How low vaccination rates contribute to the rise of coronavirus variants is a critical issue. Low vaccination rates create a breeding ground for viral evolution, allowing the virus to mutate and adapt, leading to more transmissible and potentially dangerous variants. This weakened collective immunity makes individuals and communities more vulnerable to severe illness and exacerbates the global health crisis.
This article explores the complex relationship between vaccination rates, viral evolution, and the emergence of new variants. It examines how reduced immunity in a population fuels the selective pressure for more transmissible variants, enabling them to escape immune responses. We’ll also delve into the impact on vulnerable populations, global implications, and strategies to curb future variant emergence.
Low Vaccination Rates and Viral Evolution
Low vaccination rates within a population significantly impact viral evolution, creating a breeding ground for more dangerous and transmissible variants. This vulnerability arises from the reduced collective immunity, leaving a substantial portion of the population susceptible to infection. This susceptibility, in turn, provides the virus with ample opportunity to replicate, mutate, and adapt. The result is a cascade effect, leading to the emergence of variants that can evade existing immunity and potentially cause more severe illness.Reduced immunity within a population allows viruses to circulate freely and undergo a greater number of mutations.
These mutations can lead to changes in the virus’s characteristics, such as its ability to spread more easily or to evade the immune system. A high rate of viral replication, in the absence of a robust immune response, dramatically increases the likelihood of these mutations. This process is crucial for understanding how viruses adapt and evolve, highlighting the importance of widespread vaccination in preventing the emergence of dangerous variants.
Impact of Low Vaccination Rates on Viral Evolution
Low vaccination rates lead to a higher proportion of susceptible individuals in a population. This provides a breeding ground for viral replication and mutation. The virus has more opportunities to interact with and infect individuals, leading to the accumulation of mutations that may result in the emergence of new variants. These variants might exhibit enhanced transmissibility, immune evasion capabilities, or even increased virulence, potentially leading to more severe disease outcomes.
This vulnerability is particularly concerning in the context of highly contagious diseases like COVID-19.
Mechanisms of Variant Emergence in Less-Immunized Populations
Reduced immunity within a population creates an environment where the virus can replicate and mutate more freely. The virus encounters fewer immune responses, allowing for the selection and proliferation of mutations that enhance its ability to spread and infect new hosts. This process is akin to natural selection, where mutations that confer an advantage, such as increased transmissibility, become more prevalent in the population.
These variants can then spread more easily and establish themselves within the community. Examples include the emergence of variants like Delta and Omicron in populations with low vaccination rates.
Selective Pressure and Transmissible Variants
A less-immunized population provides a powerful selective pressure on the virus. The virus, through replication and mutation, is driven to adapt and evolve to overcome the reduced immune response. Mutations that enhance the virus’s transmissibility, such as changes in the spike protein, are more likely to spread and become dominant within the population. This is because these variants are better equipped to infect and spread within a less-immunized population.
Low vaccination rates unfortunately fuel the evolution of coronavirus variants, making the fight against this virus harder. It’s a bit like a domino effect, and it’s truly concerning. While we’re all dealing with these complex issues, it’s interesting to see how pop stars are also grappling with personal struggles, like Taylor Swift’s recent Netflix documentary where she openly discusses her experience with an eating disorder, taylor swift talks eating disorder in new netflix doc.
Ultimately, this highlights the importance of prioritizing public health measures, like vaccination, to help curb the spread of these illnesses and prevent the emergence of more dangerous variants.
This selective pressure directly contributes to the emergence of more transmissible variants, which can further exacerbate the spread of the virus.
Opportunities for Viral Mutations Due to Reduced Immune Response
The reduced immune response within a population allows the virus to replicate with minimal interference from the host’s immune system. This enables the virus to undergo a greater number of mutations, as there are fewer immune checkpoints to select against these changes. The accumulation of these mutations can lead to the emergence of variants with altered characteristics, such as increased transmissibility, immune evasion, or increased virulence.
The absence of a robust immune response provides fertile ground for these changes, creating a dangerous cycle.
