How telemedicine makes healthcare more accessible for people with obesity is a game-changer. Traditional healthcare often presents significant hurdles for those struggling with obesity, from scheduling difficulties to geographical limitations. Telemedicine offers a flexible and convenient alternative, enabling remote consultations, personalized treatment plans, and ongoing support, ultimately making care more attainable and empowering.
This article delves into how telemedicine platforms and technologies are revolutionizing obesity management. We’ll explore the specific benefits, address common challenges, and provide a comprehensive overview of the evolving landscape of telemedicine in obesity care.
Introduction to Telemedicine for Obesity Management: How Telemedicine Makes Healthcare More Accessible For People With Obesity
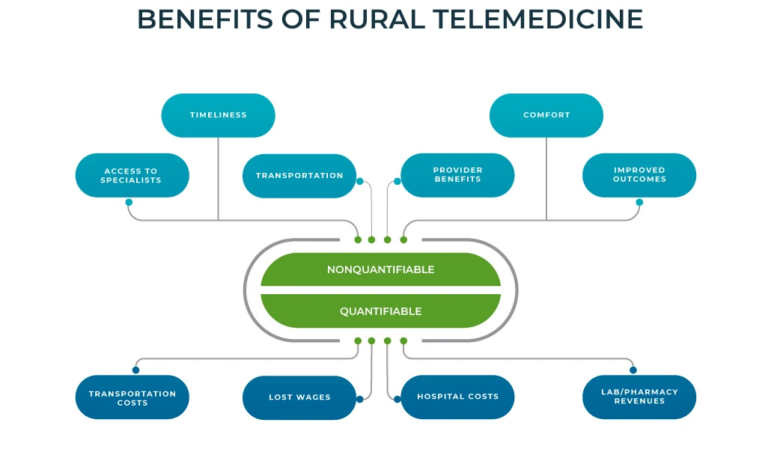
Telemedicine is revolutionizing healthcare by expanding access to care, particularly for individuals facing challenges in accessing traditional in-person appointments. In the context of obesity management, telemedicine offers a convenient and often more accessible pathway to support, monitoring, and treatment. This approach empowers individuals to actively participate in their weight management journey from the comfort of their homes, fostering a sense of control and potentially leading to better long-term outcomes.Telemedicine, in essence, leverages technology to deliver healthcare services remotely.
This includes virtual consultations, remote monitoring, and the delivery of educational resources. Its application in obesity management addresses the unique needs of patients, including those with mobility limitations, geographical barriers, or limited access to specialist care. Telemedicine allows for consistent communication between patients and healthcare providers, enabling personalized support plans and adjustments tailored to individual needs and progress.
Definition of Telemedicine in Obesity Management
Telemedicine in obesity management encompasses the use of digital tools and technologies to provide healthcare services related to weight management remotely. This includes virtual consultations with healthcare professionals, remote monitoring of vital signs and lifestyle factors, and access to educational resources and support groups.
General Principles of Telemedicine for Obesity Management
Key principles underpinning telemedicine in obesity management include accessibility, convenience, and personalized care. Telemedicine can address geographical limitations, scheduling difficulties, and time constraints, allowing for more frequent communication and support than traditional in-person appointments. It fosters a sense of empowerment by enabling patients to actively participate in their care plans and progress monitoring. The remote nature of these services also provides an opportunity for a more continuous and comprehensive approach to care.
Telemedicine is a game-changer for folks with obesity, making appointments and follow-ups much easier. Navigating the healthcare system can be extra tough when you’re dealing with the physical demands of a pandemic and the emotional toll of the associated burnout, especially in the messy middle of it all. Burnout in the messy middle of a pandemic can seriously impact mental and physical health, but telemedicine helps bridge the gap, providing crucial support and resources for those needing them most, even those with obesity.
This remote access makes a real difference in improving health outcomes.
