How surgery helped fuel the opioid epidemic? This exploration delves into the often-overlooked connection between surgical procedures and the devastating rise of opioid addiction. We’ll examine past pain management practices, the role of different surgical specialties, and the factors that contributed to the over-prescription of opioids, ultimately leading to a crisis that continues to impact our society today.
The opioid crisis is a complex issue with deep roots. From societal pressures to the accessibility of prescription opioids, multiple factors contributed to its escalation. This piece specifically looks at how surgical practices played a significant role in this issue, examining the types of surgery, the frequency of opioid prescriptions, and the alternatives available.
Introduction to the Opioid Epidemic: How Surgery Helped Fuel The Opioid Epidemic
The opioid crisis, a devastating public health emergency, has gripped the United States and other countries for decades. It’s a complex issue with deep roots, stemming from a confluence of factors that escalated over time. This crisis isn’t simply about addiction; it’s about a systemic failure to adequately address the escalating problem, leading to immense suffering and loss.The initial rise of opioid use was often intertwined with the perception of pain management as a critical medical need.
This perception, coupled with increasing marketing of opioid painkillers, played a significant role in their widespread use. Over time, the crisis has evolved, encompassing a range of synthetic opioids and illicit drug markets.
Factors Contributing to the Opioid Crisis
The escalation of the opioid crisis wasn’t a singular event but rather a consequence of interconnected societal pressures and medical practices. Aggressive marketing campaigns for prescription opioids by pharmaceutical companies, combined with a growing societal acceptance of pain management, played a pivotal role. This, coupled with a lack of adequate public health awareness and response, created a fertile ground for the crisis to take root and spread.
Prescription Opioids in the Early Stages
Prescription opioids, initially intended for pain relief, were a major catalyst in the crisis. Doctors often prescribed them liberally, sometimes failing to adequately assess the patient’s needs or potential for addiction. This led to an over-reliance on opioid painkillers for a wide array of conditions, including those that could have been treated with less potent alternatives. The ease of access to these medications, coupled with a lack of comprehensive addiction treatment programs, fueled the crisis’s rapid expansion.
Comparison of Opioid Types
| Opioid Type | Examples | Potential for Abuse | Mechanism of Action |
|---|---|---|---|
| Natural Opioids | Morphine, Codeine | Moderate to high, depending on dosage and individual factors | Bind to opioid receptors in the brain and nervous system, producing pain relief and mood changes. |
| Semi-synthetic Opioids | Oxycodone, Hydrocodone | High, often associated with higher potency and faster onset of action | Synthesized from natural opioids, but with enhanced potency and altered properties. |
| Synthetic Opioids | Fentanyl, Methadone | Extremely high, often leading to rapid and severe overdose risks | Structurally different from natural opioids, frequently offering powerful pain relief and addiction potential. |
The table above provides a concise comparison of various opioid types, highlighting the differences in their chemical structure and potential for abuse. Understanding these distinctions is crucial for developing effective prevention and treatment strategies. The varying potencies and mechanisms of action significantly influence the potential for addiction and overdose.
Surgical Practices and Opioid Prescribing
The opioid crisis, a devastating public health issue, has deep roots in various factors, including the widespread and often inappropriate use of opioid pain relievers, particularly in the context of surgical procedures. This section delves into the surgical practices and prescribing patterns that contributed to the crisis.Surgical procedures, from minor outpatient surgeries to major inpatient procedures, frequently involve pain management as a critical component of patient care.
However, the historical approach to postoperative pain management played a significant role in the subsequent opioid crisis.
Common Surgical Procedures and Post-Operative Pain Management
Common surgical procedures, such as appendectomies, cholecystectomies, and hip replacements, often result in considerable postoperative pain. Historically, pain management strategies frequently relied heavily on opioid analgesics. This was often due to the limited understanding of pain pathways and the availability of effective non-opioid alternatives. The focus on quickly and effectively suppressing pain often led to the routine use of opioids in a variety of surgical settings.