Comparison of Viral Characteristics in Highly and Lowly Vaccinated Populations
| Characteristic | Highly Vaccinated Population | Lowly Vaccinated Population |
|---|---|---|
| Viral Replication Rate | Lower, due to widespread immunity | Higher, due to susceptible individuals |
| Mutation Rate | Lower, due to limited viral replication | Higher, due to increased replication opportunities |
| Variant Emergence | Lower, due to robust immunity | Higher, due to high viral replication and mutation |
| Disease Severity | Potentially lower, due to effective immune response | Potentially higher, due to emergence of more virulent variants |
| Transmission Rate | Lower, due to reduced susceptible individuals | Higher, due to high susceptible individuals and transmissible variants |
Impact on Variant Transmission
Low vaccination rates create fertile ground for the evolution and spread of coronavirus variants, significantly impacting transmission dynamics. This vulnerability arises from the interaction between the virus’s inherent ability to mutate and the limited immunity conferred by lower vaccination coverage. The resulting higher viral load and increased contact rates in unvaccinated populations accelerate the emergence and spread of more transmissible variants.The transmission dynamics of variants in populations with low vaccination coverage are complex, influenced by multiple factors.
These include the specific characteristics of the variant (e.g., its ability to bind to and infect cells), the pre-existing immunity in the population, and the frequency of contact between individuals. Importantly, a reduced proportion of vaccinated individuals within a community directly contributes to a higher probability of viral transmission.
Transmission Rate Comparison Across Vaccination Contexts
Understanding how vaccination rates affect variant transmission requires a comparative analysis of transmission rates in different settings. Regions with high vaccination coverage often exhibit lower transmission rates for various variants compared to regions with low vaccination coverage. This difference is attributable to the reduced number of susceptible individuals in highly vaccinated communities, thus limiting the virus’s opportunities for replication and spread.
Illustrative Model of Variant Spread in Low Vaccination Rates
A simplified model depicts a population divided into vaccinated and unvaccinated segments. In a population with low vaccination rates, the variant spreads more rapidly among unvaccinated individuals, due to their lack of acquired immunity. This rapid spread can lead to a higher frequency of mutations, increasing the likelihood of variants with enhanced transmissibility.
Impact of Vaccination Levels on Specific Variants
The impact of vaccination levels on specific variants is evident in various case studies. For instance, in regions with lower vaccination rates, the Delta variant demonstrated a significantly higher transmission rate compared to regions with higher vaccination rates. Similarly, the Omicron variant, while exhibiting high transmissibility across all settings, experienced a reduced impact in regions with higher vaccination rates.
Factors Influencing Transmission Dynamics in Low Vaccination Coverage
Several factors influence the transmission dynamics of variants in populations with low vaccination coverage. High population density, limited access to preventive measures, and socioeconomic factors, like poverty and lack of adequate healthcare, can amplify the spread. These factors, coupled with low vaccination coverage, can create a perfect storm for the emergence and rapid spread of new variants.
Immune Escape and Variant Emergence
Reduced immunity, often a consequence of low vaccination rates, significantly impacts the emergence of coronavirus variants. This weakened collective immunity allows the virus to mutate more freely, leading to variants that are better at evading the immune system and spreading more easily. Understanding these mechanisms is crucial for effective public health strategies to combat the virus.
Mechanisms of Immune Evasion
Reduced immunity from low vaccination rates creates an environment where the virus can more easily replicate and mutate. This process often results in the selection of variants with mutations that allow them to escape pre-existing immunity. This is driven by the natural selection pressures within the host population, as the variants with these advantageous mutations are more likely to replicate and spread.
Mutations Facilitating Immune Escape
Mutations in viral proteins, particularly those that interact with the immune system, are key drivers of immune escape. These mutations can alter the structure of these proteins, making them less recognizable to antibodies or T cells. Examples of such proteins include the spike (S) protein, which is crucial for viral entry into host cells. Changes in the S protein can hinder the binding of antibodies or T cells to the virus, enabling the virus to evade immune responses.
