Lack of vitamin D and gum disease higher diabetes risk sets the stage for this intriguing exploration. This article delves into the potential connections between these seemingly disparate health concerns, examining the scientific understanding of how they might be linked and the potential mechanisms at play. We’ll explore the roles of vitamin D, inflammation, and the gut microbiome in the development of these conditions.
Furthermore, we’ll examine risk factors, prevention strategies, and future research directions.
Understanding the potential link between vitamin D deficiency, gum disease, and diabetes risk is crucial for proactive health management. This comprehensive look at the interconnectedness of these conditions offers valuable insights into preventative measures and highlights the importance of holistic health approaches.
Introduction to Vitamin D Deficiency, Gum Disease, and Diabetes Risk
Vitamin D deficiency, gum disease, and diabetes are increasingly recognized as interconnected health concerns. Emerging research suggests a complex interplay between these conditions, potentially impacting the development and progression of each. Understanding the potential links between these conditions is crucial for preventive strategies and personalized healthcare approaches.The scientific community is actively investigating the mechanisms by which these conditions might influence each other.
This exploration is vital for creating targeted interventions and improving public health outcomes. This article delves into the potential relationship between vitamin D deficiency, gum disease, and diabetes risk, providing an overview of the current scientific understanding and potential mechanisms involved.
Potential Link Between Vitamin D Deficiency, Gum Disease, and Diabetes Risk
Research indicates a potential link between vitamin D deficiency, gum disease, and an increased risk of diabetes. This connection isn’t fully understood, but various mechanisms are being explored. For example, vitamin D plays a role in regulating blood sugar levels, and impaired gum health may lead to increased inflammation and insulin resistance. These factors could potentially contribute to a higher risk of developing diabetes.
Current Scientific Understanding of the Interconnectedness
The current scientific understanding of the interconnectedness focuses on the role of inflammation. Studies suggest that chronic inflammation, a common feature of both gum disease and vitamin D deficiency, may contribute to insulin resistance and increased blood sugar levels, ultimately increasing the risk of developing diabetes. Furthermore, these inflammatory processes may create a cycle, where one condition exacerbates the others.
Potential Mechanisms Influencing Each Other
Several potential mechanisms may explain how vitamin D deficiency, gum disease, and diabetes risk influence each other. One possibility is that vitamin D deficiency impairs immune function, making individuals more susceptible to gum disease. Conversely, gum disease can increase inflammation throughout the body, potentially affecting insulin sensitivity and leading to a higher risk of diabetes. Another aspect is that these conditions may share common risk factors, such as poor diet and lack of physical activity, which further complicate the relationship.
Prevalence of Conditions in Different Populations
The prevalence of vitamin D deficiency, gum disease, and diabetes varies significantly across different populations. Factors such as geographic location, ethnicity, socioeconomic status, and lifestyle choices influence these rates. A comparison of these conditions’ prevalence across diverse groups can help target preventative strategies.
| Population Group | Vitamin D Deficiency Prevalence (%) | Gum Disease Prevalence (%) | Diabetes Prevalence (%) |
|---|---|---|---|
| African Americans in the Southern US | ~30-40 | ~30-45 | ~15-20 |
| Hispanic Americans in California | ~25-35 | ~20-30 | ~10-15 |
| Northern European populations | ~10-20 | ~10-15 | ~5-10 |
Note: Prevalence estimates are approximate and may vary depending on the specific study and methodology.
Vitamin D Deficiency and its Impact

Vitamin D, often called the “sunshine vitamin,” plays a crucial role in maintaining overall health. It’s essential for calcium absorption, bone health, and a robust immune system. However, a significant portion of the global population suffers from vitamin D deficiency, leading to a multitude of potential health consequences. This section will delve into the role of vitamin D, the implications of deficiency on oral health, and diagnostic methods.Vitamin D is vital for numerous bodily functions, acting as a hormone that regulates calcium and phosphorus levels.
Adequate vitamin D levels are critical for strong bones and teeth, supporting their growth and maintenance. Furthermore, it plays a pivotal role in the immune system, influencing the production of antimicrobial peptides and modulating immune responses. This crucial function helps the body fight off infections.
Role of Vitamin D in Overall Health
Vitamin D’s influence extends beyond bone health and immune function. It contributes to cellular growth and differentiation, impacting various tissues and organs throughout the body. Sufficient levels of vitamin D are associated with reduced risks of certain cancers, autoimmune diseases, and even mental health issues. The intricate network of vitamin D’s effects underscores its importance in maintaining optimal well-being.
