How eating only in the daytime can help people with type 2 diabetes is a fascinating area of exploration. This approach, sometimes called time-restricted eating, suggests that controlling your eating window to daylight hours could significantly impact blood sugar management. The potential benefits extend beyond blood sugar, touching on general health improvements. This article delves into the science behind this method, considering its effects on blood glucose levels, potential mechanisms, and practical implementation strategies.
We’ll explore how it could influence circadian rhythms, address specific considerations for various populations, and examine potential caveats.
The idea of restricting eating to a specific timeframe during the day holds promise for managing type 2 diabetes. By focusing on daytime meals, we can explore the potential impact on insulin sensitivity and secretion. This could also help regulate blood glucose levels, potentially leading to better overall health outcomes. Let’s dive into the research and see how this approach can help.
Introduction to Daytime Eating and Type 2 Diabetes
Restricting eating to daylight hours, often referred to as the “time-restricted eating” (TRE) method, involves consuming all meals and snacks within a specific timeframe, typically during daylight hours. This approach has gained attention for its potential health benefits, particularly for individuals with type 2 diabetes. While not a cure-all, it may contribute to improved metabolic function and overall well-being.
This practice is distinct from intermittent fasting, which often involves longer periods of fasting.The potential advantages of TRE extend beyond blood sugar management. Improved sleep quality, reduced cravings, and potentially better weight management are frequently cited. The impact on blood sugar regulation for individuals with type 2 diabetes is thought to arise from the body’s natural circadian rhythm.
By aligning eating patterns with the body’s natural cycle, it may enhance insulin sensitivity and help regulate blood glucose levels throughout the day.
Potential Benefits for Type 2 Diabetes
Restricting eating to daylight hours might positively influence blood sugar levels in several ways. By aligning food intake with the body’s natural metabolic processes, individuals might experience improved insulin sensitivity. This enhanced sensitivity allows the body to utilize insulin more effectively, potentially leading to better control of blood glucose levels. Further, the reduced time span for food intake might contribute to weight management, as fewer calories are consumed overall.
