Is depression remission possible? This question resonates deeply with countless individuals grappling with this challenging mental health condition. It’s a journey of understanding, resilience, and hope, where remission isn’t just about the absence of symptoms, but a shift in perspective and a newfound ability to navigate life’s complexities.
This exploration delves into the intricacies of depression remission, examining the various factors influencing its attainment, effective treatment approaches, and strategies for maintaining a state of improved well-being. We’ll unpack the nuances of remission, differentiating it from recovery, and explore the crucial role of self-care, support systems, and proactive steps in achieving lasting positive change.
Understanding Depression Remission

Depression remission is a crucial concept in mental health, representing a significant step towards improved well-being for individuals struggling with depressive disorders. It’s important to distinguish remission from recovery, as they differ in the extent and duration of symptom reduction. This understanding provides a clearer picture of the journey towards mental wellness and helps in developing appropriate treatment strategies.Remission in depression signifies a substantial reduction or absence of depressive symptoms.
While the possibility of depression remission is often debated, recent research suggests it’s more achievable than previously thought. Interestingly, a new study on the potential heart safety of Celebrex ( celebrex safer for heart than thought ) highlights the importance of ongoing research in understanding the complexities of chronic conditions like depression and the medications that may impact them.
Ultimately, individual responses to treatment vary, and more research is crucial to better understand depression remission potential.
It’s a temporary state, and while it can be incredibly positive, it’s not equivalent to complete recovery. Individuals in remission may experience significant improvement in their daily functioning, but the potential for relapse remains. This dynamic nature underscores the importance of ongoing support and management strategies.
Definition and Distinctions, Is depression remission possible
Remission in depression is defined as a sustained period of improvement characterized by a notable decrease or absence of depressive symptoms. This contrasts with recovery, which signifies the complete absence of symptoms and a return to pre-illness functioning over a prolonged period. Importantly, remission is not a cure; it’s a stage in the recovery process.
Stages of Depression and Remission
Depression often involves various stages, each characterized by different symptom intensities. Remission typically occurs within these stages, signifying a period of reduced symptom severity. For example, an individual experiencing moderate depression might enter remission after successfully completing therapy and medication, showcasing a decrease in the intensity of symptoms. Further, remission can be a stepping stone towards recovery, as the individual gradually improves and maintains their mental health.
Criteria for Diagnosing and Assessing Remission
Clinicians utilize specific criteria to diagnose and assess remission in depression. These criteria typically involve standardized assessments of symptoms, such as the Hamilton Depression Rating Scale (HDRS) or the Beck Depression Inventory (BDI). The scores obtained from these assessments provide quantitative data on the severity of symptoms. The decrease in symptom severity over time, measured against these scales, is a key indicator of remission.
Individual Perspectives on Remission
The meaning of remission varies significantly for individuals experiencing depression. Some may view it as a chance to reclaim their lives and engage in activities they had previously enjoyed. Others might see it as a temporary respite, acknowledging the potential for relapse. These diverse perspectives underscore the importance of individualized support and understanding.
Remission vs. Recovery
| Characteristic | Remission | Recovery |
|---|---|---|
| Severity of Symptoms | Reduced or absent symptoms | Complete absence of symptoms |
| Duration | Sustained period of improvement | Long-term absence of symptoms |
| Functional Impact | Improved ability to function | Full restoration of function |
This table highlights the key distinctions between remission and recovery, emphasizing the crucial role of sustained improvement and complete symptom resolution in recovery. It’s important to note that remission can be a significant achievement in the journey toward recovery.
Factors Influencing Remission: Is Depression Remission Possible
Depression remission, a period of significant improvement or absence of depressive symptoms, is not a singular event but a complex interplay of various factors. Understanding these factors is crucial for developing effective strategies to support individuals in achieving and maintaining remission. It’s important to recognize that remission is a personalized journey, and what works for one person may not work for another.Achieving and maintaining remission from depression involves a multifaceted approach that considers biological predispositions, psychological resilience, environmental circumstances, and social support networks.
These interconnected factors influence an individual’s vulnerability to relapse and their ability to sustain remission. A holistic understanding of these influences is essential for developing personalized treatment plans that promote long-term well-being.
Biological Factors
Biological factors play a significant role in susceptibility to depression and the potential for remission. Genetic predispositions can increase an individual’s risk for developing depression, and certain neurobiological imbalances can contribute to the severity and duration of depressive symptoms. Variations in brain structure and function, neurotransmitter levels, and hormonal fluctuations are all implicated in the complex interplay of biological factors affecting remission.
Individuals with a family history of depression or specific genetic markers might experience varying responses to treatment, impacting the likelihood of remission. For example, studies suggest that individuals with certain genetic variations may respond better to specific antidepressant medications, while others may benefit more from combined therapies.