Consequences of Vitamin D Deficiency on Oral Health
Vitamin D deficiency can impact oral health in several ways. It can compromise the integrity of tooth enamel, increasing susceptibility to dental caries (cavities). Furthermore, a deficiency may lead to impaired bone remodeling, affecting the supporting structures of teeth and potentially contributing to periodontal disease. These issues highlight the crucial link between systemic health, including vitamin D levels, and oral health.
Methods for Diagnosing Vitamin D Deficiency
Diagnosing vitamin D deficiency involves assessing blood levels of 25-hydroxyvitamin D, the primary circulating form of vitamin D. A blood test is the standard method for measuring vitamin D levels. The results are often expressed in nanograms per milliliter (ng/mL) or nanomoles per liter (nmol/L). Different laboratories may use slightly different reference ranges, so it’s essential to understand the specific values used by the testing facility.
Recent studies show a concerning link between a lack of vitamin D and gum disease, potentially increasing the risk of diabetes. It’s a complex interplay of factors, and like how a mask fits can be as important as what its made of how a mask fits can be as important as what its made of , different aspects of health can influence each other in unexpected ways.
Ultimately, maintaining good oral health and sufficient vitamin D levels are crucial for overall well-being and may help to reduce the risk of diabetes.
Various factors, including age, sex, and overall health, can influence the interpretation of vitamin D levels.
Symptoms and Signs of Vitamin D Deficiency
The following table Artikels common symptoms and signs associated with vitamin D deficiency. It’s important to remember that these symptoms can be subtle or overlap with other conditions. Consulting a healthcare professional is crucial for proper diagnosis and treatment.
Recent studies show a worrying link between a lack of vitamin D and gum disease, potentially increasing the risk of diabetes. It’s a complex interplay of factors, and while this research is important, access to reliable at-home HIV testing could also revolutionize preventative care for key groups, offering earlier diagnoses and improved health outcomes. This could be a game changer for those who might not otherwise access testing.
Ultimately, understanding these interconnected health risks like vitamin D deficiency and gum disease is crucial for preventative measures and better public health.
| Symptom/Sign | Description |
|---|---|
| Muscle weakness | Generalized muscle pain, tenderness, or difficulty with movement. |
| Bone pain | Pain in the bones, particularly in the legs, hips, and back. |
| Fatigue | Persistent tiredness and lack of energy. |
| Increased risk of infections | Frequent or prolonged illnesses, including respiratory infections. |
| Mood changes | Depression, irritability, or anxiety. |
| Hair loss | Thinning or loss of hair. |
Gum Disease and its Impact
Gum disease, also known as periodontal disease, is a common oral health problem that affects the tissues surrounding the teeth. It’s a progressive condition that, if left untreated, can lead to significant damage to the gums, teeth, and even other parts of the body. Understanding the causes, progression, and potential systemic effects of gum disease is crucial for maintaining overall health.Gum disease isn’t simply a problem confined to the mouth.
Chronic inflammation, a key component of gum disease, can have far-reaching consequences throughout the body. This inflammation, if sustained, can contribute to various systemic health issues, increasing the risk of complications beyond the oral cavity.
Causes and Progression of Gum Disease
Plaque, a sticky film of bacteria, is the primary culprit in the development of gum disease. When plaque isn’t removed through proper oral hygiene, it hardens into tartar (calculus), which irritates the gums. This irritation triggers an inflammatory response, leading to gingivitis, the initial stage of gum disease. If gingivitis isn’t treated, it can progress to periodontitis, a more severe form characterized by the destruction of the supporting tissues that hold teeth in place.
The progression of periodontitis is often gradual and can go unnoticed until significant damage has occurred. Factors like poor oral hygiene, genetics, certain medical conditions, and smoking significantly contribute to the progression of gum disease.
Role of Inflammation in Gum Disease
Inflammation is a crucial aspect of gum disease. The body’s immune response to bacterial plaque leads to the accumulation of inflammatory cells and substances. This chronic inflammation, if unchecked, can extend beyond the gums and potentially affect other parts of the body. The inflammatory mediators released during gum disease can enter the bloodstream, potentially contributing to systemic inflammation, a risk factor for various health problems.
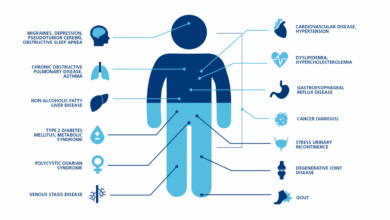
Systemic Effects of Gum Disease, Lack of vitamin d and gum disease higher diabetes risk
The inflammatory response associated with gum disease isn’t confined to the mouth. Chronic inflammation has been linked to an increased risk of several systemic conditions. Research suggests a correlation between gum disease and cardiovascular disease, as inflammation can contribute to atherosclerosis, the buildup of plaque in the arteries. Additionally, studies indicate a possible connection between gum disease and diabetes, respiratory diseases, and certain types of cancer.