Examples of Telemedicine Platforms and Technologies
Several platforms and technologies facilitate telemedicine for obesity management. Video conferencing software like Zoom and Skype are commonly used for virtual consultations. Wearable devices and mobile apps can track activity levels, sleep patterns, and dietary intake, providing valuable data for personalized interventions. Health-focused apps, including those designed specifically for weight management, offer support, education, and community interaction.
Specialized software platforms provide secure data storage and management for patient information. These various platforms and technologies work together to create a comprehensive telemedicine experience.
Addressing Unique Needs of People with Obesity
Telemedicine offers tailored solutions for the diverse needs of people with obesity. For individuals with mobility limitations, virtual consultations eliminate the need for travel. Remote monitoring tools provide continuous data collection, allowing healthcare providers to track progress and adjust care plans in real-time. Telemedicine can also facilitate access to support groups and educational resources, creating a supportive community that encourages adherence to treatment plans.
Moreover, the digital nature of telemedicine may decrease social stigma associated with obesity-related healthcare needs.
Table: Telemedicine Platforms for Obesity Management
| Platform Type | Features | Accessibility Considerations (for people with obesity) |
|---|---|---|
| Video Conferencing | Virtual consultations, physician-patient interaction, remote diagnosis, and prescription refills (where permitted). | Reduces travel barriers for individuals with mobility issues. Enables consultations from home, which is often more convenient. |
| Wearable Devices/Mobile Apps | Continuous monitoring of activity, sleep, and dietary intake; personalized insights, goal setting, and progress tracking. | Provides objective data for assessment and modification of care plans. Offers support and motivation through tracking and personalized feedback. |
| Health-focused Apps | Education resources, support groups, personalized meal plans, and exercise routines. | Offers readily available resources and support from a community of individuals facing similar challenges. |
Enhanced Access to Care for Obese Individuals
Telemedicine is revolutionizing healthcare access, and this is especially true for individuals with obesity. Traditional healthcare systems often present significant barriers to care for obese patients, leading to delayed diagnoses and inadequate treatment plans. Telemedicine offers a powerful solution by addressing these obstacles and fostering improved health outcomes.Telemedicine offers a unique opportunity to enhance the overall experience for obese patients, bridging the gap between need and access.