A lower body weight, in turn, often improves metabolic health markers, including blood sugar regulation.
Advantages and Disadvantages of Daytime Eating for Type 2 Diabetes
Implementing TRE can have a range of impacts. Understanding both the potential benefits and drawbacks is crucial for making informed decisions.
| Potential Advantages | Potential Disadvantages | Explanation | Examples |
|---|---|---|---|
| Improved Insulin Sensitivity | Potential for Increased Hunger | TRE may lead to enhanced insulin action, enabling the body to process glucose more efficiently. | Some individuals might experience heightened hunger pangs outside the designated eating window, potentially leading to overeating during permitted hours. |
| Weight Management Potential | Potential for Digestive Issues | Reduced calorie intake, due to the limited eating window, can contribute to weight loss or maintenance. | If not managed carefully, the drastic change in eating patterns can lead to digestive discomfort, such as bloating or indigestion. |
| Improved Circadian Rhythm | Social Challenges | Synchronizing eating patterns with the body’s natural sleep-wake cycle might enhance metabolic function. | Scheduling meals around social events or work commitments can be challenging. |
| Reduced Risk of Late-Night Cravings | Potential for Nutrient Deficiencies | Restricting late-night snacking can help reduce cravings and unhealthy food choices. | If the eating window is too short or the diet isn’t well-balanced, it could potentially lead to nutrient deficiencies. |
Impact on Blood Glucose Levels: How Eating Only In The Daytime Can Help People With Type 2 Diabetes
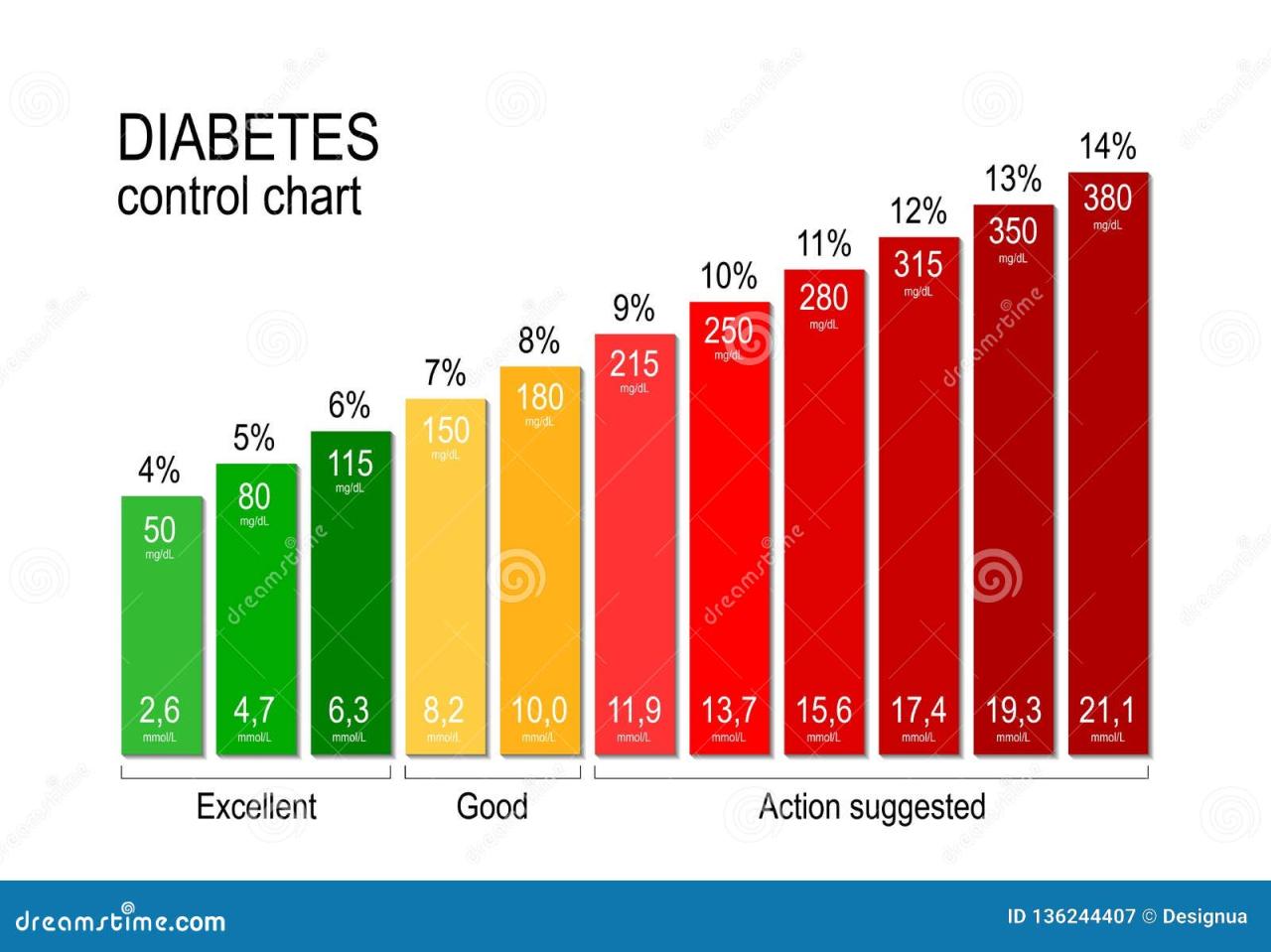
Restricting eating to daytime hours can significantly impact blood glucose levels in individuals with type 2 diabetes. This eating pattern, often referred to as time-restricted eating, can influence how the body processes carbohydrates and regulates blood sugar throughout the day. By strategically managing when we eat, we can potentially improve insulin sensitivity and secretion, leading to better blood sugar control.Daytime eating offers a unique opportunity to observe how our bodies respond to food intake during a period when we are typically more active and our metabolism is functioning at a higher rate.
This contrasts with nighttime eating, when our metabolism slows down, and our bodies may not be as efficient at processing nutrients.