Role of Pre-Existing Immunity in Variant Prevention
Higher vaccination rates, and consequently, a stronger collective immune response, can limit the emergence of new variants. A broader range of pre-existing immunity creates a less hospitable environment for the virus to replicate and evolve into variants that can escape these defenses. This is a critical aspect of public health strategies aimed at preventing future outbreaks and reducing the potential for new variant emergence.
High vaccination rates can essentially reduce the selective pressure for the virus to develop new, immune-evasive mutations.
Summary of Immune Escape Mechanisms
| Variant | Key Immune Escape Mechanisms |
|---|---|
| Alpha (B.1.1.7) | Mutations in the spike protein, altering antibody binding sites, allowing for increased transmissibility. |
| Beta (B.1.351) | Mutations in the spike protein, reducing antibody neutralization, enabling immune evasion. |
| Gamma (P.1) | Mutations in the spike protein, altering receptor binding affinity, potentially increasing transmissibility and immune evasion. |
| Delta (B.1.617.2) | Mutations in the spike protein, enhancing infectivity and reducing antibody neutralization. |
| Omicron (B.1.1.529) | Multiple mutations in the spike protein, significantly reducing antibody neutralization and potentially increasing transmissibility. Its high mutation rate has led to numerous subvariants, each with its own unique set of mutations and immune evasion mechanisms. |
Population Vulnerability and Variants
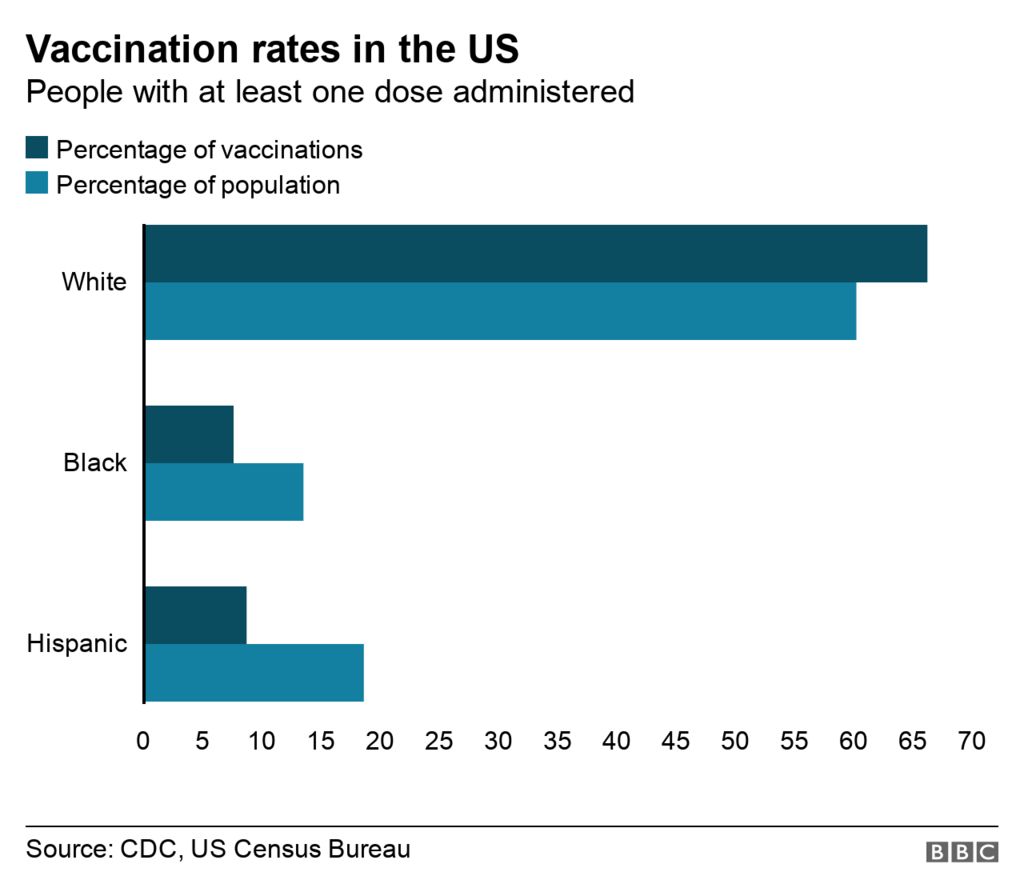
The COVID-19 pandemic highlighted the stark disparities in vulnerability to severe illness across different population groups. Understanding these vulnerabilities and their connection to vaccination rates is crucial for predicting the potential emergence of variants preferentially targeting these susceptible populations. Factors such as pre-existing medical conditions, age, and socioeconomic status significantly influence individual responses to the virus. This interplay underscores the importance of equitable vaccine access and robust public health measures to mitigate the impact of future outbreaks.
