Infections vaccinations hepatitis a are crucial for public health, safeguarding individuals and communities from this viral infection. Hepatitis A, a contagious liver disease, poses significant risks, particularly in vulnerable populations. Understanding transmission routes, vaccination strategies, and safety precautions is essential for effective prevention and control. This guide explores the complexities of hepatitis A infections and vaccinations, offering a comprehensive overview of the subject.
The guide covers the importance of vaccination in preventing hepatitis A, detailing various vaccine types, efficacy, and recommended schedules for different age groups. It also delves into the routes of transmission, comparing risks across populations and highlighting high-risk groups. Effective strategies for vaccination campaigns, the role of public health initiatives, and successful vaccination program examples are also examined.
Introduction to Hepatitis A Infections and Vaccinations: Infections Vaccinations Hepatitis A
Hepatitis A is a viral infection that primarily affects the liver. Understanding its transmission, symptoms, and preventive measures is crucial for maintaining public health. Vaccination plays a pivotal role in preventing the spread of this disease, safeguarding individuals and communities from its potential complications. This discussion delves into the specifics of Hepatitis A, focusing on its nature, transmission, and the vital role of vaccination in mitigating its impact.Hepatitis A is spread primarily through the fecal-oral route, meaning it often occurs when contaminated food or water is ingested.
Protecting kids from infections like Hepatitis A is crucial, and vaccinations play a vital role. Thinking about the challenges adoptive parents face, especially regarding health histories and potential vulnerabilities, is incredibly insightful. For example, understanding the complexities of 11 things adoptive parents understand helps one appreciate the importance of thorough medical evaluations and proactive vaccination strategies for these vulnerable children.
Ultimately, preventing infections like Hepatitis A remains a top priority for ensuring healthy futures.
This can happen through close contact with an infected person or contaminated surfaces. Symptoms can vary but commonly include fatigue, nausea, abdominal pain, jaundice (yellowing of the skin and eyes), and dark urine. While many recover without lasting effects, some individuals may experience more severe complications.
Hepatitis A Transmission and Symptoms
Hepatitis A is transmitted primarily through the fecal-oral route, often linked to contaminated food or water. Ingestion of the virus is the key mode of transmission. Direct contact with an infected person or contaminated objects can also contribute to the spread. Symptoms, though variable, frequently manifest as fatigue, nausea, abdominal discomfort, jaundice, and dark urine. The incubation period, the time between infection and the appearance of symptoms, can range from 15 to 50 days.
While most individuals recover fully, severe cases can occur, highlighting the importance of prevention.
Importance of Vaccination
Vaccination is a highly effective preventative measure against Hepatitis A. It significantly reduces the risk of contracting the infection, minimizing the potential for severe complications. The vaccine creates an immune response, preparing the body to fight off the virus should exposure occur. This protection is critical for safeguarding both individual health and public health.
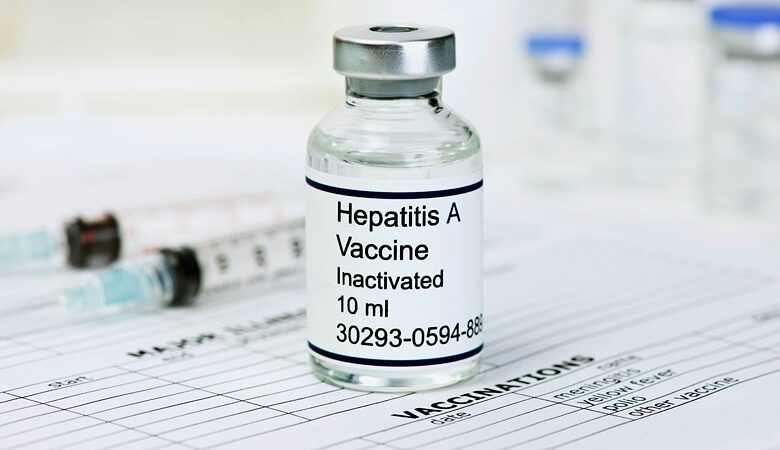
Types of Hepatitis A Vaccines and Efficacy
Several types of Hepatitis A vaccines are available, each with a proven track record of efficacy. These vaccines typically provide long-lasting protection against the infection. The inactivated virus vaccine is one commonly used type, known for its safety and high efficacy. Other forms of vaccine technology are under continuous development, often enhancing their convenience and efficacy. Clinical trials and extensive studies consistently demonstrate the vaccine’s ability to prevent Hepatitis A infection.
