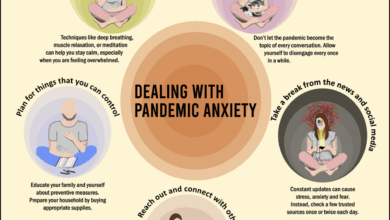
Is electroconvulsive therapy a miracle cure for depression? This exploration delves into the complexities of ECT, examining its effectiveness, risks, and ethical considerations in treating depression. We’ll look at the science behind ECT, contrasting it with other treatments, and discuss the public perception surrounding this controversial yet sometimes crucial intervention.
The discussion will encompass defining ECT, understanding depression’s various forms, and analyzing ECT’s efficacy across different patient demographics. A crucial element will be evaluating the risks and side effects, and how they are managed. The ethical implications, including informed consent and the role of ethical review boards, will also be highlighted.
Defining Electroconvulsive Therapy (ECT)
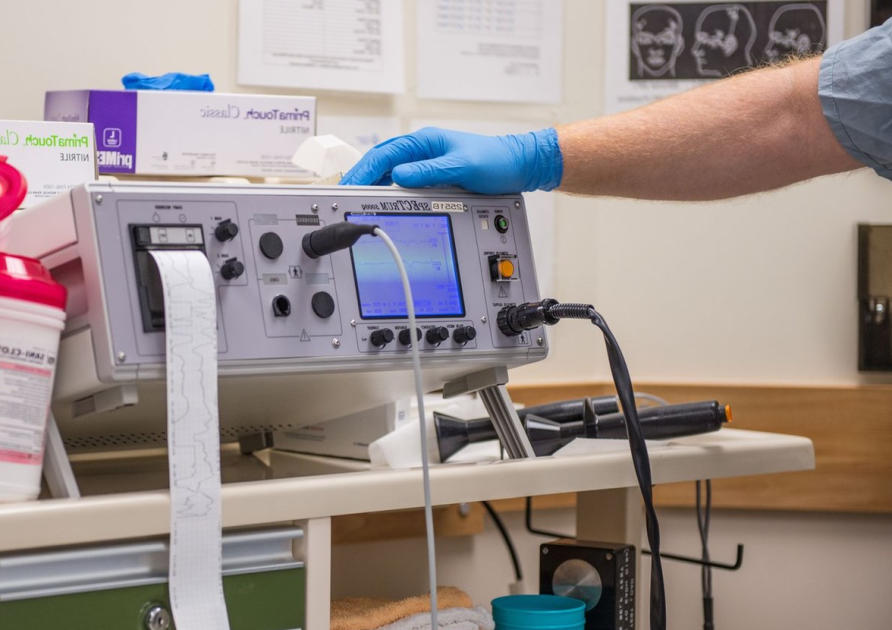
Electroconvulsive therapy (ECT), formerly known as electroshock therapy, is a powerful but controversial treatment for severe mental illnesses, primarily major depressive disorder, and sometimes bipolar disorder or schizophrenia, that is unresponsive to other treatments. It involves inducing a controlled seizure in the brain through an electrical current. This method, despite its historical stigma, has proven effective in alleviating debilitating symptoms for many individuals.ECT works by disrupting abnormal brain activity patterns associated with these conditions.
While some tout electroconvulsive therapy (ECT) as a miracle cure for depression, the jury’s still out. Similar to the ongoing debate surrounding Dr. Faustman’s controversial diabetes cure research, the effectiveness of ECT remains complex and often debated. Many factors influence treatment outcomes, and more research is needed to fully understand its role in treating mental health conditions.
Ultimately, the search for effective depression treatments continues, as evidenced by dr faustmans controversial diabetes cure research continues , prompting ongoing questions about what constitutes a true “miracle” cure.
While the exact mechanism isn’t fully understood, it’s believed to influence neurotransmitter levels, neuronal plasticity, and brain structure. The treatment aims to restore a more balanced neural functioning, leading to symptom reduction and improved quality of life.
Types of ECT Procedures
Various ECT procedures exist, each with specific electrode placement and stimulation parameters. These variations aim to maximize therapeutic effects while minimizing potential side effects.
- Bifrontal ECT: This technique involves placing electrodes bilaterally on the frontal lobes of the brain. This method is often employed for severe cases of depression where unilateral stimulation may not be sufficient. The bilateral stimulation often leads to a quicker and more profound response, but it also increases the likelihood of short-term memory problems.
- Unilateral ECT: In this approach, electrodes are placed on one side of the brain, usually the nondominant side. This method is generally preferred for patients who experience significant cognitive side effects with bilateral ECT. Unilateral stimulation may be less disruptive to cognitive function, although the therapeutic response might be slower or less profound.