Psychological Factors
Psychological factors are central to achieving and maintaining remission. Cognitive-behavioral therapy (CBT) is a cornerstone of psychological treatment, helping individuals identify and challenge negative thought patterns that contribute to depressive symptoms. Building coping mechanisms, stress management techniques, and fostering emotional regulation skills all contribute to a more resilient mindset, increasing the likelihood of remission. For instance, a patient who learns to identify and reframe negative thoughts about their self-worth is more likely to experience sustained remission.
Environmental Factors
Environmental factors encompass the external influences that impact an individual’s well-being. Stressful life events, such as job loss, relationship difficulties, or financial hardship, can trigger or exacerbate depressive symptoms. Conversely, supportive and nurturing environments can contribute to remission. Access to resources like healthy food, safe housing, and supportive communities can buffer the impact of stress and promote overall well-being.
For instance, individuals living in areas with high rates of crime or poverty might face increased challenges in achieving remission compared to those in more stable environments.
Wondering if depression remission is possible? It’s definitely a journey, and while the path isn’t always clear, taking care of your physical health can play a big role. For example, managing diabetes during the holidays can be tricky, but the hangry woman’s tips for staying healthy with diabetes during the holidays offers some helpful strategies.
Ultimately, focusing on holistic well-being, including physical and mental health, is key to potentially finding remission.
Social Support
Social support plays a crucial role in facilitating remission from depression. Strong social connections, including family, friends, and support groups, can provide emotional comfort, practical assistance, and a sense of belonging. These connections offer a buffer against stress and provide a vital network of encouragement and understanding. A strong support system can help individuals navigate challenging situations, maintain motivation for treatment, and cope with potential setbacks.
For example, a person experiencing a difficult time might find solace and encouragement in their social network, which helps maintain engagement with their treatment plan and contributes to remission.
Treatment Approaches
Different treatment approaches have varying impacts on remission rates. Evidence-based treatments like psychotherapy, medication, and lifestyle interventions all contribute to a holistic approach. The combination of medication and therapy has shown promising results in increasing remission rates. For example, a patient undergoing CBT alongside medication may experience faster and more sustained remission compared to individuals utilizing only one approach.
Relationship Between Factors and Remission Potential
| Factor | Description | Impact on Remission |
|---|---|---|
| Biological | Genetic predispositions, neurobiological imbalances, hormonal fluctuations | Can influence individual responses to treatment and risk of relapse |
| Psychological | Cognitive-behavioral therapy (CBT), coping mechanisms, emotional regulation | Essential for identifying and challenging negative thought patterns and building resilience |
| Environmental | Stressful life events, access to resources, community support | Can trigger or exacerbate depressive symptoms, or conversely promote well-being and support remission |
| Social Support | Family, friends, support groups | Provides emotional comfort, practical assistance, and a sense of belonging, potentially improving resilience and maintaining remission |
| Treatment Approaches | Combination of medication and therapy, lifestyle interventions | Can lead to more sustained and improved remission outcomes |
Treatment Approaches for Remission
Depression remission, a significant improvement in symptoms and a return to a fulfilling life, is achievable. A multifaceted approach, combining various treatment modalities, is often crucial for successful remission. This section explores the diverse landscape of treatments that can pave the way toward lasting recovery.Effective treatment for depression remission often involves a combination of approaches, tailoring the strategy to the individual’s specific needs and preferences.
This personalized approach acknowledges the complexity of the condition and the unique factors influencing its manifestation in each person.
Pharmacological Treatments
Medication plays a vital role in managing depressive symptoms and promoting remission. Antidepressants, a class of medications, are frequently prescribed to regulate neurochemicals in the brain, impacting mood and emotional regulation. Different types of antidepressants target specific neurotransmitter systems, each with varying side effects and efficacy profiles. Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed, often exhibiting a favorable side effect profile.
Other options, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs), might be considered in cases where SSRIs are ineffective or not well-tolerated. The decision of which medication to use, and the dosage, is made collaboratively with a healthcare professional. Monitoring side effects and adjusting the treatment plan is crucial to ensure optimal results.
Psychotherapeutic Treatments
Psychotherapy provides a structured environment for understanding and managing depressive symptoms. Various types of therapy can contribute to remission, each employing different strategies. Cognitive Behavioral Therapy (CBT) helps identify and modify negative thought patterns and behaviors that contribute to depressive symptoms. Dialectical Behavior Therapy (DBT) focuses on emotional regulation and distress tolerance skills, crucial for managing emotional fluctuations.
Interpersonal Therapy (IPT) addresses interpersonal issues and relationships, which can significantly influence mental well-being. The effectiveness of psychotherapy depends on factors such as the therapist’s expertise, the patient’s willingness to engage, and the specific type of therapy chosen.