Recommended Vaccination Schedules
Vaccination schedules vary depending on age. Infants and children typically receive multiple doses according to the recommended immunization schedule. Adolescents and adults often receive a two-dose series, tailored for optimal protection. The precise timing and dosage are designed to establish a robust immune response. Specific schedules are often recommended by health authorities and medical professionals, ensuring the most effective protection for different age groups.
Understanding Hepatitis A Transmission
Hepatitis A, a viral liver infection, is largely preventable. Understanding how it spreads is crucial for implementing effective preventative measures. This knowledge empowers individuals to make informed choices and communities to take proactive steps towards controlling outbreaks.Hepatitis A is primarily transmitted through the fecal-oral route, meaning contaminated food or water is the most common source. This can occur when a person with the virus does not practice proper hygiene or when contaminated food or water is consumed.
The virus replicates in the intestines and then spreads through the bloodstream to the liver. This is why sanitation and hygiene play a critical role in reducing the risk of transmission.
Transmission Routes
Different routes of exposure can lead to Hepatitis A infection. Contaminated food and water are significant vectors, particularly in areas with inadequate sanitation. Food handlers who are infected can unknowingly contaminate food, spreading the virus. Also, contact with infected individuals, particularly those who are not practicing proper hygiene, can result in transmission.
- Contaminated food and water: This is a major transmission route, especially in settings with poor sanitation. Raw shellfish, contaminated salads, and improperly prepared foods can be vectors if handled by an infected person. Water sources contaminated with fecal matter can also pose a risk.
- Direct contact: Close contact with an infected person, including direct contact with their bodily fluids, can lead to transmission. This is particularly important in households or close communities where personal hygiene may be compromised. For example, sharing utensils or food can be risky if not properly cleaned.
Risk Comparison Across Populations
Risk factors for Hepatitis A vary significantly depending on factors like socioeconomic status, access to clean water and sanitation, and geographic location.
- Travel to high-risk areas: Individuals traveling to countries with poor sanitation or limited access to clean water are at higher risk. For instance, areas with limited access to safe drinking water, poor sewage systems, or inadequate handwashing facilities. Examples include regions in some parts of developing nations.
- Exposure to contaminated food: Food preparation practices in certain regions, like improper food handling, may increase exposure. This is more likely in communities with limited access to refrigeration or those with poor food safety regulations.
- Close contact with infected individuals: Individuals living in crowded environments or those with close contact with someone known to be infected are more vulnerable to transmission. This includes situations like sharing living spaces, personal items, or close family members.
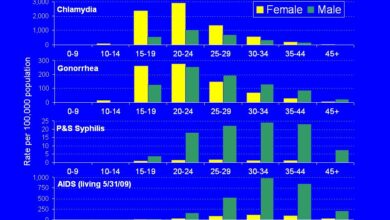
High-Risk Groups
Certain populations are more susceptible to Hepatitis A infection due to various factors.
- Individuals with poor sanitation: Communities lacking access to clean water and adequate sanitation systems are highly vulnerable. This lack of hygiene increases the chance of ingesting contaminated food or water. For instance, communities with limited or no access to clean water or sewage systems.
- Individuals with compromised immune systems: People with weakened immune systems, such as those with HIV/AIDS or other conditions, are more likely to develop severe Hepatitis A. This is because their immune systems cannot effectively fight the infection. A weakened immune system may struggle to mount an adequate defense against the virus.
- Individuals working in food service: Food handlers are at a higher risk due to their potential exposure to contaminated food. This is because of the direct contact with food and the possibility of not following proper hygiene protocols. For instance, a restaurant worker who does not wash their hands after using the restroom.
Hygiene and Sanitation in Prevention
Proper hygiene and sanitation practices are essential in preventing Hepatitis A transmission. By implementing these practices, communities can significantly reduce the risk of outbreaks.
- Handwashing: Regular handwashing with soap and water, especially after using the restroom, handling food, or coming into contact with potential contaminants, is crucial. This simple act can significantly reduce the spread of the virus. For instance, washing hands thoroughly after handling raw meat.
