research shaping the future of melanoma treatment.
Historical Background of Immunotherapy for Melanoma
Immunotherapy for melanoma wasn’t always the dominant approach. Early treatments focused primarily on surgery, radiation, and chemotherapy. However, the understanding of the immune system’s potential to recognize and destroy cancer cells laid the groundwork for the development of immunotherapy. Pioneering research highlighted the possibility of harnessing the body’s own defenses to combat the disease, leading to the development of various strategies.
Early trials, though limited in scope and understanding, served as essential stepping stones toward more effective and targeted approaches.
Significant Milestones in Melanoma Immunotherapy
The development of melanoma immunotherapy has been marked by several pivotal moments. These include the discovery of tumor-infiltrating lymphocytes (TILs) and their potential as a treatment modality, the identification of specific immune checkpoints that regulate immune responses, and the development of immune checkpoint inhibitors. These breakthroughs, coupled with ongoing research, have significantly improved patient outcomes and transformed the landscape of melanoma treatment.
Clinical Trial Examples
| Trial Name | Target Population | Key Findings | Future Implications |
|---|---|---|---|
| CheckMate 066 | Patients with advanced melanoma who had not responded to previous treatments | Pembrolizumab, an immune checkpoint inhibitor, demonstrated significant improvements in overall survival and response rates compared to chemotherapy. | This trial solidified the role of immune checkpoint inhibitors as a standard of care for advanced melanoma and paved the way for similar trials in other cancers. |
| KEYNOTE-001 | Patients with advanced melanoma | Nivolumab, another immune checkpoint inhibitor, showed promising results in terms of efficacy and safety. | These findings highlighted the broad applicability of immune checkpoint inhibitors and contributed to their broader clinical use. |
| MEDI0680 | Patients with unresectable melanoma | This trial explored the combination of immunotherapy and other treatments, demonstrating potential benefits. | Combinatorial approaches, such as the ones studied here, hold promise for improving treatment outcomes further and addressing treatment-resistant cases. |
Ongoing Research and Future Directions
Ongoing research focuses on refining existing therapies and exploring new avenues. This includes developing personalized immunotherapy strategies tailored to individual patient characteristics and tumor profiles, investigating the use of adoptive cell therapies with increased efficacy, and exploring innovative combinations of immunotherapy with other cancer treatments. Advancements in understanding the tumor microenvironment and the interactions between immune cells and cancer cells will be crucial in driving future developments.
For example, studies are investigating how to enhance the activity of immune cells within the tumor, making them more effective at targeting and destroying cancer cells. Researchers are also looking at ways to predict which patients are most likely to benefit from specific immunotherapies, thereby maximizing the efficacy of treatment.
Patient Response and Outcomes
Understanding how patients respond to immunotherapy for melanoma is crucial for tailoring treatment strategies and improving outcomes. This section delves into the factors impacting response, the diverse types of responses seen, and success rates across different melanoma subtypes. Predicting individual patient responses remains a challenge, but ongoing research is steadily refining our understanding of these complex interactions.
Factors Influencing Patient Response
Several factors influence a patient’s response to immunotherapy. These include the specific type of melanoma, the patient’s overall health, genetic factors, the presence of other medical conditions, and the specific immunotherapy regimen used. The presence of pre-existing immune deficiencies or conditions that compromise the immune system can significantly impact response rates. Tumor characteristics, such as mutational load and the presence of specific immune checkpoint targets, are also important factors.
The tumor microenvironment, which comprises the cells and molecules surrounding the tumor, plays a role in influencing the efficacy of immunotherapy.
Types of Patient Responses
Patient responses to immunotherapy can manifest in various ways. Complete response, where the cancer is eradicated, is the ideal outcome. Partial response involves a reduction in tumor size, signifying a positive impact of treatment. Stable disease indicates that the tumor growth is halted, providing a period of remission. Progressive disease signifies tumor growth despite treatment.
Understanding these response categories is essential for assessing the efficacy of therapy and guiding treatment decisions.
Success Rates Across Melanoma Subtypes
Success rates of immunotherapy vary among different types of melanoma. Cutaneous melanoma, the most common type, generally shows promising response rates to immunotherapies, though the specific response rates may vary based on the subtype. The effectiveness of immunotherapy may differ depending on the specific genetic profile of the melanoma.
Comparative Analysis of Patient Outcomes
The following table provides a comparative analysis of patient characteristics, treatment regimens, response types, and overall survival. This information is presented to illustrate the complexity of patient outcomes and the need for individualized treatment approaches. Note that this is a simplified example and actual data will vary greatly based on numerous factors.
| Patient Characteristics | Treatment Regimen | Response Type | Overall Survival (months) |
|---|---|---|---|
| Stage III melanoma, high mutational load, good general health | Checkpoint inhibitor (e.g., ipilimumab) | Complete Response | >60 |
| Stage IV melanoma, BRAF mutation, moderate health | Combination therapy (checkpoint inhibitor + anti-angiogenic) | Partial Response | 36 |
| Stage II melanoma, low mutational load, history of autoimmune disease | Checkpoint inhibitor (e.g., nivolumab) | Stable Disease | 24 |
| Stage IV melanoma, unknown genetic profile, poor general health | Combination therapy (checkpoint inhibitor + targeted therapy) | Progressive Disease | 12 |
Side Effects and Management
Immunotherapy for melanoma, while powerful, can trigger various side effects. Understanding these potential complications and the strategies to manage them is crucial for patient well-being and treatment success. Careful monitoring and proactive management are vital for maximizing the benefits of immunotherapy while minimizing its adverse effects.