Influence on Blood Glucose Levels Throughout the Day
The timing of meals plays a crucial role in blood glucose management. When we eat only during daytime hours, our bodies have a more consistent opportunity to process glucose, as opposed to a period of intense glucose uptake followed by a prolonged period of lower activity at night. This can lead to a more stable blood glucose profile, reducing the risk of post-meal spikes and promoting a gradual release of glucose into the bloodstream.
Eating only during the daytime can really help manage type 2 diabetes, by regulating blood sugar levels. For a great lunch that won’t leave you crashing later, check out this recipe for a healthy and satisfying meal: lunch recipe avoid energy crash. This kind of mindful meal planning is key to keeping those blood sugar levels stable throughout the day, which is super important for people managing type 2 diabetes.
This, in turn, may improve insulin sensitivity.
Effect on Insulin Sensitivity and Secretion
Restricting eating to daytime hours can potentially improve insulin sensitivity. When our bodies have a period of rest and reduced glucose uptake during the night, the cells become more responsive to insulin. This enhanced sensitivity means that the body can use insulin more effectively to move glucose from the bloodstream into the cells, helping to maintain a healthier blood glucose level.
Furthermore, the consistent daytime eating pattern may lead to a more stable insulin secretion profile. The body’s response to meals is often more predictable, and this predictability may lead to a more effective and balanced insulin release, further improving blood glucose control.
Comparison of Daytime and Nighttime Eating
Daytime eating often correlates with higher levels of physical activity. The combination of activity and food intake during the day can lead to more efficient glucose utilization. Nighttime eating, on the other hand, often occurs when metabolic activity is lower. This can result in a slower processing of glucose and a higher risk of blood glucose spikes.
The body may also struggle to regulate blood glucose levels effectively during the night due to reduced metabolic function.
Potential Variations in Blood Glucose Levels
The following table illustrates a potential comparison of blood glucose levels over a 24-hour period, assuming a daytime-only eating schedule versus a regular schedule. Note that individual responses may vary.
| Time | Daytime-Only Eating | Regular Eating Schedule | Description |
|---|---|---|---|
| 7:00 AM | Normal (pre-meal) | Normal (pre-meal) | Baseline levels before first meal |
| 8:00 AM | Slightly elevated (post-meal) | Elevated (post-meal) | Blood sugar rises after breakfast |
| 12:00 PM | Moderate (mid-day) | Moderate (mid-day) | Blood sugar levels during the day |
| 4:00 PM | Slightly elevated (post-meal) | Elevated (post-meal) | Blood sugar rises after lunch |
| 8:00 PM | Low (resting) | Elevated (post-dinner) | Blood sugar tends to drop after activity in daytime; night-time eating causes a higher blood sugar spike |
| 12:00 AM | Very Low (resting) | High (post-dinner) | Blood sugar continues to be elevated |
| 4:00 AM | Very Low (resting) | Elevated (during night) | Blood sugar tends to remain elevated through the night |
Mechanisms and Potential Explanations
Restricting eating to daytime hours might seem like a simple dietary adjustment, but it could have profound effects on blood sugar control for people with type 2 diabetes. This approach potentially leverages the body’s natural circadian rhythms, which play a crucial role in regulating various metabolic processes, including glucose metabolism. By aligning eating patterns with the body’s internal clock, we might see improvements in how the body processes and utilizes glucose.The physiological mechanisms behind this potential improvement are complex and still being actively researched.
However, preliminary studies and observations suggest several possible pathways through which daytime-only eating could positively influence blood glucose levels. These include improvements in insulin sensitivity, better regulation of glucose production by the liver, and a more balanced metabolic response throughout the day.
Circadian Rhythms and Glucose Homeostasis, How eating only in the daytime can help people with type 2 diabetes
Circadian rhythms are internal, 24-hour cycles that govern many physiological processes. These rhythms are regulated by a central pacemaker located in the brain, the suprachiasmatic nucleus (SCN). The SCN synchronizes bodily functions with the external light-dark cycle. This synchronization is crucial for maintaining optimal metabolic function. Disruptions to these rhythms, such as those caused by irregular eating patterns, can negatively impact glucose homeostasis.