- Safe food handling: Proper food preparation and handling practices, such as avoiding cross-contamination, using proper cooking temperatures, and storing food safely, are important to prevent contamination. This includes ensuring that raw and cooked foods are separated to avoid contamination.
- Safe water sources: Ensuring access to safe drinking water and sanitation facilities is crucial. This includes having access to potable water and proper sewage disposal.
Vaccination Strategies for Hepatitis A
Protecting vulnerable populations from Hepatitis A is crucial for public health. Effective vaccination strategies are vital to controlling the spread of this viral infection and minimizing its impact on individuals and communities. These strategies require a multifaceted approach, focusing on targeted campaigns, community engagement, and sustained public health initiatives.Targeted vaccination campaigns are essential to reach those most at risk, ensuring equitable access to preventative measures.
Vaccination programs must also account for potential barriers and work towards overcoming these hurdles, maximizing their effectiveness.
Vulnerable Population Targeting
Vaccination campaigns should prioritize vulnerable populations to maximize their impact. This includes individuals with compromised immune systems, those living in overcrowded conditions, and people in regions with a high prevalence of Hepatitis A. For instance, homeless shelters, migrant worker camps, and areas with poor sanitation infrastructure should be considered priority locations for outreach. Furthermore, ensuring vaccine accessibility in underserved communities is crucial to prevent disparities in vaccination rates.
Importance of Public Health Initiatives
Public health initiatives play a critical role in promoting Hepatitis A vaccination. These initiatives include educating the public about the importance of vaccination, dispelling myths, and providing accurate information about the virus. Effective communication strategies can also address concerns about side effects and encourage vaccination uptake. Furthermore, community health workers can act as trusted sources of information and support within their communities.
Examples of Successful Vaccination Programs
Several regions have successfully implemented Hepatitis A vaccination programs. For example, programs in some developed nations have seen a significant decrease in Hepatitis A cases after the introduction of widespread vaccination campaigns. These programs often incorporate targeted outreach to specific communities and emphasize the importance of vaccination in reducing transmission rates.
Efficacy of Vaccination against Hepatitis A Strains
Hepatitis A vaccines are highly effective in preventing infection by various strains of the virus. Studies have consistently demonstrated the efficacy of different vaccine formulations in preventing illness. Vaccination strategies should consider the specific strains prevalent in the target area. This approach allows for tailoring the vaccination campaign to the most effective vaccine type for the specific community.
Hepatitis A Vaccine Safety and Side Effects
Protecting yourself against Hepatitis A is crucial, and vaccination is a safe and effective way to do so. Understanding the potential side effects of the vaccine can help you make informed decisions and manage any reactions that may occur. This section delves into the safety profile of Hepatitis A vaccines, common side effects, rare but serious adverse events, and how to report them.
We’ll also compare the safety profiles of different vaccines to give you a more complete picture.
Safety Profile of Hepatitis A Vaccines
Hepatitis A vaccines are generally considered safe and highly effective. Rigorous testing and monitoring during development ensure the vaccines are carefully evaluated for safety before they are released for public use. Extensive clinical trials involve thousands of participants, examining the vaccine’s impact on the immune system and identifying potential adverse events. The benefits of vaccination against Hepatitis A far outweigh the potential risks for most individuals.
Common Side Effects of Hepatitis A Vaccination
Mild side effects, like soreness, redness, or swelling at the injection site, are common after receiving a Hepatitis A vaccination. These reactions are typically temporary and resolve on their own within a few days. Other common side effects include fever, fatigue, headache, and muscle aches.
Management of Common Side Effects
For mild side effects, over-the-counter pain relievers like ibuprofen or acetaminophen can help manage discomfort. Rest and hydration are also important. If the symptoms are severe or persistent, consulting a healthcare provider is recommended.
Rare But Serious Side Effects
Although rare, some individuals may experience more serious side effects following Hepatitis A vaccination. These include allergic reactions, such as hives, difficulty breathing, or swelling of the face, lips, or throat. Severe allergic reactions require immediate medical attention. Other rare but serious side effects might include Guillain-Barré syndrome, a neurological disorder. These are extremely rare occurrences.
Reporting Rare Side Effects
It is crucial to report any unusual or serious side effects following vaccination to your healthcare provider or the relevant health authorities. This helps in monitoring the safety of the vaccine and identifying any potential trends or patterns. Detailed records of the symptoms and their onset are beneficial in providing accurate reporting. Reporting systems are in place to ensure the collection and analysis of such information.