Prevailing Pain Management Paradigms
The prevailing pain management paradigms in the past prioritized the rapid and complete suppression of pain, frequently relying on opioid-based strategies. This approach was often justified by the belief that intense postoperative pain required strong analgesics to ensure patient comfort and recovery. The lack of robust evidence-based guidelines for pain management and the emphasis on patient satisfaction often led to the overprescription of opioids.
Furthermore, the perceived lack of effective alternatives to opioids played a critical role in the widespread use of these medications.
Surgical Specialties and Approaches to Opioid Use
Different surgical specialties exhibited varying approaches to opioid use. For example, orthopedic surgeons, dealing with the significant pain associated with joint replacements, often prescribed higher doses of opioids for longer durations. Similarly, general surgeons, managing a wide range of procedures, also faced challenges in optimizing pain management while minimizing opioid use. Anesthesiologists, though playing a critical role in pain management, often focused on providing adequate pain relief during and immediately following surgery without sufficient consideration for the long-term effects of opioid use.
Frequency of Opioid Prescriptions Following Different Types of Surgery
| Type of Surgery | Frequency of Opioid Prescription (Estimated) |
|---|---|
| Appendectomy | High |
| Cholecystectomy | High |
| Hip Replacement | Very High |
| Tonsillectomy | Moderate |
| Laparoscopic procedures | Variable, generally lower than open procedures |
This table provides a simplified representation of the estimated frequency of opioid prescriptions following various types of surgery. Note that these are estimations, and actual rates varied significantly based on individual patient factors, surgeon preference, and institutional protocols.
The rise of surgical procedures, unfortunately, played a significant role in kickstarting the opioid crisis. Doctors often prescribed powerful painkillers after operations, leading to a reliance on these drugs. Finding effective and safe pain relief options during labor is crucial for expectant mothers, and exploring alternative methods like pain relief during labor could lessen the need for opioids in the long run.
This over-prescription of opioids after surgery then fueled the epidemic, creating a cycle of dependence.
Motivations Behind Prescribing Practices and Impact on Patient Outcomes
The motivations behind prescribing practices were multifaceted. These included a desire to ensure patient comfort, a belief in the efficacy of opioids, and a lack of awareness of the risks associated with long-term opioid use. However, this approach often resulted in adverse outcomes, such as addiction, overdose, and chronic pain issues. Furthermore, the emphasis on quickly suppressing pain frequently overshadowed the need for comprehensive pain management strategies that incorporated non-opioid options.
The focus on rapid recovery often prioritized the quick administration of opioids over a more nuanced approach to pain management. This ultimately contributed to the long-term negative impacts on patient health and well-being.
The Link Between Surgery and Opioid Dependence
The opioid crisis is a complex issue, and the role of surgery in fueling this crisis is a significant part of the story. While pain management after surgery is crucial, the over-prescription of opioids has contributed to a concerning rise in opioid use disorder. This section will delve into the correlation between surgical procedures and the risk of developing opioid use disorder, exploring the mechanisms behind dependence, and highlighting factors that increase the risk.Surgical procedures often necessitate the use of opioids to manage post-operative pain.
However, the long-term consequences of this practice, including the risk of developing physical dependence and addiction, must be carefully considered. This isn’t to say that all surgical patients will become addicted, but the increased exposure to opioids and the potential for misuse significantly contribute to the overall problem.
Correlation Between Surgical Procedures and Opioid Use Disorder
A strong correlation exists between surgical procedures and the risk of developing opioid use disorder. Studies have shown a higher prevalence of opioid use disorder in patients who have undergone certain types of surgeries, particularly those involving significant tissue trauma and prolonged pain. For example, patients undergoing major orthopedic or abdominal surgeries are at a higher risk compared to those having minor procedures.
This increased risk is directly linked to the necessity for potent pain relief during the recovery period.