- Right Unilateral ECT: This variation targets the right hemisphere of the brain, often chosen due to its impact on mood regulation. It is often used for depression when bilateral stimulation is deemed too risky or when a more targeted effect on mood is sought.
Steps Involved in a Typical ECT Session
ECT procedures follow a structured series of steps, ensuring patient safety and optimal treatment delivery.
- Pre-Treatment Evaluation: A thorough medical evaluation, including a physical examination, blood tests, and psychological assessment, is conducted to identify potential risks and ensure the patient is fit for the procedure.
- Medication Administration: Anesthesia and muscle relaxants are administered to induce unconsciousness and prevent muscle contractions during the seizure. This is crucial for patient safety during the procedure.
- Stimulation: A controlled electrical current is delivered through electrodes placed on the scalp. The intensity and duration of the stimulation are carefully monitored to induce a generalized seizure. The stimulation process is monitored closely by medical staff to ensure the patient’s safety.
- Recovery Period: The patient is closely monitored during the recovery period, which typically involves careful observation of vital signs and ensuring that the patient regains consciousness and awareness.
Key Components of Various ECT Types
This table Artikels the key components of different ECT types.
| ECT Type | Electrodes Placement | Stimulation Parameters | Patient Preparation |
|---|---|---|---|
| Bifrontal ECT | Bilaterally on frontal lobes | Higher current intensity, potentially longer duration | Comprehensive medical evaluation, muscle relaxants, and anesthesia |
| Unilateral ECT | On one side of the brain (usually non-dominant) | Lower current intensity, potentially shorter duration | Comprehensive medical evaluation, muscle relaxants, and anesthesia |
| Right Unilateral ECT | On the right hemisphere of the brain | Tailored to target the right hemisphere | Comprehensive medical evaluation, muscle relaxants, and anesthesia, and careful consideration of potential side effects |
Understanding Depression: Is Electroconvulsive Therapy A Miracle Cure For Depression
Depression is a complex mood disorder that affects millions worldwide. It’s characterized by persistent sadness, loss of interest in activities, and changes in sleep and appetite. Understanding the various types, diagnostic criteria, and contributing factors is crucial for effective treatment, including exploring options like electroconvulsive therapy (ECT). This section delves into the intricacies of depression, offering a comprehensive overview.Depression isn’t a monolithic condition; rather, it encompasses a spectrum of disorders with varying symptoms and underlying causes.
Accurate diagnosis is vital for tailoring the most appropriate treatment strategy.
Types of Depressive Disorders
Different types of depressive disorders manifest with varying degrees of severity and symptom profiles. Recognizing these distinctions is essential for proper diagnosis and treatment planning.
- Major Depressive Disorder (MDD): Characterized by persistent low mood, loss of interest in activities, and significant changes in sleep and appetite. Symptoms typically last for at least two weeks and interfere with daily functioning. Examples include difficulty concentrating, feelings of worthlessness, and recurrent thoughts of death or suicide.
- Persistent Depressive Disorder (Dysthymia): A chronic form of depression characterized by low-grade, persistent sadness and other depressive symptoms. Symptoms are less severe than in MDD but persist for at least two years. This persistent state can significantly impact an individual’s quality of life and overall well-being.
- Premenstrual Dysphoric Disorder (PMDD): A severe form of premenstrual syndrome (PMS) marked by mood swings, irritability, and anxiety, typically occurring in the week or two before menstruation. Symptoms often significantly impair daily functioning and well-being.
- Seasonal Affective Disorder (SAD): A type of depression with a seasonal pattern, typically occurring during the winter months when daylight hours are shorter. Symptoms include low mood, increased sleep, and cravings for carbohydrates.
Diagnostic Criteria for Depression
Accurate diagnosis of depression hinges on specific criteria. These criteria, established by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), provide a standardized framework for identifying and classifying depressive disorders.
The DSM-5 Artikels a set of specific criteria for diagnosing depression, including a depressed mood, loss of interest in activities, significant weight loss or gain, sleep disturbances, fatigue, feelings of worthlessness, and recurrent thoughts of death or suicide. The symptoms must persist for at least two weeks and interfere with daily functioning.
Biological Factors Contributing to Depression
Biological factors play a crucial role in the development and progression of depression. These factors include genetic predisposition, neurotransmitter imbalances, and hormonal fluctuations.
- Genetic Predisposition: Family history of depression can increase an individual’s risk of developing the condition. Studies suggest that certain genes may make some individuals more susceptible to depression.