Comparison of Different Hepatitis A Vaccine Safety Profiles
Different Hepatitis A vaccines have comparable safety profiles. All licensed vaccines have undergone rigorous testing to ensure their safety and efficacy. While the exact frequency of side effects may vary slightly between different formulations, the overall safety profile is consistent across available vaccines. Factors like individual sensitivities and pre-existing conditions can influence the experience of side effects.
Important Note on Vaccine Safety Data
Vaccine safety data is continuously monitored and updated by public health agencies and regulatory bodies. Information on potential side effects and their management is based on current scientific evidence and best practices. Individuals should consult their healthcare provider for personalized advice regarding vaccine safety.
Vaccination for Children and Infants
Protecting our little ones from Hepatitis A is crucial. Infants and young children are particularly vulnerable to this viral infection, which can lead to serious health complications. Vaccination offers a safe and effective way to shield them from the disease and its potential long-term consequences.Early vaccination is highly recommended for infants and young children. The immune system is still developing in this age group, and vaccination provides a strong defense against the virus.
This proactive measure can prevent severe illness and long-term health issues.
Vaccination Schedules for Infants and Young Children, Infections vaccinations hepatitis a
Vaccination schedules for Hepatitis A vary slightly depending on the specific vaccine used and the recommendations of the Centers for Disease Control and Prevention (CDC) and other health organizations. These schedules are designed to provide optimal protection at the most appropriate time for a child’s developing immune system.
- A typical schedule often involves two doses of the Hepatitis A vaccine, given several months apart. The exact timing is determined by the specific vaccine used and the guidelines of the administering healthcare provider.
Potential Benefits of Vaccination
Vaccination significantly reduces the risk of Hepatitis A infection in children. This protection translates to a lower likelihood of developing the potentially severe complications associated with the disease. The benefits extend beyond the individual child, contributing to community health by limiting the spread of the virus.
Potential Risks of Vaccination
Like any medical intervention, Hepatitis A vaccination carries potential risks. However, these risks are generally mild and short-lived. Common side effects include soreness, redness, or swelling at the injection site. In rare cases, more serious side effects may occur, but these are uncommon. Parents should always discuss any concerns with their pediatrician before making vaccination decisions.
Parental Consent and Education
Parental consent is essential for vaccinating infants and young children. Healthcare providers must thoroughly educate parents about the benefits, risks, and schedule of Hepatitis A vaccination. Open communication and clear explanations empower parents to make informed decisions about their child’s health. Parents should feel comfortable asking questions and expressing concerns to their healthcare provider. This ensures a trusting relationship and a well-informed vaccination decision.
Hepatitis A Vaccination for Travelers
Traveling opens up a world of possibilities, but it’s also important to be prepared for potential health risks. Understanding the importance of Hepatitis A vaccination for travelers to high-risk areas is crucial for a safe and enjoyable trip. This article delves into the recommendations, timelines, and factors to consider when making vaccination decisions.Traveling to regions with poor sanitation and hygiene practices can increase the risk of contracting Hepatitis A.
This virus, while often mild, can lead to significant discomfort and complications. Protecting yourself with a Hepatitis A vaccination is a proactive step towards ensuring a healthy journey.
Vaccination Recommendations for Travelers
Traveling to areas with a higher prevalence of Hepatitis A requires careful consideration of vaccination. Vaccination is highly recommended for all travelers to regions where the risk of Hepatitis A infection is significant. This proactive measure can significantly reduce the chances of contracting the virus during your travels.
Recommended Vaccination Timelines for Different Travel Durations
The optimal vaccination timeline depends on the duration of your trip. It’s crucial to consult with a healthcare professional to determine the appropriate vaccination schedule for your specific travel plans.
| Travel Duration | Recommended Vaccination Timeline |
|---|---|
| Less than 4 weeks | A single dose is usually sufficient. |
| 4-6 weeks | A single dose is recommended, but some individuals may benefit from a second dose, depending on the specific vaccine and individual health status. |
| More than 6 weeks | A two-dose series, administered several weeks apart, is typically recommended for optimal protection. |
The table above provides a general guideline. It’s essential to consult with a healthcare provider for personalized recommendations, taking into account individual factors like age, health status, and specific travel itinerary.