Mechanisms of Opioid Dependence
Opioids exert their effects by interacting with specific receptors in the brain and nervous system. These receptors, primarily mu-opioid receptors, are involved in pain perception, mood regulation, and reward pathways. When opioids bind to these receptors, they trigger a cascade of events that lead to a temporary reduction in pain signals. However, chronic opioid use can alter the brain’s reward system, leading to a heightened desire for the drug.
The brain adapts to the presence of opioids, and the body can experience withdrawal symptoms if the drug is stopped abruptly. This physical dependence can further escalate into addiction if not managed properly.
The rise of opioid prescriptions after surgery played a significant role in the epidemic. It’s interesting to consider how societal pressures, often reflected in media portrayals, might have contributed to this. For example, the way men and women are stereotyped in the media men vs women media stereotypes could subtly influence how doctors prescribe pain medication, potentially leading to over-prescription in certain cases.
Ultimately, the issue of over-reliance on opioids after surgery remains a complex problem needing multifaceted solutions.
“Chronic opioid use can alter the brain’s reward system, leading to a heightened desire for the drug.”
Factors Increasing the Risk of Opioid Use Disorder After Surgery
Several factors increase the risk of developing opioid use disorder after surgery. These factors include a pre-existing history of substance use disorders, a family history of addiction, and mental health conditions such as depression or anxiety. Furthermore, patients who experience chronic pain or who have a higher perception of pain sensitivity are more susceptible to developing opioid dependence.
The type of surgery itself plays a role; more invasive procedures, involving extensive tissue trauma, can lead to a more intense and prolonged need for opioid pain management.
Long-Term Effects of Opioid Use on Physical Health
Chronic opioid use can have detrimental effects on physical health. The following table Artikels some of the potential consequences:
| Effect | Description |
|---|---|
| Gastrointestinal Issues | Constipation, nausea, vomiting |
| Respiratory Depression | Slowed breathing, potential for respiratory arrest |
| Cardiovascular Problems | High blood pressure, heart rate fluctuations |
| Liver Damage | Increased risk of liver disease |
| Kidney Issues | Impaired kidney function |
| Weakened Immune System | Increased susceptibility to infections |
Post-Surgical Pain Management Alternatives

The opioid crisis has highlighted the urgent need for safer and more effective pain management strategies following surgery. Traditional reliance on opioids often leads to addiction and long-term health problems. Fortunately, a wide array of non-opioid methods are now available and increasingly used in modern surgical practices. These approaches offer significant advantages in minimizing adverse effects while still effectively controlling post-operative discomfort.Moving beyond opioids requires a comprehensive understanding of alternative pain management techniques.
This includes a holistic approach that considers the individual patient’s needs, preferences, and potential risks. The goal is to provide effective pain relief while minimizing the risk of addiction and long-term complications.
Non-Pharmacological Pain Management Techniques
Non-pharmacological methods play a crucial role in post-surgical pain management. These approaches focus on strategies that do not involve medications, providing a valuable alternative to opioids.
- Physical Therapy and Exercise: Post-operative physical therapy programs are vital for restoring function and promoting healing. Regular exercises, tailored to the patient’s specific needs, help to reduce muscle stiffness and improve circulation, contributing to faster recovery and less pain. This is often combined with guided movements and stretching routines. For example, gentle walking exercises on the day after knee replacement surgery can help reduce swelling and promote healing.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can significantly reduce pain and inflammation. Heat therapy improves blood flow, easing muscle tension and discomfort. Cold therapy, on the other hand, reduces swelling and inflammation, which is particularly useful in the initial post-operative period. These methods can be used in conjunction with other treatments for maximum effectiveness.
Prescription painkillers, often prescribed after surgery, played a significant role in the opioid crisis. This unfortunately mirrors the concerning trend of flavored tobacco use rising again among teens, a worrying parallel. The easy access to these powerful drugs, and the subsequent addiction, sadly highlight the need for better pain management strategies and stricter regulations to prevent further suffering.
This is a complex issue, but one that demands our attention.