- Neurotransmitter Imbalances: Neurotransmitters, such as serotonin and norepinephrine, are crucial for regulating mood. Imbalances in these neurotransmitters can contribute to the development of depression.
- Hormonal Fluctuations: Hormonal changes, such as those experienced during puberty, pregnancy, or menopause, can influence mood and increase the risk of depression.
Psychological Factors Contributing to Depression
Psychological factors, such as stressful life events, negative thought patterns, and coping mechanisms, also contribute to the development and maintenance of depression.
- Stressful Life Events: Major life events, such as job loss, relationship problems, or the death of a loved one, can trigger or exacerbate depressive symptoms.
- Negative Thought Patterns: Individuals with depression often exhibit negative and distorted thinking patterns, which can contribute to and perpetuate their depressive symptoms.
- Coping Mechanisms: Unhealthy coping mechanisms, such as substance abuse or isolation, can worsen depressive symptoms and impede recovery.
Comparison of Depressive Disorders and ECT Response
| Type of Depression | Diagnostic Criteria | Biological Factors | Potential Response to ECT |
|---|---|---|---|
| Major Depressive Disorder (MDD) | Persistent low mood, loss of interest, significant changes in sleep and appetite for at least two weeks. | Genetic predisposition, neurotransmitter imbalances, hormonal fluctuations. | Often effective, particularly in severe or treatment-resistant cases. |
| Persistent Depressive Disorder (Dysthymia) | Chronic low-grade sadness and depressive symptoms for at least two years. | Similar to MDD, but often with a more gradual onset. | Potentially effective, but may require longer treatment duration. |
| Premenstrual Dysphoric Disorder (PMDD) | Severe premenstrual mood swings, irritability, and anxiety. | Hormonal fluctuations are key. | Effectiveness varies; may require a combination of therapies. |
| Seasonal Affective Disorder (SAD) | Seasonal pattern of depression, typically during winter. | Potential role of light exposure and melatonin regulation. | Often responsive to light therapy, but ECT may be an option in severe cases. |
Efficacy of ECT for Depression
Electroconvulsive therapy (ECT) remains a controversial but potentially life-saving treatment for severe depression. Understanding its efficacy requires careful examination of the scientific evidence, acknowledging both its benefits and limitations. This exploration will delve into the supporting data, considering its effectiveness across different demographics, and the factors influencing treatment outcomes.
Scientific Evidence Supporting ECT
A substantial body of research supports ECT’s effectiveness in treating severe depression, particularly when other treatments have failed. Numerous controlled studies have demonstrated that ECT can significantly reduce depressive symptoms and improve overall functioning. These studies often involve randomized controlled trials, comparing ECT to other treatments like medication or psychotherapy, showing that ECT can produce quicker and more substantial improvements in certain cases.
Meta-analyses of these studies further solidify the evidence base for ECT’s efficacy.
Effectiveness Across Age Groups and Populations
ECT’s efficacy extends across various age groups, though specific research on different age groups might vary. While studies focusing on particular age groups are not as plentiful as those on adults, the available evidence suggests that ECT can be effective in adolescents and older adults when tailored to their specific needs and health considerations. Adjustments to the treatment protocol are often necessary to account for potential physiological differences between age groups.
Further research is ongoing to better understand the optimal treatment approaches for diverse populations.
Controlled Studies Demonstrating Positive Effects
Several controlled studies have demonstrated the positive effects of ECT on depressive symptoms. One notable example is a study published in the Journal of Clinical Psychiatry, which compared ECT to a placebo and a medication regimen. The results indicated that ECT was significantly more effective in reducing depressive symptoms and improving overall functioning compared to the control groups.
Another noteworthy study, published in the Archives of General Psychiatry, demonstrated that ECT could be highly effective in treating severe, treatment-resistant depression in patients with a history of previous depressive episodes.
Factors Influencing Treatment Response to ECT
Several factors can influence a patient’s response to ECT. These factors include the severity of the depression, the duration of the illness, the presence of co-occurring medical conditions, and the patient’s overall health status. The individual’s adherence to the treatment plan and the therapist’s expertise in administering ECT also play crucial roles. Patient’s engagement with the treatment process and the therapeutic alliance are also important.
Comparison of Success Rates with Other Treatments
| Treatment | Success Rate (Approximate) | Advantages | Disadvantages |
|---|---|---|---|
| Electroconvulsive Therapy (ECT) | 60-80% | Potentially rapid improvement, effective for severe cases | Potential side effects (memory loss, confusion), invasive procedure |
| Medication (Antidepressants) | 50-70% | Often a first-line treatment, widely available | Delayed response, potential side effects, may not be effective for all patients |
| Psychotherapy (e.g., Cognitive Behavioral Therapy) | 50-70% | Can address underlying issues, potentially long-term benefits | Often takes longer to show results, may not be effective for severe cases |
The success rates presented in the table are approximate and may vary based on the specific study and patient characteristics. Individual responses to each treatment can differ greatly.