Influence of Daytime-Only Eating on Circadian Rhythms
Shifting eating to daytime hours could potentially re-establish a more natural alignment between eating and the body’s circadian rhythm. This alignment might lead to a more consistent and predictable metabolic response. The body’s internal clock is sensitive to the timing of meals. By restricting meals to daylight hours, the body may be better equipped to respond appropriately to the influx of glucose.
Potential Factors Influencing Blood Glucose Control
| Factor | Potential Mechanism | Possible Impact on Blood Glucose | Example |
|---|---|---|---|
| Insulin Sensitivity | Improved synchronization of insulin release with the body’s natural rhythms. | Reduced need for insulin to regulate blood sugar. | A person eating only during daylight hours may see a more stable insulin response throughout the day. |
| Hepatic Glucose Production | Reduced glucose production by the liver during nighttime hours, when it is typically higher. | Lower blood glucose levels during fasting periods. | Studies have shown that meal timing can affect the liver’s release of glucose, potentially leading to lower fasting glucose levels. |
| Gut Microbiome | Potentially altered gut microbiome composition, which can affect glucose metabolism. | Improved gut health, and a possible improvement in glucose absorption and regulation. | The impact of dietary timing on the gut microbiome is an active area of research. |
| Metabolic Flexibility | Improved ability to switch between different metabolic pathways. | Better adaptation to different energy needs throughout the day. | A more balanced metabolic response can potentially improve overall health and reduce fluctuations in blood glucose. |
Practical Considerations and Strategies
Transitioning to a daytime-only eating schedule requires careful planning and adjustments. This approach offers significant benefits for managing type 2 diabetes, but successful implementation demands a thoughtful strategy to navigate hunger, cravings, and maintaining a balanced diet. Understanding how to effectively manage these aspects is key to long-term adherence and achieving positive health outcomes.
Eating only during the day can be a surprisingly effective strategy for managing type 2 diabetes. It helps regulate blood sugar levels, and can contribute to overall health improvements. However, it’s crucial to remember that while this dietary approach can be beneficial, other serious health concerns, like lung cancer, unfortunately remain a significant threat. In the U.S., lung cancer remains the leading cause of cancer deaths in the U.S.
So, while focusing on daytime eating is a great step for diabetes management, it’s essential to consider a comprehensive approach to health, including regular check-ups and preventative measures.
Implementing a Daytime-Only Eating Schedule
This approach involves consuming all meals and snacks within a specific timeframe during the day, typically 8-12 hours. It’s crucial to select a consistent window that aligns with your daily routine and natural sleep-wake cycle. Consistency is vital for regulating blood sugar and establishing a predictable pattern for your body. Avoid making drastic changes; instead, gradually adjust your eating window over a week or two to allow your body to adapt.
Consider consulting a registered dietitian or diabetes educator for personalized guidance.
Managing Hunger and Cravings During Nighttime Fasting
Managing hunger and cravings during the fasting period is crucial for adherence to the daytime-only eating schedule. Sufficient hydration throughout the day can help alleviate feelings of hunger. Drinking water, unsweetened herbal tea, or water infused with fruits or vegetables can be helpful. Maintaining a balanced diet during the day is also crucial. Include fiber-rich foods, lean proteins, and healthy fats to keep you feeling full and satisfied.
If hunger persists, consult a healthcare professional or registered dietitian to determine the underlying cause.
Eating only during the day can really help manage type 2 diabetes, especially when you consider food safety. Proper food handling and government oversight, like those involved in food safety government inspection , are crucial for everyone’s health, but especially for those with this condition. It’s all about making informed choices about what you eat and when you eat it, and a consistent schedule can be a powerful tool in managing blood sugar levels.
Maintaining a Balanced Diet During the Daytime Eating Window
A balanced diet during the daytime eating window is essential for optimal health and blood glucose control. Prioritize whole, unprocessed foods such as fruits, vegetables, lean proteins, and whole grains. Limit processed foods, sugary drinks, and excessive saturated and unhealthy fats. Consider using portion control to ensure you’re not overeating. Portion sizes should be adjusted to meet your individual needs and activity levels.