- Acupuncture and Acupressure: These traditional therapies involve inserting thin needles into specific points on the body (acupuncture) or applying pressure to these points (acupressure). These techniques aim to stimulate the body’s natural pain-relieving mechanisms. Research suggests that these methods can be effective in reducing pain and improving overall well-being, although further studies are needed.
- Mindfulness and Relaxation Techniques: Techniques such as deep breathing exercises, meditation, and guided imagery can help patients manage stress and anxiety, which can contribute to pain perception. Learning these techniques pre- and post-surgery can significantly reduce pain and promote relaxation. For instance, a patient undergoing a major abdominal surgery might benefit from meditation and deep breathing to manage anxiety and reduce pain.
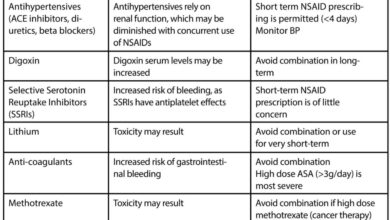
Pharmacological Alternatives to Opioids
While non-pharmacological methods are important, pharmacological alternatives to opioids also play a vital role. These medications provide effective pain relief without the risks associated with opioid use.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs, such as ibuprofen and naproxen, are commonly used to manage mild to moderate pain. They work by reducing inflammation and pain signals. However, NSAIDs can have side effects, including gastrointestinal issues, and should be used cautiously, especially in patients with pre-existing conditions.
- Acetaminophen: This over-the-counter medication is known for its analgesic properties. It is often used in combination with other pain relievers or as a stand-alone medication for mild to moderate pain. Acetaminophen is generally well-tolerated, but it’s crucial to follow dosage recommendations to avoid liver damage.
- Local Anesthetics: These medications can be administered directly to the surgical site to numb the area and provide targeted pain relief. They are often used in conjunction with other pain management strategies. This approach minimizes systemic effects and avoids the potential for addiction.
Comparative Effectiveness of Non-Opioid Pain Management Methods
The effectiveness of different non-opioid pain management methods can vary depending on the individual patient and the type of surgery. A comprehensive approach, incorporating multiple strategies, is often the most effective.
| Method | Effectiveness | Advantages | Disadvantages |
|---|---|---|---|
| Physical Therapy | High | Improves function, promotes healing | Requires commitment and adherence |
| Heat/Cold Therapy | Moderate | Simple, readily available | May not be sufficient for severe pain |
| Acupuncture/Acupressure | Variable | Potentially reduces pain, improves well-being | Limited scientific evidence, individual response varies |
| Mindfulness/Relaxation | Moderate | Reduces stress, improves mood | May not be sufficient for acute pain |
| NSAIDs | High | Effective for inflammation and pain | Potential side effects (e.g., gastrointestinal issues) |
| Acetaminophen | Moderate | Generally well-tolerated | Limited effectiveness for severe pain |
| Local Anesthetics | High | Targeted pain relief | May not be suitable for all types of surgery |
Provider Training and Education
For healthcare providers to effectively implement these alternatives, comprehensive training and education are essential. This includes understanding the mechanisms of action of various non-opioid medications, recognizing potential side effects, and tailoring treatment plans to individual patient needs. Clinicians must also be well-versed in the use of non-pharmacological methods. This requires specialized training in techniques like physical therapy, acupuncture, and mindfulness practices.
Policy and Societal Impacts
The opioid crisis isn’t just a healthcare issue; it’s a societal crisis with profound economic and human consequences. Policies enacted to address the crisis have attempted to balance the need for pain management with the urgent need to curb opioid misuse. Understanding these policies, their successes and failures, is crucial to crafting effective future strategies.
Policies Related to Opioid Prescribing and Pain Management
Numerous policies have been implemented to regulate opioid prescribing and improve pain management practices. These regulations aim to reduce the availability of opioids and promote safer alternatives. Key aspects of these policies include:
- Increased monitoring of opioid prescriptions: This involves stricter regulations on prescribing practices, including mandatory reporting of suspicious opioid use and implementation of electronic prescribing systems to track and monitor prescriptions. For example, states have implemented prescription drug monitoring programs (PDMPs) to track opioid prescriptions, enabling healthcare providers to identify patients at risk for misuse.