Factors Influencing the Need for Hepatitis A Vaccination in Travelers
Several factors influence the necessity of Hepatitis A vaccination for travelers. The level of sanitation in the destination, the traveler’s personal health history, and the duration of the trip all play a role in determining the risk assessment. A thorough evaluation of these factors is crucial for making informed decisions.
- Destination Sanitation: Areas with poor sanitation and hygiene practices pose a higher risk of Hepatitis A transmission. Travelers visiting these regions are at a greater risk and should strongly consider vaccination.
- Pre-existing Health Conditions: Individuals with compromised immune systems or pre-existing liver conditions may be at a higher risk of complications from Hepatitis A. Pre-travel consultation with a doctor is crucial to assess individual risk factors.
- Duration of Stay: The length of the trip significantly influences the likelihood of exposure. Extended stays in high-risk areas necessitate a more thorough evaluation of vaccination needs.
Importance of Pre-Travel Consultations for Vaccination Decisions
Pre-travel consultations with a healthcare provider are essential for optimal vaccination decisions. A healthcare professional can assess individual risk factors, recommend the appropriate vaccination schedule, and address any concerns. This personalized approach ensures travelers receive the best possible guidance for their specific circumstances.
A pre-travel consultation with a doctor allows for a personalized risk assessment and ensures that the traveler receives the most appropriate advice and guidance.
Vaccination in conjunction with other diseases
Coordinating hepatitis A vaccination with other immunizations is crucial for maximizing overall protection and minimizing potential health risks. Proper scheduling ensures optimal immune response and prevents unnecessary delays in achieving full immunity. This approach is especially important for children and infants who may be receiving multiple vaccines at the same time.
Thinking about infections like hepatitis A, and the crucial role of vaccinations in preventing them, got me wondering about the bigger picture. Recent news about the possibility of the US losing its measles elimination status next month will the us lose its measles elimination status next month really highlights the importance of proactive public health measures, especially when it comes to preventable diseases.
Ultimately, staying informed and up-to-date on vaccinations is key to maintaining our health and well-being.
Optimal Timing of Hepatitis A Vaccination
The optimal timing of hepatitis A vaccination in relation to other vaccinations is based on several factors, including the child’s age, the specific vaccines being administered, and the recommended intervals between doses. Different vaccine schedules may exist for various countries and health organizations, highlighting the importance of consulting local guidelines and recommendations. It is essential to adhere to these schedules to ensure effective immune response and protection against the disease.
Possible Combinations and Recommended Intervals
Vaccination schedules often allow for simultaneous administration of multiple vaccines, provided the recommended intervals are respected. This approach simplifies the immunization process for both healthcare providers and patients. Co-administration of vaccines is generally safe and effective when appropriate intervals are observed.
| Vaccine | Hepatitis A Vaccine | Recommended Interval |
|---|---|---|
| Diphtheria, Tetanus, Pertussis (DTaP) | Administer simultaneously | Recommended, but intervals may vary based on specific schedule |
| Measles, Mumps, Rubella (MMR) | Administer simultaneously | Recommended, but intervals may vary based on specific schedule |
| Varicella (Chickenpox) | Administer simultaneously | Recommended, but intervals may vary based on specific schedule |
| Inactivated Poliovirus Vaccine (IPV) | Administer simultaneously | Recommended, but intervals may vary based on specific schedule |
| Haemophilus influenzae type b (Hib) | Administer simultaneously | Recommended, but intervals may vary based on specific schedule |
Note: This table provides general guidelines. Always consult the specific vaccination schedule recommended by your healthcare provider or local health authority. The recommended intervals between doses for each vaccine combination are crucial for maximizing effectiveness.
Potential Benefits and Risks of Co-administration
Co-administration of vaccines offers significant benefits, including streamlined immunization schedules and reduced patient visits. It allows for efficient use of healthcare resources and improves compliance with vaccination schedules. However, potential risks are minimal when following established protocols and recommended intervals. Proper training and adherence to protocols by healthcare providers are essential to minimize any potential risks.
“Co-administration of vaccines is generally safe and effective when appropriate intervals are observed.”
Recommended Protocols for Vaccine Administration
Recommended protocols for vaccine administration when combined with other vaccines are established to ensure proper injection technique and avoid potential complications. Adherence to these protocols is essential for optimal efficacy and safety. Each vaccine has specific requirements regarding injection site and needle gauge, which must be carefully followed. Consult local health authorities and healthcare providers for detailed protocols.