These potential links highlight the importance of managing gum disease for overall health.
Relationship with Cardiovascular Disease and Other Health Issues
The connection between gum disease and cardiovascular disease is gaining increasing recognition. Chronic inflammation associated with gum disease can contribute to the development of atherosclerosis. This process involves the buildup of plaque in the arteries, potentially leading to heart attacks and strokes. Moreover, gum disease has been linked to other health issues such as respiratory illnesses, diabetes complications, and some types of cancer.
Comparison of Gum Disease Types
| Type of Gum Disease | Symptoms |
|---|---|
| Gingivitis | Inflammation and redness of the gums, bleeding gums during brushing or flossing, swollen gums, bad breath. |
| Periodontitis | Swollen, tender, and bleeding gums, receding gums, loose teeth, formation of pockets around teeth, pus, bad breath, and pain. |
Note: Symptoms can vary in severity and presentation. Consult a dentist for proper diagnosis and treatment.
Diabetes and its Impact
Diabetes, a chronic metabolic disorder, significantly impacts various bodily functions. It’s characterized by elevated blood glucose levels, stemming from insufficient insulin production or impaired insulin action. This disruption in glucose regulation has widespread consequences throughout the body, impacting everything from energy production to nerve function. Understanding the mechanisms of diabetes and its ramifications is crucial for effective management and prevention.Diabetes arises from a complex interplay of genetic predisposition and environmental factors.
Factors like diet, lifestyle, and certain medical conditions contribute to the development of the disease. The body’s inability to properly utilize or produce insulin leads to a buildup of glucose in the bloodstream. This persistent hyperglycemia, if left unchecked, sets off a cascade of harmful effects on numerous bodily systems.
Mechanisms of Diabetes and Impact on Bodily Functions
Diabetes affects virtually every organ and tissue in the body. Elevated blood glucose damages blood vessels, increasing the risk of cardiovascular disease, stroke, and kidney disease. The damage extends to nerves, leading to neuropathy, a condition causing pain, numbness, and tingling, particularly in the extremities. Chronic high blood sugar can also impair vision, potentially causing retinopathy and even blindness.
Link Between Diabetes and Inflammation
A crucial aspect of diabetes’s impact is the significant role of inflammation. Persistent hyperglycemia triggers a chronic inflammatory response throughout the body. This inflammation contributes to the development and progression of various diabetes-related complications, including cardiovascular disease, neuropathy, and nephropathy. The inflammatory process damages blood vessels, exacerbates nerve damage, and impairs kidney function. Studies have shown a strong correlation between inflammatory markers and the severity of diabetes-related complications.
Potential Effects of Diabetes on Oral Health
Diabetes significantly impacts oral health, increasing the risk of various dental problems. High blood sugar levels weaken the immune system, making individuals more susceptible to oral infections. The increased inflammation associated with diabetes can also lead to gum disease, gingivitis, and periodontitis. Delayed wound healing and impaired immune response exacerbate the problem. This increased susceptibility to oral infections can lead to tooth loss and other severe complications.
Recent studies show a concerning link between a lack of vitamin D and gum disease, increasing the risk of diabetes. Meanwhile, a new swine flu has been discovered in pigs in China, raising concerns about potential global health impacts. While the swine flu situation is certainly worrying, it’s crucial to remember that maintaining good oral hygiene and sufficient vitamin D levels can significantly reduce the risk of diabetes and other related health issues.
Types of Diabetes and Associated Risk Factors
Understanding the different types of diabetes and their respective risk factors is crucial for preventative measures and personalized management strategies. The following table Artikels the common types and their associated risk factors:
| Type of Diabetes | Description | Risk Factors |
|---|---|---|
| Type 1 Diabetes | An autoimmune disease where the body’s immune system attacks and destroys the insulin-producing cells in the pancreas. | Genetic predisposition, certain environmental factors, and possible viral infections. |
| Type 2 Diabetes | A condition characterized by insulin resistance, where the body’s cells do not respond effectively to insulin. Over time, the pancreas may also lose its ability to produce enough insulin. | Obesity, family history of diabetes, physical inactivity, unhealthy diet, age (over 45), ethnicity (certain groups), and gestational history. |
| Gestational Diabetes | A form of diabetes that develops during pregnancy. | Genetic predisposition, family history of diabetes, ethnicity (certain groups), obesity, advanced maternal age, previous history of gestational diabetes, and certain medical conditions. |
Interconnectedness of Vitamin D, Gum Disease, and Diabetes: Lack Of Vitamin D And Gum Disease Higher Diabetes Risk
The complex interplay between vitamin D deficiency, gum disease, and an increased risk of diabetes is a growing area of research. These three conditions, seemingly disparate, share common threads, particularly concerning inflammation and the gut microbiome. Understanding these connections could pave the way for more targeted preventative strategies and interventions.The link between these conditions isn’t straightforward, but there are compelling reasons to believe they are intertwined.