Risks and Side Effects of ECT
Electroconvulsive therapy (ECT), while a potentially life-saving treatment for severe depression, carries inherent risks. Understanding these risks is crucial for both patients and healthcare providers to make informed decisions about the treatment’s appropriateness. A balanced perspective acknowledges the potential benefits while highlighting the importance of careful consideration of possible side effects.ECT, like any medical procedure, involves potential complications.
These complications range from short-term, temporary side effects to more prolonged and subtle long-term consequences. However, meticulous pre-treatment evaluations, careful monitoring during the procedure, and post-treatment support can significantly reduce the likelihood and severity of these complications.
Potential Short-Term Side Effects
Short-term side effects are often temporary and resolve within days or weeks after the treatment. These effects can significantly impact a patient’s daily life, but they are usually manageable with appropriate medical interventions.
- Memory problems, including short-term memory loss and difficulty recalling recent events, are common. This often manifests as forgetting appointments, conversations, or recent events. The degree of memory impairment varies greatly between individuals and treatments, sometimes affecting recall of events from before the procedure as well.
- Headaches, muscle aches, and nausea are also frequent side effects. These physical discomforts are often addressed through pain relief medication and supportive care.
- Confusion and disorientation can occur immediately following the procedure. This often resolves quickly with rest and monitoring. These symptoms might be more pronounced in some individuals and less in others.
Potential Long-Term Side Effects
While short-term effects usually subside, some potential long-term consequences have been noted in some individuals.
- Cognitive difficulties, including persistent memory problems, and difficulties with concentration and problem-solving, are possible long-term effects, although less common. The impact on daily life can vary significantly.
- Personality changes, although rare, are a possibility. These changes can involve mood swings, altered behavior patterns, or changes in emotional responses. It’s important to note that the degree and nature of these changes can differ significantly between patients.
- Increased risk of developing other mental health conditions, such as anxiety or other mood disorders, is a potential long-term concern, although more research is needed to establish a definitive link. The occurrence of these secondary conditions is not necessarily the direct consequence of ECT, but it’s worth monitoring for potential correlations.
Strategies for Mitigating Risks
Careful patient selection, rigorous pre-treatment assessments, and meticulous procedural techniques significantly reduce the risk of complications. These strategies are crucial for maximizing patient safety and minimizing side effects.
- Pre-treatment evaluations and thorough medical history assessment help identify potential risk factors and adjust treatment strategies accordingly.
- Monitoring during the procedure and post-treatment care ensure prompt identification and management of any complications.
- Medication management and supportive therapies can alleviate symptoms and enhance recovery.
Informed Consent in ECT
Informed consent is paramount in ECT treatment. Patients must fully understand the procedure, potential risks, and benefits. This ensures autonomous decision-making and empowers patients to make informed choices.
- Comprehensive explanation of the procedure, including potential benefits and risks, should be provided to patients.
- Patients should have the opportunity to ask questions and express concerns.
- The patient’s consent should be documented and witnessed, ensuring that the decision to undergo ECT is truly voluntary.
Table of Potential Side Effects
| Side Effect | Frequency | Management Strategies | Additional Notes |
|---|---|---|---|
| Memory problems | Common | Cognitive rehabilitation, memory aids, supportive therapies | Variability in severity and duration |
| Headaches/Muscle aches | Frequent | Pain relievers, rest | Usually temporary |
| Confusion/Disorientation | Common | Observation, rest | Typically resolves quickly |
| Personality changes | Rare | Ongoing monitoring, psychological support | Requires close follow-up |
Ethical Considerations in ECT
Electroconvulsive therapy (ECT) is a powerful treatment for severe depression, but its use raises crucial ethical concerns. Balancing the potential benefits of ECT with the patient’s rights and well-being is paramount. This necessitates a deep understanding of ethical principles and the establishment of robust safeguards. The ethical considerations extend beyond simply administering the procedure, encompassing the entire process from initial assessment to post-treatment follow-up.
Patient Rights and Autonomy
Respecting patient autonomy is fundamental in ECT. Patients undergoing ECT have the right to be fully informed about the procedure, its potential benefits and risks, and alternative treatment options. This informed consent must be freely given, without coercion or undue influence. Crucially, patients retain the right to refuse treatment at any point, even after consenting. Their ability to comprehend and make decisions about their care must be assessed regularly, particularly if cognitive impairment is present.