It streamlines the process, providing a more convenient and comfortable way to receive the care they require. By embracing these advancements, we can work towards a more inclusive and equitable healthcare system.
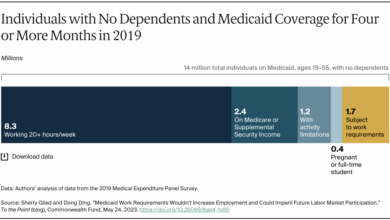
Barriers to Traditional Healthcare Access for Obese Individuals
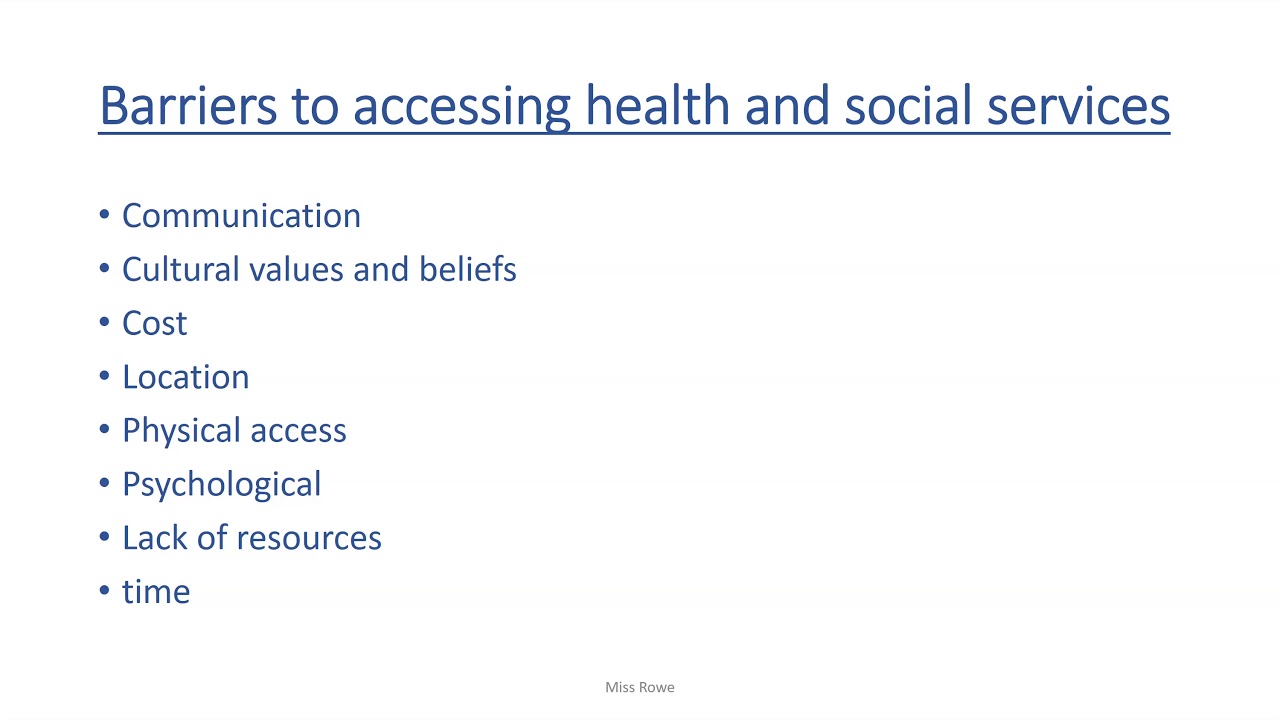
Many factors contribute to the difficulties obese individuals face in accessing traditional healthcare. Physical limitations, like mobility issues, can make in-person visits challenging and time-consuming. Additionally, financial constraints and lack of transportation options are significant obstacles. Stigma and discrimination from healthcare providers can also deter obese patients from seeking care. These barriers can lead to delayed diagnoses, inadequate treatment, and a cycle of worsening health.
In-Person vs. Telemedicine Appointments for Obese Patients
In-person appointments, while offering direct interaction, may pose practical difficulties for obese patients. Scheduling, travel, and potential discomfort during examinations can create significant challenges. Telemedicine appointments, on the other hand, offer a more flexible and convenient alternative. Virtual consultations eliminate the need for travel and can be scheduled around the patient’s availability. This increased accessibility can lead to more frequent and timely medical check-ups.
Overcoming Geographical Limitations with Telemedicine
Telemedicine effectively eliminates geographical limitations. Patients in rural areas or those with limited mobility can now access specialists and healthcare professionals without the need for extensive travel. This expands access to care for individuals who previously faced significant barriers due to their location. Telemedicine empowers these individuals by connecting them with the care they need, regardless of their physical location.
Reducing Wait Times for Obese Patients
Wait times for appointments are a significant concern for obese patients, often leading to delayed diagnoses and treatment. Telemedicine can play a crucial role in reducing these wait times. Virtual consultations allow for quicker scheduling and can expedite the diagnostic process, leading to earlier interventions. This streamlined approach can significantly improve patient outcomes and quality of life.
Role of Remote Monitoring in Improving Access and Engagement
Remote monitoring tools, integrated with telemedicine platforms, offer a valuable means of enhancing engagement and improving access to care for obese patients. These tools enable continuous tracking of vital signs, medication adherence, and lifestyle choices, empowering patients to actively participate in their care. This proactive approach fosters a stronger doctor-patient relationship and promotes better health outcomes.