- Promoting non-opioid pain management options: Policies encourage the use of non-pharmacological therapies such as physical therapy, acupuncture, and counseling to address chronic pain. This approach recognizes that pain management should encompass a wider range of interventions beyond medication.
- Establishing guidelines for opioid prescribing: Standardized guidelines for opioid prescribing have been developed by professional organizations and government bodies. These guidelines aim to reduce the risk of opioid misuse by recommending lower doses, shorter durations, and alternative pain management options whenever possible. For example, the CDC’s guidelines for prescribing opioids for chronic pain emphasize the need for careful consideration of the risks and benefits of opioid use and encourage the use of non-opioid alternatives.
Role of Healthcare Providers in Preventing Opioid Misuse
Healthcare providers play a critical role in mitigating the opioid crisis. Their awareness and adherence to prescribing guidelines, combined with an understanding of patient needs and risk factors, are paramount.
- Educating patients about risks: Healthcare providers must educate patients about the potential risks of opioid misuse, including addiction, overdose, and other adverse effects. This includes open communication about alternative pain management strategies.
- Comprehensive pain assessment: Providers need to conduct thorough pain assessments, evaluating the source and severity of pain to develop a comprehensive treatment plan. This includes exploring non-opioid options and patient preferences.
- Collaboration with patients and families: Effective pain management necessitates collaborative efforts involving patients, families, and other healthcare professionals. This includes regular communication and shared decision-making.
Societal Impacts of the Opioid Crisis, How surgery helped fuel the opioid epidemic
The opioid crisis has had a devastating impact on society, impacting not only individuals but also the economy and communities.
- Economic costs: The economic costs of the opioid crisis are substantial, encompassing healthcare expenditures, lost productivity, and criminal justice costs. For example, studies have shown that the opioid crisis has significantly increased healthcare costs, impacting insurance premiums and overall economic productivity.
- Loss of life: The crisis has led to a substantial increase in overdose deaths. The sheer scale of this loss of life underscores the urgency of addressing the crisis.
- Community disruption: The opioid crisis has severely disrupted communities, impacting social structures and institutions. This includes increased crime rates, family breakdown, and the erosion of trust in healthcare systems.
Key Policy Changes in Response to the Opioid Crisis
“The opioid crisis demands a multifaceted approach that encompasses policy changes, healthcare provider education, and community support. The goal is to reduce opioid use, improve pain management practices, and address the societal impacts of this crisis.”
Challenges and Successes in Addressing the Opioid Crisis
Addressing the opioid crisis presents significant challenges, including overcoming entrenched prescribing patterns, fostering patient trust, and ensuring access to effective treatment. However, there have also been notable successes, including increased awareness, policy changes, and the development of innovative treatment options.
Future Trends and Prevention Strategies
The opioid crisis, significantly fueled by surgical practices, demands proactive and multifaceted approaches to prevent future misuse and promote healthier pain management strategies. Understanding the evolving landscape of opioid use and pain management is crucial for implementing effective prevention strategies. Addressing the underlying factors contributing to opioid dependence, and fostering a culture of safer pain management, is essential for mitigating the crisis’s long-term impact.
Forecasting Future Trends in Opioid Use and Pain Management
Predicting future trends in opioid use and pain management requires analyzing current data and considering potential societal shifts. Technological advancements, evolving public health initiatives, and shifts in medical practices are all likely to play a role.