Monitoring your calorie intake and macronutrient balance is important to maintain a healthy weight.
Sample Daytime Eating Schedule
| Meal Time | Food Choices (Examples) | Portion Size (Approximate) | Nutrient Distribution |
|---|---|---|---|
| Breakfast (7:00 AM) | Oatmeal with berries and nuts, scrambled eggs with spinach, Greek yogurt with fruit | 1/2 cup oatmeal, 2 eggs, 1 cup Greek yogurt | Complex carbohydrates, protein, healthy fats, vitamins, and minerals |
| Mid-morning Snack (10:00 AM) | Apple slices with almond butter, a handful of almonds, a small portion of mixed vegetables with hummus | 1 medium apple, 2 tbsp almond butter, 1/4 cup almonds | Healthy fats, fiber, vitamins, minerals |
| Lunch (1:00 PM) | Grilled chicken salad with mixed greens and vegetables, lentil soup with whole-wheat bread, fish with roasted vegetables | 4 oz grilled chicken, 1.5 cups salad, 1 cup soup, 2 slices whole-wheat bread | Protein, complex carbohydrates, fiber, vitamins, minerals |
| Afternoon Snack (4:00 PM) | Small handful of mixed nuts, a piece of fruit, a small portion of cottage cheese | 1/4 cup mixed nuts, 1 piece of fruit, 1/2 cup cottage cheese | Healthy fats, fiber, protein |
| Dinner (7:00 PM) | Baked salmon with roasted vegetables, lean beef stir-fry with brown rice, vegetable curry with brown rice | 4 oz salmon, 2 cups vegetables, 1 cup brown rice | Protein, complex carbohydrates, vitamins, minerals, fiber |
Considerations for Specific Populations
Daytime eating, while beneficial for many type 2 diabetes sufferers, isn’t a one-size-fits-all solution. Individual needs and circumstances vary significantly. Understanding how different populations might react to this dietary approach is crucial for safe and effective implementation. This section will delve into considerations for specific groups, including potential challenges and adaptations.
Children and Adolescents
Implementing daytime-only eating for children and adolescents requires careful consideration. Their growing bodies and fluctuating energy needs may be affected by this dietary restriction. A consistent meal pattern with balanced nutrition throughout the day is vital for their development. It’s crucial to consult with a pediatrician or registered dietitian experienced in pediatric nutrition. They can provide personalized advice and ensure the child receives the necessary nutrients and calories for healthy growth and development.
Furthermore, ensuring adequate access to healthy snacks during the daytime is essential.
Pregnant Women
Pregnant women require increased caloric and nutrient intake to support the developing fetus. Daytime eating may not be suitable for all pregnant women, especially those with pre-existing dietary conditions or those experiencing morning sickness. Consult with an obstetrician and a registered dietitian to determine the best dietary approach for maintaining both maternal and fetal well-being. A personalized meal plan that provides adequate nutrient intake throughout the day, encompassing both daytime and nighttime, is paramount for a healthy pregnancy.
Individuals with Certain Medical Conditions
Certain medical conditions may necessitate modifications to the daytime eating schedule. Individuals with conditions like gastroparesis, for instance, might experience difficulties with rapid digestion if meals are consumed solely during the daytime. Individuals with conditions like severe GERD or other digestive issues may require a more gradual approach to the daytime-eating plan. Working closely with a healthcare professional is essential for adapting the plan to specific needs and medical conditions.
Careful monitoring of blood glucose levels and other relevant health indicators is also essential.
Individuals with Irregular Schedules
Shift workers, students with demanding schedules, or individuals with irregular work hours might find it challenging to strictly adhere to a daytime eating schedule. Flexibility is key. Adjusting the eating window to accommodate work or school hours is important. For instance, someone working night shifts might consume their larger meal during the day when they are awake and active.
Meal timing can be adjusted, but it’s critical to ensure that total calorie intake and nutrient balance remain consistent.