Cost-Effectiveness of Telemedicine vs. Traditional Care
| Feature | Telemedicine | Traditional Care |
|---|---|---|
| Initial Consultation Cost | Lower due to reduced overhead | Potentially higher due to travel and facility costs |
| Follow-up Visits | Significantly lower due to virtual nature | Higher due to travel and appointment scheduling |
| Travel Costs | Eliminated | Significant, especially for patients in rural areas or with mobility limitations |
| Time Commitment | Reduced, as appointments can be scheduled around patients’ schedules | Higher due to travel time, waiting time, and in-person consultation time |
| Overall Cost | Potentially lower, especially for long-term management | Potentially higher due to added travel and in-person costs |
Telemedicine has the potential to significantly reduce healthcare costs while simultaneously improving access and engagement for obese patients.
Telemedicine Tools and Techniques for Obesity Management
Telemedicine offers a powerful new approach to obesity management, enabling individuals to receive personalized care and support from the comfort of their homes. By leveraging technology, healthcare providers can connect with patients, monitor their progress, and tailor interventions to their specific needs, ultimately improving outcomes. This personalized approach is particularly beneficial for obese individuals, who may face barriers to accessing traditional healthcare services.Telemedicine platforms can overcome geographical limitations and scheduling difficulties, fostering a more accessible and convenient care experience for people with obesity.
The ability to monitor patients remotely, coupled with the integration of various tools for tracking progress, enhances the effectiveness of obesity management programs.
Remote Patient Monitoring
Remote patient monitoring (RPM) is a key component of telemedicine in obesity management. It allows healthcare providers to continuously track vital health data without requiring frequent in-person visits. This constant monitoring provides valuable insights into patients’ progress and helps identify potential issues early on, enabling proactive interventions. RPM tools can facilitate the collection of data on weight, activity levels, and dietary intake, contributing to a more comprehensive understanding of the patient’s overall health.
This data-driven approach is essential for personalized interventions.
Tools for Weight Tracking, Activity Monitoring, and Dietary Logging
Several telemedicine platforms offer dedicated tools for tracking weight, activity, and dietary intake. Weight tracking apps often integrate with wearable devices, providing a seamless and convenient way to monitor changes in body weight. Similarly, activity monitoring apps use data from fitness trackers to record steps, calories burned, and other metrics related to physical activity. Dietary logging apps help patients record the food they consume, enabling the identification of patterns and potential areas for improvement in their diet.
These tools provide patients with a greater level of self-awareness and control over their health journey.
Examples of Telemedicine Tools for Obesity Management
| Tool | Specific Functions | Potential Impact on Obese Patients |
|---|---|---|
| Weight-tracking apps | Record weight, track trends, set goals | Improved self-awareness, accountability, and motivation for weight loss. |
| Fitness trackers and apps | Monitor activity levels, steps taken, calories burned | Increased physical activity, improved motivation for exercise, and better understanding of activity patterns. |
| Dietary logging apps | Record food intake, analyze nutritional content, identify unhealthy patterns | Enhanced dietary awareness, identification of nutritional deficiencies or excesses, support for dietary modifications. |
| Health Management Platforms | Centralized hub for all health data, integration with wearables and apps | Comprehensive view of patient’s health status, easier data analysis and reporting for healthcare providers. |
Telehealth in Supporting Behavioral Interventions
Telehealth plays a crucial role in supporting behavioral interventions for obesity. Virtual support groups provide a safe and encouraging environment for patients to connect with peers facing similar challenges. These groups offer a sense of community and shared experiences, boosting motivation and adherence to treatment plans. Virtual counseling sessions can help patients develop healthy coping mechanisms, address emotional factors contributing to overeating, and create personalized strategies for weight management.
These interventions help patients understand and address the underlying reasons behind their weight challenges.
Virtual Support Groups and Counseling Sessions
Virtual support groups for weight management offer a supportive community environment. Participants can share experiences, provide encouragement, and hold each other accountable. These groups often have moderators who guide discussions and provide support. Similarly, virtual counseling sessions can address emotional eating, stress management, and other behavioral factors influencing weight. Counselors can provide personalized guidance, develop coping strategies, and empower patients to make lasting lifestyle changes.
The convenience and accessibility of virtual support groups and counseling sessions make them particularly beneficial for individuals with obesity.