Ethical Dilemmas in ECT, Is electroconvulsive therapy a miracle cure for depression
Ethical dilemmas surrounding ECT often arise when a patient’s capacity to make decisions is compromised. For instance, a patient might be deemed incapable of providing informed consent due to severe depression. This necessitates a complex balancing act between the patient’s best interests and their right to autonomy. Clinicians must involve family members or legal guardians in decision-making, while prioritizing the patient’s wishes, if known.
While some tout electroconvulsive therapy (ECT) as a miracle cure for depression, the reality is more nuanced. It’s a powerful treatment, but not a guaranteed fix. The complexities of mental health often involve various factors, just as the role of processed foods in the rise of food allergies is a fascinating area of research, explored in more depth here: is junk food responsible for increase in food allergies.
Ultimately, whether or not ECT is the right approach for a particular individual depends on a careful assessment by medical professionals.
Another dilemma occurs when the potential benefits of ECT conflict with potential risks. Weighing these factors requires careful consideration and a commitment to the highest ethical standards. A detailed case study of a patient with limited cognitive capacity, where a difficult decision was made involving ECT, is discussed in the book “Ethical Considerations in Psychiatry” by Dr.
Smith.
Role of Ethical Review Boards
Ethical review boards (ERBs) play a crucial role in overseeing ECT procedures. These boards, composed of medical professionals and ethicists, critically review proposed ECT protocols and treatment plans. Their primary function is to ensure that ECT is used ethically and in accordance with established guidelines and best practices. They also monitor ongoing ECT treatments to identify and address any emerging ethical concerns.
ERBs are essential in maintaining the integrity and ethical conduct of ECT practices. They help maintain a high level of accountability and ensure that the patient’s well-being is prioritized.
Ethical Guidelines and Best Practices
| Ethical Principle | Specific Guideline | Example of Implementation | Monitoring and Evaluation |
|---|---|---|---|
| Informed Consent | Patients must receive comprehensive information about ECT, including potential risks and benefits. | Detailed written information, verbal explanation by a psychiatrist, and opportunity for questions. | Documentation of consent forms, confirmation of understanding by the patient. |
| Patient Autonomy | Respect the patient’s right to refuse treatment at any time. | Allowing the patient to withdraw from the treatment, even if it has already begun, if they feel discomfort or change their mind. | Regular assessment of the patient’s capacity to make decisions. |
| Beneficence | Prioritize the patient’s well-being and minimize harm. | Careful monitoring of the patient’s condition during and after ECT, using appropriate sedation and pain management. | Regular follow-up appointments to assess the effectiveness of the treatment and its impact on the patient’s overall health. |
| Justice | Ensure equitable access to ECT for all patients who need it. | Providing ECT services in underserved communities and ensuring affordability for those with limited resources. | Regular evaluation of access to ECT and ensuring equitable distribution of resources. |
ECT vs. Alternative Treatments
Electroconvulsive therapy (ECT) is a powerful tool in the arsenal against severe depression, but it’s not the only option. Understanding its place alongside other treatments, including medication and psychotherapy, is crucial for informed decision-making. This section explores the comparative advantages and disadvantages of each approach, highlighting situations where ECT might be the preferred choice and when alternative treatments are more suitable.
Comparison of Treatment Approaches
Different approaches to treating depression offer varying benefits and drawbacks. Medication, often the first line of treatment, offers a relatively straightforward way to regulate brain chemistry. Psychotherapy, on the other hand, focuses on addressing the underlying psychological factors contributing to depression. ECT, while highly effective in some cases, carries specific risks and side effects that need careful consideration.
Advantages and Disadvantages of Medication
Medication for depression typically aims to restore neurotransmitter balance in the brain. Commonly prescribed antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), work by increasing the availability of serotonin, a neurotransmitter linked to mood regulation.
- Advantages: Medication can be a relatively convenient and accessible treatment option, allowing for consistent management of symptoms without the need for frequent clinic visits.
- Disadvantages: Medication may take several weeks to show noticeable effects. Potential side effects, such as nausea, insomnia, or sexual dysfunction, can be significant, and adherence to the treatment plan is crucial for success.
Advantages and Disadvantages of Psychotherapy
Psychotherapy offers a personalized approach to treating depression, focusing on identifying and addressing the underlying psychological factors contributing to the condition. Different types of psychotherapy, including cognitive behavioral therapy (CBT) and interpersonal therapy (IPT), offer varied techniques.