Comparing Daytime Eating Schedules
| Age Group/Lifestyle | Meal Timing Considerations | Potential Challenges | Strategies for Adaptation |
|---|---|---|---|
| Children (6-12) | Regular meals and snacks during the day to support growth and development. | Maintaining consistent energy levels throughout the day, especially during periods of increased activity. | Collaborating with parents and educators to ensure adequate access to healthy snacks and meals during school hours. |
| Pregnant Women | Adequate calorie and nutrient intake throughout the day to support fetal development. | Morning sickness, potential digestive issues, and maintaining a balanced schedule with the demands of pregnancy. | Consulting with an obstetrician and registered dietitian for a personalized meal plan. |
| Shift Workers | Adjusting meal timing to align with work hours, while ensuring consistent nutrient intake. | Maintaining a consistent schedule can be difficult with fluctuating work hours. | Planning meals in advance, using meal prepping techniques, and ensuring sufficient hydration and healthy snacks during off-shift periods. |
| Individuals with Irregular Schedules | Flexibility in meal timing, but maintaining a consistent daily intake of calories and nutrients. | Maintaining a consistent intake when schedules vary and avoiding overeating or undereating. | Utilizing meal prepping, portion control, and mindful eating techniques to manage calorie intake. |
Important Caveats and Limitations
Restricting eating to daytime hours can be a valuable tool for managing type 2 diabetes, but it’s crucial to acknowledge potential drawbacks and limitations. While this approach can positively impact blood glucose control, it’s not a universally applicable or risk-free strategy. Individual responses and needs vary significantly, and careful consideration is necessary before adopting this dietary pattern.This section highlights potential downsides, risks, and situations where daytime-only eating might not be appropriate.
Understanding these caveats is vital for making informed decisions about dietary management.
Potential Drawbacks and Risks
Daytime-only eating, while potentially beneficial, can lead to several potential drawbacks and risks. For example, it may disrupt normal eating patterns, potentially affecting social interactions and daily routines. This can lead to increased stress or difficulties in adhering to the regimen. Additionally, a restricted eating window might not be suitable for individuals with specific dietary needs or those who struggle with hunger or cravings.
Situations Where This Approach Might Not Be Appropriate
Certain situations may render daytime-only eating less suitable or potentially harmful. For example, individuals with certain medical conditions, such as those requiring frequent medication or specific nutrient intake throughout the day, may find it challenging or even dangerous to adhere to this eating pattern. Similarly, individuals with a history of eating disorders or those prone to emotional eating might experience increased risk or difficulty with this approach.
Also, consider those with specific nutritional needs, such as pregnant women, children, or those recovering from illness. Individuals on medications that require specific timing with meals may find this pattern incompatible.
Contraindications and Potential Side Effects
| Potential Side Effect | Description | Severity | Contraindications |
|---|---|---|---|
| Disrupted sleep patterns | Changes in sleep quality or quantity, difficulty falling asleep, or waking up frequently. | Mild to moderate | Individuals with pre-existing sleep disorders or those reliant on consistent sleep schedules. |
| Nutrient deficiencies | Inadequate intake of essential vitamins, minerals, or macronutrients if not carefully planned. | Moderate to severe | Individuals with specific nutritional requirements or those who are not skilled in meal planning. |
| Increased hunger and cravings | Stronger feelings of hunger or cravings outside the designated eating window, potentially leading to overeating later. | Mild to moderate | Individuals with a history of eating disorders or those struggling with emotional eating. |
| Reduced energy levels | Fatigue or lack of energy, particularly if the eating window is too short or inadequate nutrients are consumed. | Mild to moderate | Individuals with strenuous physical activity or those who are already experiencing low energy levels. |
| Gastrointestinal issues | Stomach upset, indigestion, or other digestive problems due to rapid shifts in eating patterns. | Mild to moderate | Individuals with existing gastrointestinal issues. |
| Social challenges | Difficulty in participating in social activities involving meals or gatherings. | Mild to moderate | Individuals with strong social ties or who rely on meals as social events. |
Important Considerations
Careful planning and professional guidance are crucial when considering a daytime-only eating approach. Individuals should consult with their healthcare providers or registered dietitians to determine if this approach is appropriate for their specific circumstances. A comprehensive assessment of individual needs and medical history is essential before making any dietary changes. Monitoring blood glucose levels and adjusting the eating window as needed are also vital components of this approach.