Alternative Therapies
Alternative therapies, while not always scientifically proven to treat depression, may offer complementary support. Mindfulness-based stress reduction (MBSR) techniques, incorporating meditation and mindful practices, can help manage stress and improve emotional regulation. Yoga and Tai Chi, promoting physical and mental well-being, may provide additional support for remission. Nutritional interventions, focusing on balanced diets and addressing potential deficiencies, can contribute to overall health and well-being.
While these approaches may not be a primary treatment for depression, they can be used in conjunction with other treatments to enhance the overall therapeutic experience. It is important to consult with a healthcare professional before incorporating any alternative therapies into your treatment plan.
Treatment Options Table
| Treatment Type | Description | Potential Benefits for Remission |
|---|---|---|
| Antidepressants (e.g., SSRIs, SNRIs) | Medications that affect neurotransmitter levels in the brain. | Can alleviate depressive symptoms, potentially leading to remission, but may have side effects. |
| Cognitive Behavioral Therapy (CBT) | A type of psychotherapy that helps identify and change negative thought patterns and behaviors. | Can improve mood, reduce symptoms, and promote healthy coping mechanisms. |
| Dialectical Behavior Therapy (DBT) | A type of therapy focusing on emotional regulation and distress tolerance skills. | Can enhance emotional regulation and improve overall well-being, potentially contributing to remission. |
| Interpersonal Therapy (IPT) | Therapy addressing interpersonal issues and relationships. | Can improve relationship dynamics and reduce stress, potentially leading to a reduction in depressive symptoms. |
| Mindfulness-based Stress Reduction (MBSR) | Techniques like meditation and mindfulness practices. | Can enhance stress management, emotional regulation, and well-being, potentially complementing other treatments. |
Maintaining Remission

Achieving depression remission is a significant step toward a healthier and happier life. However, the journey doesn’t end there. Maintaining this positive state requires ongoing effort and proactive strategies. This phase focuses on preventing relapse, fostering resilience, and building a strong support system. It’s about understanding that remission isn’t a destination, but a sustained path requiring consistent attention and adaptation.Maintaining remission involves a multifaceted approach that goes beyond just managing symptoms.
It’s about nurturing overall well-being and developing coping mechanisms to navigate life’s inevitable challenges. This proactive approach empowers individuals to stay in remission, allowing them to fully engage in life and thrive.
Proactive Strategies for Preventing Relapse
Sustaining remission requires a proactive and multifaceted approach that encompasses various strategies. Individuals should not wait for warning signs to appear but actively engage in measures to prevent potential relapses. This proactive approach includes developing a strong support system and engaging in consistent self-care practices. Furthermore, understanding and addressing potential triggers can significantly aid in maintaining remission.
Is depression remission possible? Absolutely. Finding healthy coping mechanisms, like incorporating regular walks into your routine, can be incredibly helpful. For example, ways to ease menopause symptoms with walking often involve strategies that also benefit mental well-being. The key is consistency and finding activities that bring you joy and a sense of accomplishment.
Ultimately, consistent self-care, like walking, can pave the way towards a more positive outlook, regardless of the challenges we face.
Importance of Ongoing Self-Care
Ongoing self-care is crucial for maintaining remission. It involves nurturing physical, mental, and emotional well-being. Consistent self-care strategies help individuals build resilience, manage stress, and maintain a healthy outlook. This includes activities like regular exercise, a balanced diet, sufficient sleep, mindfulness practices, and engaging in hobbies and activities that bring joy. A consistent self-care routine becomes a cornerstone in the ongoing management of mental health.
Role of Support Systems in Maintaining Remission
Strong support systems play a vital role in maintaining remission. These systems can provide emotional support, encouragement, and accountability. Having a network of friends, family, or support groups can offer a sense of belonging and shared experience. This can help individuals navigate challenging times and stay connected to their support network. Seeking professional guidance, if needed, can also be a valuable addition to one’s support system.
Examples of Proactive Steps
Numerous proactive steps can help maintain remission. These steps include maintaining a consistent medication schedule (if applicable), establishing healthy routines, prioritizing stress management techniques, and practicing mindfulness. Building a support system, engaging in regular therapy sessions, and setting realistic expectations are equally important aspects. Regular self-reflection and journaling can also aid in recognizing early warning signs and adapting strategies to prevent relapse.
Potential Warning Signs of Relapse
Recognizing potential warning signs of relapse is critical in maintaining remission. These signs may include changes in mood, sleep patterns, appetite, energy levels, or concentration. Increased irritability, social withdrawal, or a decline in interest in previously enjoyed activities are also potential indicators. Individuals should actively monitor these subtle changes and promptly address them through established coping mechanisms.