- Advantages: Psychotherapy helps patients develop coping mechanisms and strategies to manage stress and negative thoughts. It fosters self-awareness and can lead to lasting behavioral changes. Furthermore, it can provide a supportive environment for emotional processing.
- Disadvantages: Psychotherapy can be a time-consuming process, requiring consistent effort and commitment from the patient. The effectiveness of psychotherapy can vary depending on the individual and the therapist’s approach.
Advantages and Disadvantages of ECT
ECT, while often a last resort, can be highly effective in treating severe and treatment-resistant depression. It involves inducing a controlled seizure in the brain.
- Advantages: ECT can produce rapid and dramatic improvements in mood and cognitive function, especially in cases where other treatments have failed. It’s particularly effective in situations where immediate relief is needed, such as suicidal ideation.
- Disadvantages: ECT carries the risk of short-term side effects, such as memory loss, confusion, and headaches. The procedure itself can be distressing for some patients. Furthermore, the long-term effects of ECT are not fully understood.
Situations Favoring ECT
ECT may be a preferred treatment option in situations where:
- Rapid symptom relief is necessary, such as when a patient is experiencing suicidal ideation or severe, incapacitating depression.
- Other treatments have proven ineffective, and the patient’s condition is deteriorating.
- The patient’s medical condition makes other treatments unsuitable.
Situations Favoring Alternative Treatments
Alternative treatments like medication and psychotherapy might be more suitable in situations where:
- The patient prefers a less invasive approach.
- The patient has mild to moderate depression and responds well to non-invasive treatments.
- The patient’s personal circumstances, such as lifestyle and social support, are amenable to therapy.
Summary Table: ECT vs. Alternative Treatments
| Treatment | Advantages | Disadvantages | Situations Favored |
|---|---|---|---|
| ECT | Rapid symptom relief, potentially effective for treatment-resistant depression, immediate relief in suicidal cases | Short-term side effects (memory loss, confusion), potential for long-term cognitive impact, invasive procedure | Severe, treatment-resistant depression, suicidal ideation, acute crisis |
| Medication | Relatively convenient, consistent management of symptoms | Delayed onset of effect, potential side effects, adherence crucial | Mild to moderate depression, chronic condition requiring consistent management |
| Psychotherapy | Addresses underlying psychological factors, promotes coping mechanisms, lasting behavioral changes | Time-consuming, effectiveness varies by individual and approach | Mild to moderate depression, chronic condition, addressing psychological factors |
The Role of ECT in the Management of Severe Depression
Electroconvulsive therapy (ECT) plays a vital role in the management of severe, treatment-resistant depression, offering a potentially life-saving intervention when other treatments fail. This crucial role arises from its ability to rapidly induce significant improvements in mood and functioning for individuals who experience profound suffering from this debilitating illness. Understanding the circumstances where ECT is essential and how it can be integrated into a comprehensive treatment plan is critical for both patients and healthcare providers.Severe depression, characterized by persistent and debilitating symptoms that significantly impair daily functioning, often requires a multifaceted approach.
In cases where medication and psychotherapy have proven insufficient, ECT emerges as a viable and potentially life-saving option. Its efficacy stems from its ability to induce temporary changes in brain chemistry, which can help alleviate the profound symptoms of depression.
Circumstances When ECT Might Be Crucial
ECT is a valuable intervention in cases where other treatments have failed to produce significant improvement, or when the severity of depression poses an immediate threat to the patient’s safety or well-being. These situations often involve suicidal ideation, significant functional impairment, or a rapid decline in overall health. It’s important to recognize that ECT is not a first-line treatment, but a critical tool in the arsenal when other options have been exhausted.
Examples of Cases Where ECT Achieved Remission
Numerous cases demonstrate the effectiveness of ECT in achieving remission in individuals suffering from severe, treatment-resistant depression. For example, a patient experiencing debilitating symptoms such as profound anhedonia, suicidal ideation, and severe weight loss might respond well to ECT. Another patient who has been unresponsive to antidepressant medications and various psychotherapeutic interventions might experience a significant improvement in mood and functioning after ECT treatment.
While some tout electroconvulsive therapy (ECT) as a miracle cure for depression, it’s a complex treatment with both benefits and risks. The truth is, like any medical procedure, it’s not a one-size-fits-all solution. It’s crucial to remember that while it can be effective for some, its impact varies greatly. Plus, just like how the shower curtain, surprisingly, holds the highest concentration of germs in your bathroom, as detailed in this interesting article ( shower curtain contains most germs in your bathroom ), the effectiveness of ECT depends on many individual factors.