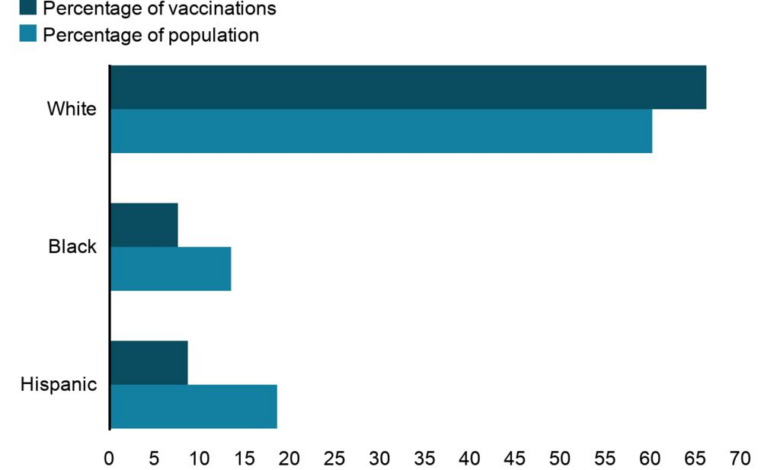
Vulnerable Population Groups and Vaccination Rates
Various population groups exhibit heightened susceptibility to severe COVID-19 outcomes. These include individuals with pre-existing health conditions like diabetes, cardiovascular disease, and chronic respiratory illnesses. Older adults, particularly those over 65, are also at significantly higher risk due to age-related immune system decline. Additionally, racial and ethnic minorities and those living in underserved communities often face systemic barriers to healthcare access, including vaccination.
Low vaccination rates unfortunately fuel the creation of coronavirus variants, which is a real concern. It’s all about the virus needing to adapt to find susceptible hosts, and when people aren’t vaccinated, there are more opportunities for the virus to mutate. This is a frustrating reality, and something we should all be thinking about when considering how important vaccinations are.
While we’re talking about health, it’s interesting to consider the many positives of menopause, such as reasons to thank menopause , and how they impact women’s overall well-being. But ultimately, high vaccination rates are still crucial in preventing the emergence of more variants, and protecting our collective health.
These factors frequently intersect, creating vulnerable subgroups within populations. Lower vaccination rates in these groups can exacerbate the risks associated with variant emergence. For example, regions with lower vaccination rates may experience a disproportionate burden of severe cases, potentially leading to the selection and spread of variants better adapted to infecting these populations.
Impact of Age on Disease Severity and Vaccination Status
Age is a critical factor influencing the severity of COVID-19. Young children generally experience milder symptoms compared to older adults. However, severe outcomes are still possible, and some children develop long-term complications. Elderly individuals, due to a weakened immune response, are more prone to severe illness, hospitalization, and death. Vaccination plays a significant role in mitigating the severity of disease across all age groups.
Fully vaccinated individuals generally experience milder symptoms and reduced risk of severe outcomes compared to unvaccinated individuals, regardless of age.
Variant Virulence in Different Population Segments, How low vaccination rates contribute to the rise of coronavirus variants
Some variants have demonstrated varying degrees of virulence in different population groups. Early studies suggested that certain variants might exhibit a higher propensity to cause severe illness in older adults, while others might preferentially target younger individuals. This complex relationship between variants, population demographics, and vaccination status requires ongoing research to fully understand. For example, the Delta variant demonstrated a higher transmission rate among all age groups, leading to increased hospitalizations and deaths, particularly in unvaccinated individuals.