Practical Tips for Maintaining Remission
- Establish a consistent sleep schedule to ensure adequate rest.
- Maintain a healthy diet rich in fruits, vegetables, and lean proteins for optimal physical health.
- Engage in regular physical activity to reduce stress and improve mood.
- Practice mindfulness techniques, such as meditation or deep breathing exercises, to manage stress.
- Develop healthy coping mechanisms to manage stress and difficult emotions.
- Cultivate a strong support system of friends, family, or support groups.
- Prioritize self-compassion and acceptance of imperfections.
- Schedule regular appointments with mental health professionals for ongoing support and guidance.
- Maintain open communication with loved ones about your mental health journey.
- Engage in activities that bring joy and fulfillment.
Challenges and Considerations
Navigating the path to depression remission isn’t always straightforward. While effective treatments and strategies exist, achieving and maintaining remission often presents hurdles. Understanding these challenges is crucial for developing personalized approaches that support individuals throughout their journey. This section delves into the common obstacles, societal influences, and the importance of patient-centered care in fostering long-term well-being.
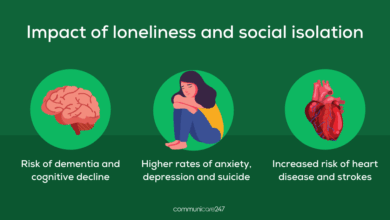
Common Obstacles to Remission
Sustaining remission requires ongoing effort and vigilance. Individuals may encounter setbacks due to various factors. Relapse can stem from stressors, both anticipated and unexpected, which can trigger depressive symptoms. These may include significant life changes, relationship issues, financial pressures, or even the absence of social support. The absence of effective coping mechanisms or a lack of proactive strategies to manage these stressors can also contribute to relapse.
Furthermore, some individuals may experience difficulty in adhering to prescribed treatment plans, whether due to side effects, logistical challenges, or a lack of motivation.
Societal and Cultural Factors
Societal and cultural norms can profoundly impact the experience of depression and the pursuit of remission. Stigma surrounding mental illness can discourage individuals from seeking help or disclosing their struggles. This can lead to feelings of isolation, shame, and reluctance to engage in necessary treatments, hindering progress towards remission. Cultural beliefs and values may also influence how depression is understood and treated.
For example, in some cultures, mental health issues might be viewed as a sign of weakness or a family disgrace, leading individuals to conceal their struggles and avoid seeking professional help. The cultural landscape plays a significant role in shaping access to resources and treatment options.
Addressing Stigma
The stigma associated with depression remission is a significant challenge. Individuals may feel pressure to conform to societal expectations or fear judgment from loved ones, friends, or colleagues. Open and honest conversations about mental health are crucial in combating stigma. Educating others about the nature of depression and remission can foster empathy and understanding. Encouraging individuals to share their experiences and highlight their resilience can also help reduce the social isolation and judgment that often accompany mental health challenges.
Importance of Patient-Centered Care
Patient-centered care is vital for promoting successful remission. This approach emphasizes the individual’s unique needs, preferences, and experiences. It involves collaboration between the patient and healthcare professionals, ensuring that treatment plans are tailored to the individual’s specific circumstances and goals. This personalized approach allows for proactive management of potential challenges, facilitates open communication about setbacks, and empowers individuals to take an active role in their recovery.
This collaborative partnership builds trust and fosters a supportive environment conducive to sustained remission.
Available Resources
Numerous resources are available to support individuals in their journey towards remission. Support groups, online forums, and mental health professionals can provide valuable guidance and encouragement. Self-help books, educational materials, and online resources offer practical strategies and coping mechanisms. Mental health organizations and government agencies often provide access to information and support services. Furthermore, community centers and local organizations frequently offer workshops, seminars, and support groups designed to assist individuals in their recovery journey.
Common Challenges and Potential Solutions
| Challenge | Potential Solution |
|---|---|
| Relapse due to unforeseen stressors | Developing coping mechanisms, stress management techniques, and establishing a support network. |
| Difficulty adhering to treatment plans | Open communication with healthcare providers, exploring alternative treatment options, and addressing any logistical or financial barriers. |
| Stigma and social isolation | Educating others about depression and remission, joining support groups, and promoting open conversations about mental health. |
| Lack of patient-centered care | Advocating for individualized treatment plans, actively participating in treatment decisions, and seeking out healthcare providers who prioritize patient-centered care. |
Closing Summary
Ultimately, the possibility of depression remission underscores the importance of personalized care and proactive strategies. By understanding the interplay of biological, psychological, and environmental factors, individuals can work collaboratively with healthcare professionals to create a path toward sustained well-being. It’s a journey, not a destination, and the commitment to self-care, support, and open communication is paramount in achieving and maintaining remission.