| Trend | Potential Impact | Example |
|---|---|---|
| Increased use of non-opioid pain relievers | Potentially reduced reliance on opioids for acute and chronic pain management | Wider adoption of NSAIDs and other non-opioid pain medications |
| Emphasis on multimodal pain management | Lower opioid prescriptions for post-surgical patients | Combination of physical therapy, psychological support, and non-pharmacological approaches |
| Advancements in pain management technologies | Enhanced pain relief without opioids, improved patient outcomes | Development of targeted nerve blocks, minimally invasive surgical techniques |
| Growing awareness of opioid misuse | Increased scrutiny on opioid prescribing practices, improved patient education | Public campaigns and educational programs promoting safe opioid use |
| Increased focus on preventative care | Reduced need for opioid pain management | Early intervention for chronic pain conditions, proactive measures to avoid surgery when possible |
Strategies for Preventing Opioid Misuse After Surgery
Implementing strategies to prevent opioid misuse after surgery is paramount. Proactive measures must be integrated into the surgical process, emphasizing patient education and alternative pain management options.
- Patient Education: Comprehensive pre-operative education empowers patients with knowledge about pain management alternatives, risks of opioid misuse, and responsible medication use. This includes providing clear instructions on how to manage post-operative pain without relying solely on opioids.
- Multimodal Pain Management Plans: Surgical teams should develop and implement comprehensive multimodal pain management plans incorporating non-pharmacological strategies like physical therapy, ice packs, and psychological support, in addition to appropriate pharmacological alternatives to opioids. This approach provides a holistic strategy for pain relief, minimizing reliance on opioids.
- Opioid-Sparing Medications: Prioritize using non-opioid analgesics, such as acetaminophen and NSAIDs, whenever possible, in conjunction with other methods of pain management.
- Proper Disposal of Medications: Emphasize proper disposal methods for unused opioids to prevent diversion and misuse.
Educational Initiatives Aimed at Reducing Opioid Overprescription
Educational initiatives are crucial for reducing opioid overprescription. These programs should target healthcare providers and patients alike, fostering a shared understanding of safer pain management practices.
- Continuing Medical Education: Offer comprehensive continuing medical education programs for healthcare professionals to update their knowledge on best practices for opioid use and safer pain management strategies. This should include practical guidance on multimodal pain management strategies, as well as the risks of opioid overprescription.
- Physician Training Programs: Integrate training programs that emphasize the importance of non-opioid pain management techniques into medical school curriculums and residency programs.
- Public Awareness Campaigns: Public health campaigns should promote understanding of the risks associated with opioid misuse and highlight safer pain management alternatives.
Best Practices for Managing Chronic Pain Without Opioids
Chronic pain management should prioritize non-pharmacological and multimodal approaches. These methods should be considered first-line treatments, with opioids used judiciously, only when other options are insufficient.
- Physical Therapy: Physical therapy can effectively manage pain and improve function, often minimizing the need for opioid pain relievers.
- Cognitive Behavioral Therapy (CBT): CBT can help patients cope with chronic pain by modifying their thoughts and behaviors related to pain.
- Mindfulness and Meditation: Mindfulness practices can help patients manage pain perception and stress, potentially reducing the need for opioid pain medication.
- Acupuncture and other alternative therapies: In some cases, alternative therapies can be beneficial in managing chronic pain.
The Role of Public Health Initiatives in Addressing the Opioid Crisis
Public health initiatives play a critical role in mitigating the opioid crisis. These initiatives must be comprehensive, addressing prevention, treatment, and recovery.
- Increased Funding for Research: Increased funding for research into innovative pain management techniques and the development of non-opioid alternatives is essential.
- Community-Based Programs: Community-based programs focused on opioid prevention, treatment, and recovery can provide vital support for individuals and families affected by the crisis.
- Collaboration between Healthcare Providers and Public Health Officials: Stronger collaborations between healthcare providers and public health officials are necessary to develop comprehensive strategies for addressing the crisis.
Conclusive Thoughts
In conclusion, the link between surgery and the opioid epidemic is undeniable. Past pain management strategies, often relying heavily on opioids, inadvertently fueled a crisis that has had profound consequences for individuals and communities. This discussion highlights the critical need for alternative pain management techniques, better education for healthcare providers, and comprehensive policy changes to address the issue.
Looking forward, prevention strategies and public health initiatives are crucial to mitigate future risks and ensure safer, more effective pain management practices.