Secure Communication and Data Privacy
Secure communication and data privacy are paramount in telemedicine for obesity management. Robust encryption protocols and secure platforms are essential to protect sensitive patient information. Compliance with relevant privacy regulations (e.g., HIPAA in the US) is critical to ensure patient confidentiality and trust. This focus on secure communication and data privacy ensures that patients feel comfortable sharing their personal health information and fosters a safe and reliable environment for their healthcare journey.
Addressing Specific Needs of Obese Patients
Telemedicine offers a powerful tool to improve access to care for individuals with obesity, but its effectiveness hinges on addressing the unique needs and concerns of this patient population. Beyond simply offering virtual appointments, successful telemedicine programs must prioritize personalized care, cultural sensitivity, and a robust understanding of the physical and emotional challenges obese individuals face. This proactive approach fosters trust, promotes adherence to treatment plans, and ultimately leads to better health outcomes.
Specific Health Needs and Concerns
Obese patients often experience a range of physical and emotional health concerns. These can include chronic conditions like type 2 diabetes, hypertension, and sleep apnea, as well as concerns about body image, social stigma, and emotional well-being. Telemedicine can effectively address these concerns by providing ongoing monitoring, personalized education, and access to mental health support. Recognizing and proactively addressing these issues is crucial for successful treatment and improved quality of life.
Telemedicine is a game-changer for folks struggling with obesity, offering convenient appointments and virtual consultations. While worrying news like the recent discovery of a new swine flu in China, new swine flu discovered in pigs in china , highlights the importance of global health awareness, telemedicine’s ability to provide crucial support for weight management and related health issues remains a valuable resource.
This access to care, regardless of location or mobility challenges, makes a real difference in the lives of many.
Culturally Sensitive Care
Cultural sensitivity is paramount in telemedicine, especially when addressing obesity. Different cultural backgrounds and beliefs influence attitudes towards weight management and healthcare. Telemedicine platforms should be designed to accommodate diverse communication styles, preferences, and dietary traditions. This includes offering multilingual support and culturally appropriate educational materials. Providers should also be trained to understand and respect the cultural context surrounding weight management.
Supporting Diverse Populations and Needs
Obesity affects individuals across diverse populations, with varying levels of physical ability, socioeconomic status, and access to resources. Telemedicine can bridge these gaps by providing accessible care in remote areas, offering flexible scheduling, and utilizing assistive technologies. The goal is to provide personalized solutions that meet the specific needs of each individual, irrespective of their background or circumstances.
This requires a thorough understanding of the barriers to care and a proactive effort to overcome them.
Adapting to Different Levels of Physical Ability
Telemedicine can be adapted to accommodate individuals with varying levels of physical ability. This includes providing options for remote monitoring of vital signs, encouraging exercise regimens that can be performed at home, and facilitating access to assistive devices. The goal is to make care as accessible and practical as possible, encouraging participation and adherence to treatment plans.
Personalized Treatment Plans
Telemedicine platforms can be leveraged to create personalized treatment plans for obesity. These plans can integrate dietary recommendations, exercise routines, and behavioral modifications, all tailored to the individual’s specific needs and preferences. Telemedicine allows for ongoing monitoring and adjustments to the plan, ensuring that it remains relevant and effective throughout the treatment process. This personalized approach fosters a strong patient-provider relationship and promotes adherence to the prescribed plan.