Post-Vaccination Considerations
Taking the necessary steps after receiving a hepatitis A vaccination is crucial for ensuring its effectiveness and minimizing any potential complications. Post-vaccination care goes beyond simply receiving the shot; it encompasses monitoring for side effects, understanding follow-up procedures, and acknowledging the importance of post-vaccination support. This comprehensive approach helps individuals achieve optimal health outcomes following the vaccination.
Monitoring for Side Effects
Post-vaccination monitoring is essential to identify and manage any potential side effects promptly. Mild reactions, such as soreness at the injection site, are common and typically resolve within a few days. However, severe or persistent reactions warrant immediate medical attention. This proactive approach ensures that any concerning symptoms are addressed swiftly, preventing potential complications.
Recommended Follow-Up Procedures
Following up with your healthcare provider after vaccination is important for evaluating the effectiveness of the vaccine and addressing any concerns. Your healthcare provider will assess your response to the vaccination and provide guidance on any necessary follow-up measures. The recommended follow-up timeframe may vary depending on the individual’s specific circumstances.
Importance of Post-Vaccination Care and Support
Post-vaccination care extends beyond just medical monitoring. It includes providing emotional support and practical guidance to address any anxieties or concerns related to the vaccination process. This holistic approach helps ensure a positive experience and promotes adherence to the recommended vaccination schedule.
Possible Post-Vaccination Complications and Management
| Possible Complication | Description | Management ||—|—|—|| Localized Reaction (e.g., pain, redness, swelling at injection site) | Common, usually mild and resolves within a few days. | Apply a cold compress to the injection site. Over-the-counter pain relievers (e.g., ibuprofen) may help. || Fever | A temperature of 100.4°F (38°C) or higher. | Monitor fever closely.
Rest, hydration, and over-the-counter fever reducers (e.g., acetaminophen) can help. Seek medical attention if fever persists or worsens. || Allergic Reaction | Symptoms can range from mild (hives, itching) to severe (difficulty breathing, swelling of the face or throat). | Seek immediate medical attention. Severe allergic reactions require emergency medical treatment.
|| Severe Pain | Persistent or intense pain at the injection site. | Consult your healthcare provider for appropriate pain management strategies. || Anaphylaxis | A life-threatening allergic reaction. Characterized by rapid onset and potentially severe symptoms. | Immediate medical intervention is critical.
Individuals with a history of severe allergies should be aware of the signs and symptoms of anaphylaxis. |
Prevention Strategies Beyond Vaccination
While vaccination is a cornerstone of Hepatitis A prevention, other crucial measures significantly reduce the risk of infection. Understanding and implementing these strategies, in addition to vaccination, creates a comprehensive approach to safeguarding individuals and communities from Hepatitis A.Implementing preventive measures beyond vaccination enhances the effectiveness of vaccination programs and minimizes the overall risk of Hepatitis A transmission. These strategies encompass personal hygiene, public health interventions, and responsible food handling practices.
Combining vaccination with these preventative measures creates a powerful defense against the virus.
Personal Hygiene Practices for Prevention
Maintaining meticulous personal hygiene plays a pivotal role in preventing Hepatitis A transmission. This involves consistent handwashing, particularly after using the restroom, preparing food, or touching potentially contaminated surfaces. Frequent and thorough handwashing significantly reduces the risk of infection.
- Handwashing Technique: Thoroughly wash hands with soap and water for at least 20 seconds, ensuring all surfaces, including between fingers and under nails, are cleansed. Alcohol-based hand sanitizers are effective alternatives when soap and water are unavailable.
- Hygiene Practices: Avoiding contact with contaminated food, water, and surfaces is crucial. Avoiding sharing personal items like utensils, towels, and drinking glasses is essential.
Public Health Measures for Infection Control
Public health measures are vital in controlling the spread of Hepatitis A within communities. These measures aim to ensure safe water supplies, proper sanitation, and effective waste disposal systems.
Thinking about infections like Hepatitis A and the importance of vaccinations got me pondering. It’s fascinating how our brains react to new information. Recent research, for example, shows that our brains physically change when we alter our opinions, research shows what happens in our brains when we change our minds. This highlights how crucial vaccination programs are; they literally help us, as a society, to adjust our collective understanding of and response to infections like Hepatitis A.