Additional Factors Influencing Blood Sugar Control
Daytime eating, while beneficial for managing type 2 diabetes, isn’t the sole factor in blood sugar regulation. Other lifestyle choices significantly impact how well blood glucose levels are controlled. Understanding these interconnected elements is crucial for creating a comprehensive approach to managing the condition effectively.Beyond the timing of meals, other crucial lifestyle factors can impact blood sugar control.
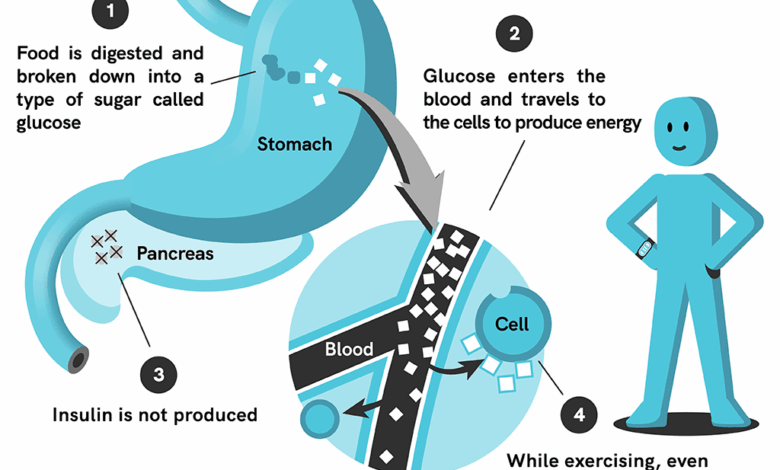
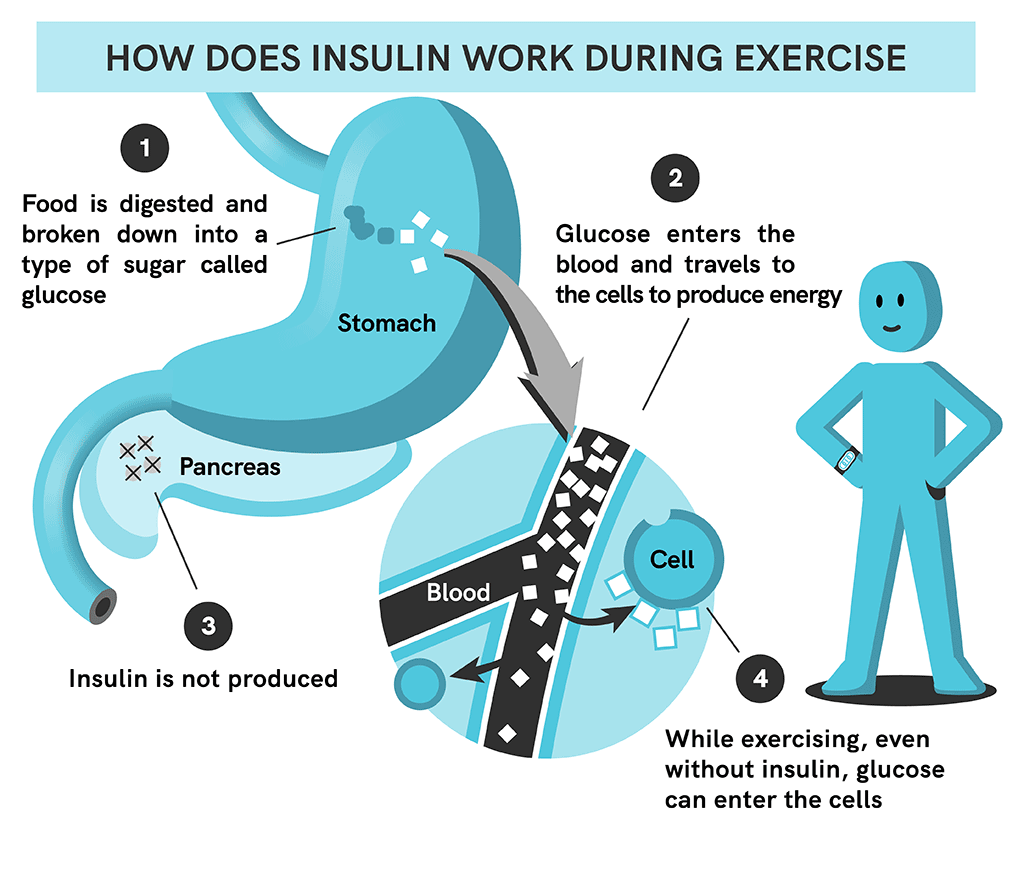
Exercise and Blood Sugar Management
Regular physical activity is essential for individuals with type 2 diabetes. Exercise helps the body use insulin more effectively, lowering blood sugar levels. This effect can persist for hours after exercise, demonstrating the long-term benefits of incorporating regular physical activity into the daily routine. Incorporating exercise into a daytime eating schedule can further enhance blood sugar control. For instance, a brisk walk after lunch can help process the food consumed and minimize post-meal blood sugar spikes.
Stress Management and Blood Sugar Levels
Chronic stress can negatively impact blood sugar control. Stress hormones, such as cortisol, can raise blood glucose levels. Effective stress management techniques, such as meditation, yoga, or deep breathing exercises, can help regulate these hormones and improve blood sugar control. Stress management strategies should be integrated into the daily routine, complementing the daytime eating schedule. For example, incorporating a short meditation session before a daytime meal can potentially help reduce stress-induced blood sugar fluctuations.
Medication Adherence and Blood Sugar Control
Adherence to prescribed medications is critical in managing type 2 diabetes. Consistent medication intake, as directed by a healthcare professional, helps maintain optimal blood sugar levels. This is vital in conjunction with a daytime eating plan. For example, taking prescribed medication before a meal can help the body process the food consumed more efficiently, preventing large blood sugar spikes.
Importance of Professional Guidance