Table: Telemedicine Solutions for Obesity Management
| Patient Need | Telemedicine Solution | Potential Challenges |
|---|---|---|
| Access to routine monitoring | Remote blood pressure and glucose monitoring, virtual weight tracking | Technical issues, patient motivation, adherence to monitoring |
| Dietary counseling | Virtual nutrition consultations, personalized meal planning, access to dietitian services | Lack of hands-on interaction, difficulty in accurately assessing dietary intake |
| Physical activity guidance | Virtual exercise programs, access to certified trainers, home-based exercise routines | Lack of equipment, patient motivation to engage in physical activity |
| Mental health support | Teletherapy sessions, access to mental health professionals | Privacy concerns, patient reluctance to discuss sensitive issues |
| Cultural sensitivity | Multilingual support, culturally appropriate educational materials, training for providers | Difficulty in understanding cultural nuances, potential language barriers |
Improving Engagement and Adherence to Treatment
Telemedicine offers a powerful opportunity to enhance patient engagement and adherence to weight management plans, particularly for individuals with obesity. Traditional healthcare settings often present challenges for these patients, leading to frustration and reduced motivation. Telemedicine’s flexibility and personalized approach can address these issues, fostering a more supportive and empowering environment for weight loss journeys.Traditional healthcare settings can be challenging for obese patients due to factors like long wait times, impersonal interactions, and the perceived lack of personalized attention.
This can lead to feelings of discouragement and difficulty adhering to prescribed weight management plans. Telemedicine, with its ability to provide remote consultations, personalized feedback, and ongoing support, can significantly improve patient engagement and adherence.
Telemedicine Strategies for Enhanced Engagement, How telemedicine makes healthcare more accessible for people with obesity
Telemedicine offers various strategies to motivate and support patients in their weight loss journeys. Regular virtual check-ins, progress monitoring tools, and interactive educational resources can foster a sense of accountability and empowerment. Personalized feedback and tailored recommendations, delivered virtually, can address individual needs and preferences more effectively than a one-size-fits-all approach. These personalized interactions cultivate a stronger therapeutic alliance, encouraging patients to actively participate in their care.
This active participation, in turn, often leads to increased adherence to treatment plans.
Motivational Interviewing in Virtual Settings
Motivational interviewing (MI) techniques are crucial for fostering intrinsic motivation and promoting self-efficacy in weight management. Virtual platforms allow for flexible application of MI principles. Empathetic listening, open-ended questioning, and reflective listening, all fundamental components of MI, can be effectively employed in virtual consultations. Recognizing and affirming patients’ strengths and successes, even small ones, can greatly boost motivation and confidence.
MI in a virtual setting allows for ongoing dialogue, empowering patients to explore their own motivations and develop personalized strategies.
Promoting Long-Term Weight Management Through Continued Support
Telemedicine can effectively support long-term weight management through ongoing support and encouragement. This includes proactive follow-up appointments, virtual support groups, and access to online resources. By fostering a sense of community and providing ongoing support, telemedicine can help patients maintain their progress and avoid relapses. Regular virtual check-ins and progress reviews act as checkpoints to address any challenges or setbacks early on, promoting sustainable behavior changes.
This sustained support system is crucial for long-term weight management success.
Table: Telemedicine Interventions for Obesity Management
| Intervention Type | Implementation Details | Potential Outcomes (Engagement and Adherence) |
|---|---|---|
| Personalized Virtual Consultations | Regular virtual appointments with a healthcare provider for personalized feedback, goal setting, and adjustments to the treatment plan. | Increased patient engagement, enhanced understanding of treatment plan, improved adherence to recommendations. |
| Progress Tracking and Monitoring Tools | Using mobile apps or online platforms to track weight, diet, and exercise progress. Sharing this data with the healthcare provider. | Increased accountability and motivation, better visualization of progress, improved adherence. |
| Virtual Support Groups | Facilitated online groups connecting patients for peer support, sharing experiences, and encouragement. | Enhanced social support, increased motivation, improved coping mechanisms for challenges, greater adherence to plan. |
| Interactive Educational Resources | Providing access to educational materials, interactive videos, and online articles on healthy eating, exercise, and behavior modification. | Increased knowledge and understanding, better empowerment and self-efficacy, improved motivation, higher adherence to plan. |
| Motivational Interviewing Techniques | Using open-ended questions, reflective listening, and affirmation techniques in virtual consultations to empower patients to make their own decisions. | Increased patient autonomy and motivation, improved self-efficacy, higher likelihood of sustained engagement and adherence. |
Illustrative Case Studies (Illustrative examples)
Telemedicine offers a powerful tool for obesity management, making it more accessible and convenient for patients. This section presents hypothetical case studies demonstrating how telemedicine can effectively address the unique needs of obese individuals, improve their engagement in treatment, and ultimately achieve positive weight loss outcomes. These examples highlight the potential of telemedicine to bridge the gap in healthcare access and support for this often underserved population.