Potential Side Effects
Immunotherapy, by stimulating the immune system to attack cancer cells, can also inadvertently target healthy tissues. This can lead to a range of side effects, some mild and manageable, others more severe. The specific side effects and their severity can vary greatly depending on the type of immunotherapy used, the patient’s individual characteristics, and the dosage. These effects are often dose-dependent and can range from mild discomfort to life-threatening complications.
Mechanisms of Side Effects
The mechanisms behind immunotherapy side effects stem from the immune system’s heightened activity. When the immune system is activated to fight cancer cells, it can mistakenly target healthy cells, leading to inflammation and damage in various parts of the body. This is a complex process involving multiple immune cells and pathways, which can lead to a cascade of effects in different organs and tissues.
Strategies for Managing Side Effects
Effective management of immunotherapy side effects relies on a multi-faceted approach. Early recognition and prompt intervention are crucial. Close monitoring by healthcare professionals is essential to detect and address problems as they arise. Supportive care measures, including pain management, nutritional support, and symptom relief, are integral to patient comfort and quality of life. Medical interventions, like medication adjustments or specific therapies, may be necessary to control severe side effects.
Table of Side Effects, Mechanisms, Symptoms, and Management Strategies
| Side Effect | Mechanism | Symptoms | Management Strategies |
|---|---|---|---|
| Fatigue | Immune activation and inflammation throughout the body | Persistent tiredness, lack of energy, difficulty concentrating | Rest periods, pacing activities, nutritional support (e.g., iron supplementation), potential medication adjustments, and counseling on energy conservation techniques. |
| Inflammation | Immune response targeting healthy tissues | Swelling, redness, pain, fever, discomfort at the injection site. | Cold compresses, anti-inflammatory medications (NSAIDs), pain relievers, and close monitoring of inflammation markers. In severe cases, corticosteroids may be necessary. |
| Skin Reactions | Immune response targeting skin cells | Rashes, itching, dryness, inflammation, blisters, skin sores at the injection site | Moisturizing creams, topical steroids, antihistamines, and in severe cases, systemic medications. |
| Immune-related colitis | Immune system attacking the colon | Abdominal pain, diarrhea, bloody stools, nausea, and vomiting. | Dietary modifications, anti-inflammatory medications, and in severe cases, hospitalization and intravenous fluids. |
Future of Immunotherapy in Melanoma Treatment
The journey of immunotherapy in melanoma treatment has been remarkable, moving from a novel concept to a cornerstone of care. As research progresses, the future holds even more promise, focusing on personalized approaches, synergistic combinations, and innovative strategies. This evolution is driven by a deep understanding of the immune system’s intricate role in fighting cancer, specifically melanoma.The future of melanoma immunotherapy hinges on refining existing approaches and developing entirely new ones.
Personalized medicine is set to play a pivotal role, tailoring treatments to the unique genetic and immunological characteristics of each patient. This targeted approach has the potential to enhance treatment efficacy and minimize side effects, marking a paradigm shift in cancer care. Furthermore, the integration of immunotherapy with other modalities, such as surgery, radiation, and chemotherapy, could unlock even greater therapeutic potential.
These combined approaches will undoubtedly be a key element in achieving durable responses and improving patient outcomes.
Personalized Immunotherapy Approaches
Personalized immunotherapy for melanoma aims to leverage individual patient characteristics to maximize treatment effectiveness. This includes analyzing a patient’s tumor’s specific genetic mutations, immune cell profiles, and other relevant factors to develop a tailored treatment strategy. For instance, identifying specific neoantigens presented by the tumor cells allows for the development of vaccines or immune checkpoint inhibitors that are more likely to be effective in targeting that particular cancer.
By focusing on the individual tumor’s genetic fingerprint, personalized immunotherapy could drastically improve the chances of a successful outcome.
Integration of Immunotherapy with Other Treatment Modalities
Combining immunotherapy with other treatment modalities is a promising avenue for enhancing outcomes. For example, combining immune checkpoint inhibitors with targeted therapies that inhibit specific growth pathways in melanoma cells can create a synergistic effect, leading to a more potent anti-tumor response. Surgery, radiation therapy, and chemotherapy can also play a supportive role, clearing tumor burden and preparing the tumor microenvironment for a stronger immune response.
These combined approaches are expected to lead to improved outcomes, especially in cases where the tumor burden is substantial or the tumor exhibits resistance to single-agent immunotherapy.