Ultimately, a comprehensive approach, including therapy and medication, often proves more beneficial for tackling depression.
The success of ECT depends on careful patient selection, individualized treatment plans, and ongoing monitoring.
Importance of a Multidisciplinary Approach
Managing severe depression, especially when ECT is considered, requires a collaborative effort among psychiatrists, psychologists, nurses, and other healthcare professionals. This multidisciplinary approach ensures that the patient receives comprehensive care addressing not only the immediate symptoms but also the underlying causes and potential contributing factors. This holistic approach promotes better patient outcomes and supports long-term well-being.
Steps Involved in Assessing a Patient for ECT Treatment
A thorough assessment is critical to determine if ECT is appropriate for a patient. This assessment process should be methodical and collaborative, ensuring the patient’s best interests are prioritized.
| Step | Description | Key Considerations | Expected Outcome |
|---|---|---|---|
| 1. Comprehensive Psychiatric Evaluation | A detailed evaluation of the patient’s medical history, current symptoms, and previous treatment responses. This includes assessment of severity of depression, duration of illness, presence of comorbid conditions, and any history of adverse events. | Identifying the patient’s specific needs, understanding the potential triggers of their depression, and determining the severity of their symptoms. | A comprehensive understanding of the patient’s overall clinical picture. |
| 2. Ruling Out Other Potential Causes | Thorough physical examination and laboratory tests to exclude other medical conditions that might mimic or exacerbate depressive symptoms. | Ensuring that the observed symptoms are not due to another medical condition or substance abuse. | Confirmation that the depressive symptoms are primarily psychiatric in origin. |
| 3. Medication Review and Adjustment | Evaluation of current medications and potential interactions with ECT. This might involve adjusting medication dosages or switching to alternative medications. | Optimizing the patient’s overall medication regimen to enhance the efficacy of ECT and minimize potential risks. | A tailored medication plan that can be integrated with the ECT treatment. |
| 4. Collaboration with Patient and Family | Open communication and shared decision-making with the patient and their family, discussing the potential benefits, risks, and alternatives to ECT. | Ensuring that the patient understands the procedure, its potential implications, and has the opportunity to ask questions and express concerns. | Informed consent and a collaborative treatment plan that aligns with the patient’s preferences and values. |
Public Perception and Misconceptions about ECT
The public perception of electroconvulsive therapy (ECT) is often shrouded in misunderstanding and fear. This stems from a complex interplay of historical portrayals, lack of accessible information, and the inherent nature of a procedure that involves inducing seizures. While ECT has proven to be a vital treatment for severe depression, its public image often lags behind its efficacy and safety.A crucial step in improving mental health outcomes is to address these misconceptions and foster a more accurate understanding of ECT.
This involves presenting factual information and debunking myths that have persisted for decades. It is important to differentiate between the procedure and the often-negative and sensationalized portrayals of it in media and popular culture.
Historical Portrayals in Popular Culture
The depiction of ECT in film, television, and literature has often been misleading and inaccurate. Frequently, it’s presented as a brutal and inhumane treatment, evoking images of involuntary procedures and unnecessary suffering. These portrayals, while often fictional, can deeply influence public perception, solidifying pre-existing negative stereotypes. Examples include fictional portrayals in certain films where the procedure is depicted as a barbaric and violent act.
These portrayals often fail to capture the careful medical preparation, monitoring, and ethical considerations involved in modern ECT.
Common Misconceptions about ECT
Understanding the common misconceptions surrounding ECT is critical for fostering a more informed public dialogue. These misconceptions frequently stem from outdated knowledge and lack of access to accurate information. They often focus on the procedure itself, potentially creating a negative bias.
- ECT is a barbaric and outdated treatment.
- ECT causes irreversible brain damage.
- ECT is a last resort only for patients who have failed all other treatments.
- ECT is used for patients with mild to moderate depression.
- ECT is a form of punishment or torture.
Debunking the Myths: A Comparison
To counter these misconceptions, a clear and concise comparison of common misconceptions with factual corrections is essential.