Hypothetical Patient Journey
A 45-year-old woman, Sarah, struggles with obesity and has difficulty accessing traditional healthcare due to geographical limitations and scheduling conflicts. She is initially hesitant about telemedicine, but after researching and hearing positive testimonials, she decides to try it. Sarah schedules an initial consultation with a registered dietitian and a certified personal trainer via video conferencing. During the session, Sarah discusses her weight loss goals, dietary habits, and current exercise routine.
The professionals provide personalized recommendations, creating a tailored plan incorporating a balanced diet and gradual increase in physical activity. The dietitian provides meal planning resources and nutritional guidance through a secure online platform. The trainer develops a personalized exercise program that Sarah can access through a dedicated mobile app, which includes progress tracking and motivational tools.
Telemedicine Tools and Techniques
Telemedicine employs various tools to facilitate obesity management. Video conferencing enables real-time consultations with healthcare professionals, allowing for personalized guidance and support. Mobile applications provide convenient access to exercise routines, dietary plans, and progress tracking tools. Secure online platforms facilitate secure data sharing, medication management, and communication between patients and healthcare providers. This holistic approach ensures that patients receive comprehensive care tailored to their individual needs.
Success Factors for Telemedicine Implementation
Several key factors contribute to the success of telemedicine in obesity management. Firstly, patient engagement is crucial. Clear communication, personalized plans, and consistent support from healthcare professionals are essential for maintaining motivation and adherence to treatment. Secondly, reliable internet access and suitable devices are necessary for seamless communication and access to resources. Finally, strong collaboration between healthcare providers, including dietitians, trainers, and physicians, is critical for comprehensive care and positive outcomes.
Challenges and Overcoming Them
A common challenge for patients like Sarah is the initial apprehension about telemedicine. The lack of face-to-face interaction can be a concern. However, telemedicine platforms can effectively address this by incorporating video conferencing for consultations, fostering a sense of connection and trust. Another challenge is ensuring patient access to reliable technology and internet connectivity. Telemedicine providers can mitigate this by offering resources and support to help patients overcome these barriers.
Case Study: Effectiveness of Telemedicine for Weight Loss
A study conducted by [insert reputable source, e.g., a medical journal] examined the effectiveness of a telemedicine-based weight loss program. The program included online consultations, personalized meal plans, and exercise routines delivered via a mobile app. The results indicated significant weight loss among participants compared to a control group receiving traditional in-person care. The study highlights the potential of telemedicine to enhance weight loss outcomes and improve patient adherence to treatment.
Telemedicine is revolutionizing healthcare access for folks with obesity, making appointments and follow-ups much easier. It’s great for those who struggle with mobility or live in remote areas. Looking for some cool health-related gifts for the fitness fanatics in your life? Check out some amazing ideas in our gift guides health nut to inspire your search.
Ultimately, telemedicine’s convenience makes it a game-changer for better health outcomes for those living with obesity.
Patient Outcomes Table
| Patient Profile | Telemedicine Approach | Treatment Outcomes |
|---|---|---|
| Sarah, 45-year-old woman, limited access to traditional healthcare | Online consultations with dietitian and trainer, personalized meal plans, mobile app for exercise routines | Significant weight loss, improved dietary habits, increased physical activity, improved overall well-being |
| John, 32-year-old man, busy work schedule | Scheduled video consultations with physician and nutritionist, accessible online resources | Reduced blood pressure, improved cholesterol levels, consistent weight management |
Future Trends and Innovations in Telemedicine for Obesity Management
Telemedicine is rapidly evolving, and its applications in obesity management are poised for significant advancements. This dynamic field is embracing innovative technologies to improve accessibility, personalize care, and ultimately, enhance patient outcomes. The future of telemedicine for obesity management promises more effective and convenient care for individuals struggling with this complex condition.