Future Developments in Melanoma Immunotherapy
Novel therapies and combinations are constantly emerging in the field of melanoma immunotherapy. The development of novel immune checkpoint inhibitors targeting different pathways, or even new immune cells and molecules for engagement, could broaden the therapeutic options available. Furthermore, the advancement of immunotherapy delivery systems, such as targeted drug delivery or nanotechnology, could improve treatment efficacy and minimize side effects.
Research into immune-activating agents, like cytokines or engineered T cells, offers another promising area for future development. These approaches are likely to improve response rates, reduce the duration of treatment, and ultimately improve patient outcomes.
Comparison of Immunotherapy Types Based on Future Potential
| Immunotherapy Type | Future Potential | Examples |
|---|---|---|
| Immune Checkpoint Inhibitors | High potential for further development, especially in personalized medicine contexts, where specific targets and combinations can be tailored to individual patients. | PD-1/PD-L1 inhibitors, CTLA-4 inhibitors |
| Adoptive Cell Therapy (CAR T-cells) | Continued development of CAR designs and engineering strategies, potentially leading to broader application and improved safety profiles. Focus on engineering cells that can persist longer in the body. | Chimeric Antigen Receptor (CAR) T-cells |
| Cancer Vaccines | Personalized approaches using neoantigen-based vaccines hold significant potential. Developing vaccines to target specific genetic mutations in the patient’s tumor. | Neoantigen-based vaccines |
| Cytokine Therapy | Further research on cytokine cocktails and targeted delivery systems could improve efficacy and safety. | Interferon-alpha, IL-2 |
Illustrative Examples
Immunotherapy for melanoma, while showing remarkable success, presents a complex interplay of individual responses, treatment strategies, and potential side effects. Understanding these nuances through real-world examples and hypothetical scenarios provides a valuable framework for comprehending the treatment’s practical application and limitations. This section delves into specific case studies, potential challenges, and emerging research breakthroughs to paint a clearer picture of the future of melanoma immunotherapy.
Case Study of Successful Treatment
A 55-year-old male patient, diagnosed with stage III melanoma, initially received conventional chemotherapy, but experienced significant side effects and showed no response. Subsequently, he underwent treatment with a checkpoint inhibitor, specifically pembrolizumab. After several cycles, the patient experienced a complete remission of the tumor, with no evidence of disease progression for over two years. This outcome highlights the potential for immunotherapy to effectively treat melanoma even in cases where conventional therapies have failed.
This case also underscores the importance of personalized treatment approaches and the potential for long-term remission in responsive patients.
Hypothetical Scenario: Challenges and Benefits
Consider a 30-year-old female patient with a BRAF-mutated melanoma, diagnosed at stage II. This patient has a strong family history of autoimmune diseases, increasing the risk of immunotherapy-related adverse events. The benefits of immunotherapy, including the potential for durable responses, are significant. However, the patient’s pre-existing predisposition to autoimmune issues necessitates careful monitoring and management of potential side effects.
The physician would need to meticulously weigh the potential risks and benefits of immunotherapy, carefully considering the patient’s overall health profile, tumor characteristics, and the specific immunotherapy option available.
Recent Research Breakthrough
A recent study published in theJournal of Clinical Oncology* investigated the use of a novel combination therapy involving a checkpoint inhibitor and a programmed cell death-1 (PD-1) ligand. This approach demonstrated significant tumor regression in preclinical models of melanoma, especially in patients with specific genetic markers. Preliminary results suggest that the combination therapy enhances the body’s anti-tumor immune response, potentially leading to improved outcomes for patients with melanoma.
The study highlighted the potential for combining different immunotherapy strategies to amplify their effectiveness and overcome resistance mechanisms.
Comparison of Immunotherapy Approaches
| Characteristic | Checkpoint Inhibitors (e.g., Pembrolizumab) | Adoptive Cell Therapy (e.g., CAR T-cell therapy) |
|---|---|---|
| Mechanism of Action | Blockade of immune checkpoints, allowing the immune system to recognize and attack tumor cells. | Isolation and modification of a patient’s immune cells (T cells) to specifically target and destroy tumor cells. |
| Administration | Infusion of drugs intravenously. | Collection, modification, expansion, and reinfusion of immune cells. |
| Potential Side Effects | Immune-related adverse events (e.g., colitis, skin rash). | Cytokine release syndrome, neurotoxicity, and graft-versus-host disease. |
| Cost | Generally lower compared to adoptive cell therapies. | Significantly higher due to the complex manufacturing process. |
| Patient Selection | Wider range of patients, including those with specific genetic markers. | More restricted to patients with specific tumor characteristics. |
This table summarizes key distinctions between two prevalent immunotherapy approaches, emphasizing the similarities and differences in their mechanisms, administration, potential side effects, cost, and patient selection criteria. Each approach offers unique advantages and disadvantages, highlighting the importance of individualized treatment strategies.
Summary
In conclusion, immunotherapy offers a promising avenue for treating melanoma, though it’s not a one-size-fits-all solution. The effectiveness of these treatments varies depending on the patient and the specific type of melanoma. Understanding the mechanisms, clinical trials, and potential side effects is crucial for informed decision-making. While challenges remain, ongoing research and the development of personalized approaches suggest a bright future for immunotherapy in melanoma treatment.