The Omicron variant, while generally less severe, still presented a significant challenge in terms of widespread infection, even among vaccinated individuals. However, the impact of Omicron on vulnerable populations warrants further investigation.
Vaccination Impact on Disease Severity Across Demographics
The following table illustrates the potential impact of vaccination on disease severity across different demographics. It’s crucial to note that these are general trends and individual experiences can vary widely. More granular data and ongoing research are needed to fully characterize the effect of vaccination in specific subgroups.
| Demographic Group | Vaccination Status | Potential Impact on Disease Severity |
|---|---|---|
| Older Adults (65+) | Vaccinated | Significantly reduced risk of severe illness, hospitalization, and death |
| Older Adults (65+) | Unvaccinated | Higher risk of severe illness, hospitalization, and death |
| Young Adults (18-30) | Vaccinated | Generally milder symptoms and reduced risk of severe illness |
| Young Adults (18-30) | Unvaccinated | Potentially increased risk of severe illness, particularly with certain variants |
| Individuals with Pre-existing Conditions | Vaccinated | Reduced risk of severe illness and complications |
| Individuals with Pre-existing Conditions | Unvaccinated | Significantly increased risk of severe illness and complications |
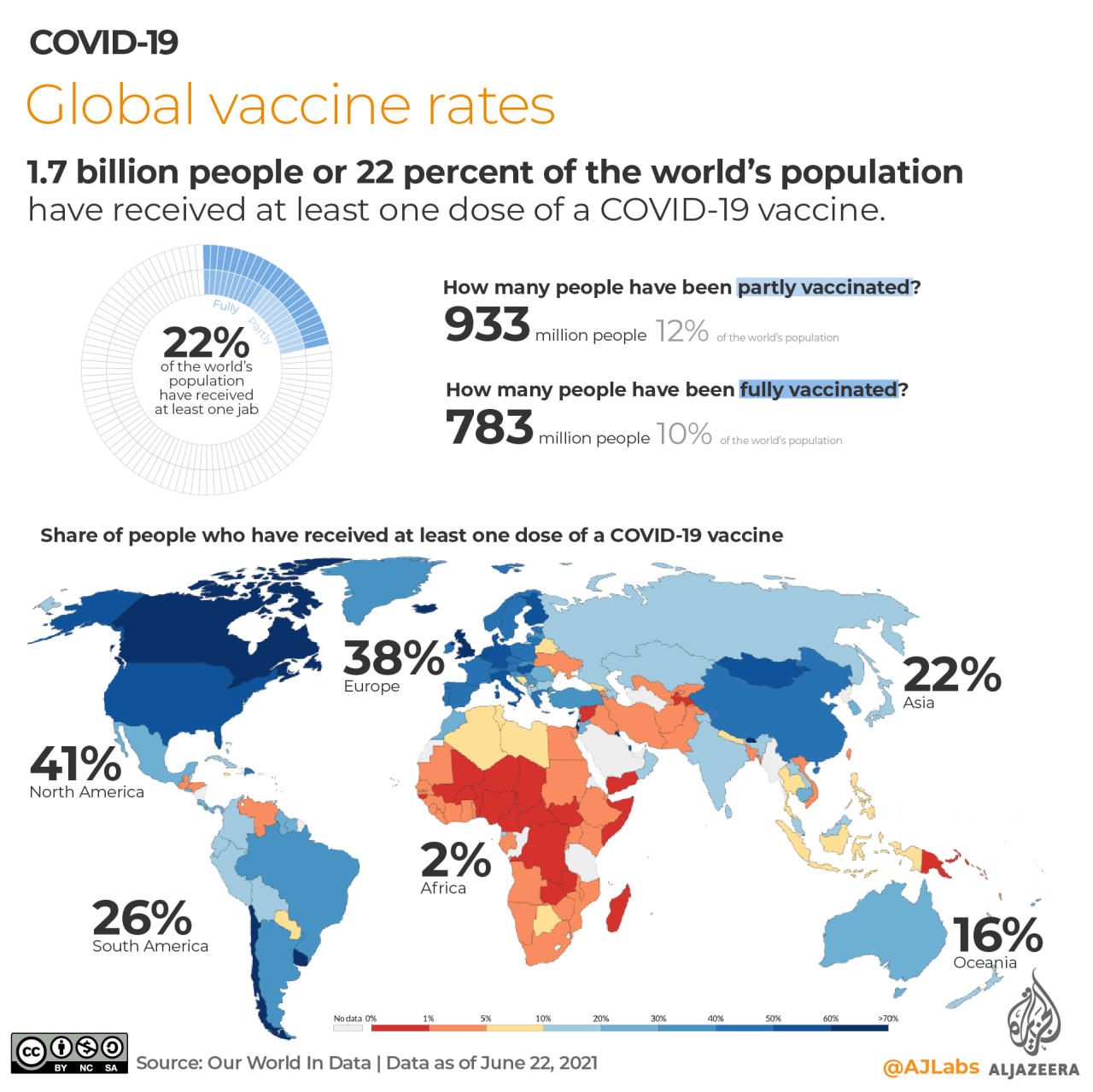
Global Implications of Low Vaccination Rates: How Low Vaccination Rates Contribute To The Rise Of Coronavirus Variants
Low vaccination rates create a breeding ground for the emergence of highly contagious and potentially dangerous coronavirus variants. This phenomenon has significant global implications, impacting not only public health but also economies worldwide. The interconnected nature of our world means that a lack of vaccination in one region can have devastating consequences for the entire globe.The ongoing pandemic highlights the critical importance of global cooperation in vaccination efforts.
Failure to achieve widespread vaccination coverage in all countries exacerbates the risk of new variants emerging, spreading, and causing further disruptions to global health and economic stability. The evolution of the virus is a continuous process, and the lack of immunity in vulnerable populations fuels the development of variants with the potential to evade existing vaccines and therapies.
Impact on Global Health