Emerging Technologies and Trends
Telemedicine for obesity management is benefiting from the integration of several cutting-edge technologies. These advancements are not just theoretical; they’re already demonstrating practical applications in various healthcare settings. Remote monitoring technologies, AI-powered tools, and virtual and augmented reality experiences are just a few examples of the innovations that are changing the landscape of obesity care. These technologies have the potential to make a significant impact on the lives of individuals seeking to manage their weight.
Potential of AI and Machine Learning
Artificial intelligence (AI) and machine learning (ML) are poised to revolutionize telemedicine for obesity management. AI algorithms can analyze vast amounts of patient data, including medical history, lifestyle factors, and biometric readings, to create personalized treatment plans. This level of personalization goes beyond generic recommendations and tailors interventions to each individual’s unique needs and circumstances. For instance, AI can predict potential weight loss outcomes based on individual factors, allowing for proactive interventions and adjustments to treatment plans.
Virtual and Augmented Reality Applications
Virtual reality (VR) and augmented reality (AR) offer immersive and engaging experiences for weight management. VR can simulate real-world environments, allowing patients to practice healthy habits in a safe and controlled digital space. For example, a VR experience could simulate grocery shopping, allowing patients to visualize healthier food choices and practice portion control. AR can overlay health information onto the real world, providing real-time feedback and support during physical activities or dietary choices.
This augmented reality experience could help patients track their progress and stay motivated.
Remote Surgery and Procedures for Weight Management
Remote surgical procedures, while not yet commonplace for weight management, show promising potential. Minimally invasive procedures, like those used for bariatric surgery, could potentially be performed remotely. This technology holds the possibility of making complex surgical interventions more accessible in rural or underserved areas, thus expanding access to these life-changing treatments. While still in the early stages, research into remote surgical tools and techniques for weight management continues to advance.
Integration of Wearable Technology and Remote Monitoring
Wearable technology and remote monitoring play a critical role in obesity management. Smartwatches, fitness trackers, and other wearable devices provide continuous data on physical activity, sleep patterns, and other relevant metrics. This data can be remotely transmitted to healthcare providers, enabling proactive monitoring and personalized feedback. The continuous stream of data enables healthcare professionals to adjust treatment plans in real time, facilitating better outcomes and adherence to the treatment regimen.
Potential Future Trends
- Personalized nutrition plans: AI-powered tools will analyze individual genetic predispositions, dietary preferences, and lifestyle factors to create customized meal plans. This level of personalization ensures that dietary recommendations are highly relevant to each individual’s needs, thereby maximizing adherence and effectiveness.
- Predictive modeling: AI algorithms will predict potential weight loss outcomes based on individual factors, enabling proactive interventions and adjustments to treatment plans. This proactive approach can prevent potential setbacks and ensure that patients stay on track towards their goals.
- Remote patient support communities: Virtual platforms will connect patients with support groups and mentors to foster a sense of community and provide ongoing encouragement. This social support network can prove instrumental in maintaining motivation and adherence to treatment plans.
- Gamification: Interactive games and virtual challenges will incentivize healthy behaviors and make weight management more enjoyable. Gamified approaches will provide a motivating and engaging way for patients to stay committed to their weight management goals.
- Tele-endocrinology: Telemedicine will play a larger role in diabetes management, which is often intertwined with obesity. This will enable remote monitoring of blood sugar levels and provide personalized diabetes care.
Last Word
In conclusion, telemedicine presents a powerful solution for improving access to and engagement with obesity care. By overcoming geographical barriers, reducing wait times, and personalizing treatment, telemedicine is poised to transform how we approach obesity management. The future of obesity care is undoubtedly intertwined with the continued development and implementation of innovative telemedicine solutions.