Making significant dietary changes, particularly those impacting meal timing, should always be discussed with a healthcare professional. They can provide personalized advice and guidance tailored to individual needs and health conditions. A healthcare provider can assess the impact of daytime eating on existing medications and overall health. They can also identify any potential interactions or complications. This personalized approach ensures the safety and efficacy of any dietary changes.
Comprehensive Approach to Managing Type 2 Diabetes
| Lifestyle Intervention | Description | Daytime Eating Impact | Considerations |
|---|---|---|---|
| Daytime Eating Schedule | Consuming meals primarily during daytime hours. | Can help regulate blood sugar levels and improve insulin sensitivity. | Consult with a doctor before making significant dietary changes. |
| Regular Exercise | Engaging in physical activity on a regular basis. | Improves insulin sensitivity and helps process food more efficiently. | Consult with a doctor to determine appropriate exercise intensity and duration. |
| Stress Management Techniques | Employing methods to reduce stress levels. | Can help regulate stress hormones, which can impact blood sugar. | Explore various stress management techniques and find what works best for you. |
| Medication Adherence | Taking prescribed medications as directed. | Essential for maintaining stable blood sugar levels in conjunction with daytime eating. | Adhere to the prescribed dosage and schedule to maximize effectiveness. |
Last Point
In conclusion, the concept of daytime-only eating for managing type 2 diabetes presents a compelling possibility for improved blood sugar control. While promising, it’s crucial to remember that this approach isn’t a one-size-fits-all solution. Individual needs and circumstances must be considered, and careful planning, coupled with guidance from healthcare professionals, is essential. Further research is needed to fully understand the long-term effects and optimal strategies for different populations.
This method offers a promising avenue for enhancing diabetes management, but it should be approached with a thorough understanding of its potential benefits and limitations.