The emergence of variants in regions with low vaccination rates poses a significant threat to global health. These variants, often more transmissible or better able to evade immune responses, can quickly spread across borders, potentially overwhelming healthcare systems in previously unaffected areas. The experience of the Delta and Omicron variants serves as a stark reminder of the rapid and global impact of viral evolution.
Low vaccination rates create a breeding ground for coronavirus variants, which is a real concern. Think about how important pain relief during labor is for a mother’s well-being. Finding the right approach to manage discomfort during labor, like exploring different options for pain relief, is crucial for a positive birthing experience. Likewise, high vaccination rates protect communities, reducing the chance of new variants emerging and keeping everyone safer.
It’s all connected, and a vital part of public health.
The lack of immunity in unvaccinated populations increases the likelihood of severe illness, hospitalization, and death.
Impact on Global Economies
The emergence of new variants has significant economic repercussions. Lockdowns, quarantines, and disruptions to supply chains, often necessitated by variant outbreaks, can lead to significant economic losses. The economic burden of treating COVID-19 patients, particularly those requiring hospitalization, further strains resources. Furthermore, the unpredictability of new variants and the need for continuous adaptation in public health measures can create considerable uncertainty in the global economy.
The ongoing need for testing, treatment, and preventative measures further adds to economic strain.
Potential for Spread to Previously Unaffected Regions
The spread of variants from low-vaccination areas to previously unaffected regions is a serious concern. Air travel, global trade, and migration patterns contribute to the rapid dissemination of the virus. The consequences can be devastating, leading to surges in cases, hospitalizations, and deaths in regions lacking the infrastructure or resources to effectively manage such outbreaks. Historical examples of infectious disease outbreaks, such as the H1N1 pandemic, illustrate the potential for rapid global spread.
Need for Global Cooperation in Vaccination Efforts
Global cooperation in vaccination efforts is crucial to curbing the emergence of new variants. Sharing data on variant evolution, vaccine development, and treatment strategies can accelerate the response to new threats. Equitable access to vaccines is essential to prevent the emergence of variants in regions with limited resources. This requires a concerted global effort to ensure that everyone has access to effective vaccines.
The development and distribution of vaccines in developing countries is critical to halting the pandemic’s spread.