Inflammation plays a pivotal role in the development and progression of all three. Disruptions in the gut microbiome, often triggered by poor dietary habits and chronic inflammation, might also be a common factor. Further research is crucial to fully understand these interactions.
Potential Common Pathways
Multiple interconnected pathways might explain the increased risk of diabetes in individuals with vitamin D deficiency and gum disease. These conditions are not independent but rather parts of a larger system, where inflammation and microbial dysbiosis play a key role.
Role of Inflammation
Inflammation is a key factor in the development and progression of these conditions. Chronic low-grade inflammation is implicated in the pathogenesis of type 2 diabetes, periodontal (gum) disease, and vitamin D deficiency. This inflammatory response can disrupt metabolic processes, potentially leading to insulin resistance and impaired glucose tolerance. For example, chronic inflammation can directly affect the pancreas, reducing its ability to produce insulin, which is crucial for regulating blood sugar levels.
Gut Microbiota Interactions
The gut microbiome, the complex community of microorganisms residing in the gut, is emerging as a key player in the interconnectedness of these conditions. An imbalance in the gut microbiota, often referred to as dysbiosis, may trigger or exacerbate inflammation, leading to problems with vitamin D metabolism, immune function, and glucose regulation. The presence of certain bacteria and fungi in the gut may also contribute to the inflammatory response in the gums and other tissues.
Research Examples
Numerous studies have explored the potential links between vitamin D deficiency, gum disease, and diabetes risk. For example, a study published in the Journal of Clinical Endocrinology & Metabolism found a correlation between low vitamin D levels and a higher prevalence of periodontitis. Another study demonstrated that individuals with gum disease had a higher likelihood of developing type 2 diabetes compared to those with healthy gums.
These findings suggest a potential causal relationship, though further research is needed to establish a definitive link.
Furthermore, studies examining the gut microbiome in individuals with these conditions have shown altered microbial profiles. These changes may influence the host’s immune response and metabolic processes, contributing to the development of these conditions.
Risk Factors and Prevention
The interconnectedness of vitamin D deficiency, gum disease, and diabetes risk isn’t just a theoretical concept; it’s a tangible reality with significant implications for public health. Understanding the risk factors and proactive measures to prevent these conditions is crucial for maintaining overall well-being. This section will delve into the potential causes of these issues and explore lifestyle choices that can mitigate the risk of developing them.Recognizing the risk factors associated with these conditions allows individuals to make informed decisions about their health and take preventive measures.
Proactive steps like adopting a balanced diet, maintaining good oral hygiene, and engaging in regular physical activity can significantly reduce the likelihood of developing these conditions.
Potential Risk Factors
Several factors can increase an individual’s susceptibility to vitamin D deficiency, gum disease, and diabetes. Age, genetics, and certain medical conditions play a role. For example, older adults often have reduced vitamin D production due to decreased sun exposure and changes in metabolism. Genetic predispositions to these conditions also exist, although lifestyle choices can significantly influence the manifestation of these risks.
Lifestyle Choices for Risk Reduction
Adopting healthy lifestyle choices is crucial in minimizing the risk of developing these conditions. A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients for overall health, including vitamin D. Regular physical activity improves insulin sensitivity, which is critical in managing blood sugar levels.
- Dietary Choices: A diet rich in fruits, vegetables, and whole grains is essential. These foods provide essential nutrients and fiber, supporting overall health and well-being. Limiting processed foods, sugary drinks, and excessive saturated fats is equally important for maintaining a healthy weight and reducing inflammation, which can contribute to various health issues.
- Sun Exposure: Sunlight is crucial for vitamin D synthesis. Moderate sun exposure, without excessive tanning or burning, is beneficial. Consulting a doctor for personalized recommendations is advisable, especially for individuals with specific conditions or limited sun exposure.
- Physical Activity: Regular physical activity, such as brisk walking, jogging, or swimming, is essential for maintaining a healthy weight and improving insulin sensitivity. Physical activity helps regulate blood sugar levels and promotes overall health. Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
Importance of Oral Hygiene and Dental Checkups
Maintaining good oral hygiene and scheduling regular dental checkups are paramount for preventing gum disease. Plaque buildup, if not addressed, can lead to gingivitis and periodontitis, potentially impacting systemic health.