- Safe Water Supplies: Ensuring access to safe and clean drinking water is a cornerstone of public health. This involves treating water sources to eliminate contamination.
- Sanitation and Waste Disposal: Implementing effective sanitation and waste disposal systems prevents contamination of water sources and food. This includes proper sewage treatment and the segregation of human waste.
- Food Safety Regulations: Stringent regulations concerning food preparation and handling are essential to prevent contamination. These regulations cover all aspects of the food supply chain.
Safe Food Handling Practices
Safe food handling practices are crucial to prevent Hepatitis A transmission. These practices encompass all stages, from procuring food to preparing and serving it.
- Food Source Verification: Ensure that food is procured from reputable sources and that it has been handled safely throughout its journey. Careful inspection of food items for any signs of contamination is essential.
- Proper Food Storage: Storing food at appropriate temperatures and avoiding cross-contamination during preparation and serving are crucial. The correct temperature range for food storage prevents bacterial growth, which can further contribute to contamination.
- Avoiding Contaminated Food: Avoid consuming food from sources that may have been contaminated, such as street vendors in areas with poor sanitation.
Historical Context of Hepatitis A and Vaccination
Tracing the history of Hepatitis A reveals a fascinating journey from recognizing the disease to developing effective preventative measures. Early understanding of this viral infection was hampered by limited diagnostic tools and a lack of comprehensive epidemiological data. This historical context underscores the significant advancements in public health and medical science that have led to the widespread availability and efficacy of Hepatitis A vaccines.
Early Recognition and Outbreaks
Understanding the historical context of Hepatitis A requires recognizing that early recognition was often indirect. Symptoms, which could range from mild to severe, were sometimes confused with other illnesses. Epidemiological studies, particularly those linking outbreaks to contaminated water or food, gradually provided a clearer picture of the disease’s transmission. These outbreaks, sometimes impacting entire communities, served as crucial triggers for public health interventions.
For instance, historical records often highlight instances where water contamination led to large-scale Hepatitis A outbreaks in densely populated areas.
Development of Hepatitis A Vaccines
Significant progress in understanding the Hepatitis A virus paved the way for vaccine development. Scientists, through meticulous research, identified key viral components and eventually developed methods for producing safe and effective vaccines. This process wasn’t instantaneous; it involved rigorous testing and refinement, with early prototypes undergoing numerous trials before reaching the standards required for widespread use.
Evolution of Vaccination Strategies
The evolution of vaccination strategies for Hepatitis A reflects the continuous refinement of public health approaches. Initial vaccination programs focused on high-risk groups, such as travelers or individuals in specific geographic areas with a history of outbreaks. Over time, strategies broadened to encompass broader population groups, often in conjunction with other vaccination programs. These evolving strategies are directly influenced by epidemiological data, understanding of transmission routes, and the availability of improved vaccine formulations.
For example, the inclusion of Hepatitis A vaccination in routine childhood immunization schedules demonstrates a shift towards broader population protection.
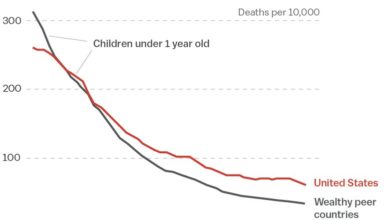
Impact of Vaccination Programs on Global Hepatitis A Rates
Vaccination programs have had a substantial impact on reducing global Hepatitis A rates. Areas with robust vaccination programs have seen significant declines in the incidence of Hepatitis A infections. The availability and use of vaccines have demonstrably contributed to reduced morbidity and mortality associated with the disease. Countries with comprehensive vaccination programs often report significantly lower rates of Hepatitis A compared to those without.
For example, data from various global health organizations consistently show a strong correlation between vaccination rates and a decrease in Hepatitis A infections.
Last Recap
In conclusion, infections vaccinations hepatitis a are a critical public health concern. Comprehensive vaccination strategies, coupled with preventative measures beyond vaccination, are essential for controlling hepatitis A. Understanding the historical context, safety profiles, and specific considerations for various populations, such as children, travelers, and those with co-existing conditions, allows for personalized and effective interventions. This guide provides a thorough understanding of the multifaceted nature of hepatitis A and vaccination, equipping readers with the knowledge to make informed decisions about their health and the health of those around them.