Summary of Impact of Low Vaccination Rates on Global Health Indicators
| Global Health Indicator | Impact of Low Vaccination Rates |
|---|---|
| Infection Rates | Higher infection rates, particularly in regions with low vaccination rates. |
| Hospitalizations | Increased hospitalizations, especially among unvaccinated populations. |
| Deaths | Higher mortality rates, particularly in vulnerable populations. |
| Economic Impact | Disruptions to supply chains, decreased productivity, and strain on healthcare systems. |
| Public Health Resources | Strain on healthcare systems and public health infrastructure. |
Strategies to Reduce Variant Emergence
The emergence of new coronavirus variants poses a significant threat to global health, particularly in regions with low vaccination rates. Understanding and implementing effective strategies to mitigate variant emergence is crucial to controlling the pandemic and preventing future outbreaks. These strategies must consider the complex interplay between vaccination coverage, viral evolution, and population vulnerability.High vaccination rates act as a critical barrier against variant emergence.
By reducing the virus’s circulation, vaccination limits opportunities for the virus to mutate and generate new, potentially more transmissible or resistant variants. Consequently, strategies to increase vaccination rates are integral to curbing variant evolution.
High Vaccination Coverage: A Cornerstone of Prevention
High vaccination coverage is fundamental in preventing the emergence of new variants. A substantial portion of the population immunized through vaccination reduces the overall viral load within a community. This lowered viral load significantly decreases the frequency of viral replication and transmission, minimizing the opportunities for mutations that could lead to the development of more transmissible or resistant variants.
Vaccination programs targeted towards vulnerable populations are crucial to maximize this effect.
Strategies for Improving Vaccination Rates in Vulnerable Populations
Several strategies can be implemented to enhance vaccination rates within vulnerable populations. These include targeted outreach programs tailored to specific cultural and linguistic needs. These outreach programs must actively engage community leaders, healthcare providers, and community organizations to address concerns and promote vaccination confidence. Furthermore, streamlining vaccination processes, including making appointments more accessible, can improve vaccination rates.
Comparison of Vaccination Strategies
Different vaccination strategies have been implemented globally to control the spread of variants. Some strategies emphasize broad-based vaccination campaigns targeting the entire population. Others focus on high-risk groups, such as healthcare workers or older adults. The effectiveness of each strategy depends on various factors, including the specific variant, the vaccination type, and the population’s characteristics. Comparing these strategies allows for a nuanced understanding of their impact on variant transmission and emergence.
Notably, the effectiveness of vaccination strategies can be evaluated by measuring the proportion of the population immunized, the rate of new variant emergence, and the reduction in severe disease cases.
A Plan for Achieving High Vaccination Rates in a Specific Community
To achieve high vaccination rates within a specific community, a comprehensive plan should be developed. This plan should include detailed strategies for outreach, education, and engagement. For example, community health workers can play a vital role in educating residents about the benefits of vaccination and addressing concerns. Utilizing trusted community leaders to advocate for vaccination is also crucial.
Moreover, establishing convenient vaccination sites, offering incentives for vaccination, and providing accurate and accessible information are essential components of the plan. Regular monitoring and evaluation of the plan’s progress are also vital to ensure its success. Consideration of specific factors, such as language barriers, cultural norms, and socioeconomic disparities, are crucial for tailoring the approach to the community’s needs.
This tailored approach enhances the plan’s efficacy and addresses the specific concerns within the community. For instance, if a community has a history of mistrust in healthcare institutions, the plan should incorporate strategies to build trust and address those concerns directly. Furthermore, the plan should address potential barriers to vaccination, such as transportation issues or scheduling difficulties, to ensure inclusivity and accessibility.
Final Summary
In conclusion, the evidence clearly demonstrates a strong link between low vaccination rates and the proliferation of coronavirus variants. The emergence of these variants poses a significant threat to global health and economic stability. Prioritizing high vaccination coverage, particularly within vulnerable populations, is crucial in mitigating the risk of future outbreaks and variant emergence. Global cooperation and targeted interventions are essential to prevent the further spread of these potentially dangerous variants and to safeguard public health.