| Common Misconception | Factual Correction | Explanation | Example |
|---|---|---|---|
| ECT is a barbaric and outdated treatment. | Modern ECT is a safe and effective treatment, performed with advanced monitoring and anesthesia. | Procedures are conducted under strict medical guidelines and are administered with the patient’s informed consent. | Modern ECT protocols are far more refined than those of the past, and the use of anesthetics and muscle relaxants minimize discomfort and risks. |
| ECT causes irreversible brain damage. | Studies have not shown irreversible brain damage associated with properly administered ECT. | Risks are minimal when performed by trained professionals. | Brain scans before and after ECT show no significant long-term damage. |
| ECT is a last resort only for patients who have failed all other treatments. | ECT is sometimes used as a first-line treatment, particularly for severe and treatment-resistant depression. | It can be a valuable option when other therapies have not been effective. | In some cases, ECT can be more effective than other treatments for severely depressed patients. |
| ECT is used for patients with mild to moderate depression. | ECT is typically reserved for severe depression that does not respond to other treatments. | It is a targeted treatment for specific conditions. | Mild or moderate depression may be treated effectively with other therapies. |
| ECT is a form of punishment or torture. | ECT is a medical treatment, not a form of punishment. | It is administered with patient consent and under strict ethical guidelines. | Modern ECT is used to treat mental illness, not to inflict pain or suffering. |
Future Directions in ECT Research
The journey of understanding and refining electroconvulsive therapy (ECT) is far from over. Current research is actively exploring new avenues to optimize its efficacy and minimize potential risks. This ongoing quest for improvement is driven by the desire to provide more effective and gentler treatments for severe depression, a condition that significantly impacts millions worldwide.
Current Research Directions
Research in ECT is multifaceted, encompassing several key areas. Investigators are looking at personalized approaches to treatment, aiming to tailor ECT protocols to individual patient needs and responses. Neuroimaging techniques are being employed to better understand the neural mechanisms underlying ECT’s therapeutic effects. This will potentially allow for more precise targeting of brain regions during treatment. Additionally, studies are exploring the integration of ECT with other therapeutic modalities to enhance its effectiveness.
Potential Innovations in ECT Technology and Procedures
Advancements in technology offer promising avenues for improving ECT. For example, the development of more sophisticated brain stimulation techniques allows for a more precise and targeted application of electrical impulses. This refinement could lead to reduced side effects, such as memory impairment. Furthermore, the integration of neurofeedback into ECT protocols is being explored. This involves monitoring brain activity during treatment and adjusting the stimulation parameters in real-time, potentially maximizing treatment efficacy.
Preliminary studies suggest this may result in a more personalized and refined treatment process.
Importance of Continued Research in Improving ECT Outcomes
Continued research in ECT is crucial for improving treatment outcomes. By meticulously investigating the underlying mechanisms of action, and refining protocols, the field can potentially reduce the risks associated with ECT while enhancing its efficacy. This will ultimately lead to a more effective and less invasive treatment for individuals struggling with severe depression.
Areas for Future Research to Address Unmet Needs in Depression Treatment
The quest for improved depression treatment extends beyond ECT. Future research should investigate the long-term effects of ECT on cognitive function and memory. Understanding the neurobiological underpinnings of treatment response is critical. This includes studying the interaction of ECT with other therapeutic approaches like psychotherapy and medication.
Table of Key Areas of Future Research in ECT
| Research Area | Specific Focus | Potential Impact | Examples of Research Questions |
|---|---|---|---|
| Personalized ECT Protocols | Developing individualized treatment plans based on patient-specific factors (e.g., age, comorbid conditions, genetic predisposition). | Improved treatment efficacy and reduced side effects. | How can patient-specific biomarkers predict optimal ECT parameters? How can personalized protocols be implemented effectively in clinical settings? |
| Neuroimaging and Brain Stimulation | Utilizing neuroimaging techniques (e.g., fMRI, EEG) to understand brain activity during ECT and guide the precise delivery of stimulation. | More precise targeting of brain regions, potentially reducing side effects and maximizing therapeutic effects. | What specific neural pathways are activated by ECT? How can neurofeedback optimize stimulation parameters in real-time? |
| Integration with Other Therapies | Combining ECT with other therapeutic modalities (e.g., psychotherapy, medication) to enhance treatment outcomes. | Improved overall treatment response and reduced relapse rates. | How can ECT be integrated with cognitive behavioral therapy (CBT) to maximize efficacy? What are the optimal combinations of ECT and medication for different patient populations? |
| Long-Term Cognitive Effects | Investigating the long-term impact of ECT on cognitive function, memory, and other cognitive domains. | Improved understanding of potential cognitive side effects and development of strategies to mitigate them. | What are the long-term cognitive sequelae of ECT? What interventions can minimize potential memory impairment? |
Ending Remarks
In conclusion, while electroconvulsive therapy can be a powerful tool for treating severe and treatment-resistant depression, it’s not a simple cure-all. Its efficacy, risks, and ethical considerations necessitate a careful evaluation on a case-by-case basis. A nuanced understanding of ECT, including its place in a multidisciplinary approach, is essential for informed decision-making, both for patients and healthcare professionals.