- Daily Oral Hygiene: Brushing and flossing twice daily are essential for removing plaque and preventing the buildup of bacteria that cause gum disease. Proper technique and using fluoride toothpaste are crucial for optimal oral health.
- Regular Dental Checkups: Regular dental checkups enable early detection and treatment of gum disease. Professional cleanings and examinations are vital for maintaining oral health and preventing potential complications. Dental professionals can provide personalized guidance on oral hygiene practices and address any concerns.
Dietary Recommendations for Vitamin D
Maintaining adequate vitamin D levels requires a balanced approach, including dietary intake and appropriate sun exposure. A diet rich in vitamin D-rich foods can supplement sun exposure.
| Food | Vitamin D Content (approximate) |
|---|---|
| Fatty Fish (salmon, tuna, mackerel) | Excellent source |
| Egg Yolks | Moderate source |
| Fortified Foods (milk, cereals, yogurt) | Often fortified |
| Mushrooms | Can contain vitamin D2 |
| Beef Liver | Good source |
Vitamin D supplementation should only be considered under the guidance of a healthcare professional.
Future Research Directions
Unraveling the intricate connections between vitamin D deficiency, gum disease, and diabetes requires further investigation. Current research suggests a strong correlation, but the underlying mechanisms remain partially understood. Future studies are crucial to confirm these links and explore potential interventions. Understanding these connections could lead to significant advancements in preventative healthcare and improved patient outcomes.
Exploring the Underlying Mechanisms
Understanding the precise biological pathways linking these three conditions is paramount. Specific research should focus on identifying the molecular interactions between vitamin D, periodontal pathogens, and insulin resistance. This involves studying the expression of key genes and proteins involved in inflammation, immune response, and metabolic processes. For example, studies could examine how vitamin D supplementation affects the inflammatory response in the gums and its impact on insulin sensitivity in individuals with pre-diabetes.
Further investigations could explore the role of specific gut microbiota in the development and progression of these conditions.
Clinical Trials and Interventions
Developing effective interventions based on the established correlations is critical. Clinical trials should rigorously evaluate the impact of vitamin D supplementation, alongside periodontal therapy, on diabetes risk factors in high-risk populations. Such trials would need to consider the dosage, duration, and specific patient populations (e.g., those with existing periodontal disease, vitamin D deficiency, and prediabetes). For instance, a trial could compare the effectiveness of different vitamin D supplementation regimens combined with scaling and root planing (SRP) in reducing HbA1c levels and preventing the progression to type 2 diabetes in individuals with both gum disease and vitamin D deficiency.
Innovative Research Approaches
Innovative research approaches are necessary to address the complexity of these interconnected conditions. Multi-center collaborative studies, integrating data from various sources, will be essential. This includes combining data from existing databases on vitamin D levels, periodontal health, and diabetes markers. For example, leveraging large-scale electronic health records (EHRs) to identify individuals at high risk of developing diabetes could allow researchers to track outcomes and assess the effectiveness of preventative interventions more effectively.
Advanced statistical modeling techniques can help analyze the complex interactions between these conditions and identify predictive factors for disease development.
Potential Areas for Future Research Studies
| Research Area | Specific Focus | Potential Impact |
|---|---|---|
| Vitamin D Receptor (VDR) Signaling Pathways | Investigate how VDR signaling affects inflammatory processes in the gums and pancreatic beta-cell function. | Identify potential targets for novel therapeutic interventions. |
| Gut Microbiota Interactions | Study the interplay between gut microbiota, vitamin D metabolism, and the development of periodontal disease and insulin resistance. | Develop targeted probiotic interventions to improve metabolic health. |
| Periodontitis and Diabetes Progression | Analyze the role of periodontal inflammation in accelerating the progression of prediabetes to type 2 diabetes. | Identify early markers for disease progression and potential interventions. |
| Personalized Interventions | Develop personalized treatment strategies based on individual genetic profiles, vitamin D levels, and periodontal status. | Optimize treatment effectiveness and minimize adverse effects. |
Last Word
In conclusion, the intricate relationship between vitamin D deficiency, gum disease, and diabetes risk warrants further investigation. The potential pathways linking these conditions, particularly the role of inflammation and the gut microbiome, suggest a complex interplay that requires more research. This article emphasizes the significance of preventative measures, including maintaining optimal vitamin D levels, practicing good oral hygiene, and adopting a healthy lifestyle.
Ultimately, understanding these connections can empower individuals to make informed choices about their health and well-being.