Long COVID can cause heart problems along with breathing difficulties, posing significant challenges for those affected. This comprehensive exploration delves into the intricacies of this condition, examining the various symptoms, potential mechanisms, and potential treatment strategies.
The discussion covers the diverse aspects of Long COVID, including its definition, prevalence, and potential long-term effects on the cardiovascular and respiratory systems. It will also examine the potential interplay between heart and lung problems, and the challenges in diagnosis and treatment.
Defining Long COVID
Long COVID, also known as post-COVID-19 syndrome, is a complex and multifaceted condition characterized by persistent symptoms that linger for weeks, months, or even years after an initial COVID-19 infection. It’s not simply a matter of the initial illness persisting; rather, it’s a distinct syndrome with its own set of characteristics, often affecting multiple organ systems. Understanding its nuances is crucial for effective diagnosis and management.
Characteristics of Long COVID
Long COVID encompasses a wide range of symptoms, often varying significantly from person to person. These symptoms can affect various bodily functions, including the respiratory, cardiovascular, neurological, and gastrointestinal systems. The persistent nature of these symptoms distinguishes it from typical post-viral syndromes. This chronic nature often leads to significant functional limitations and decreased quality of life.
Diagnostic Criteria for Long COVID
Establishing definitive diagnostic criteria for Long COVID presents significant challenges. Currently, there isn’t a single, universally accepted set of diagnostic criteria. However, several criteria are used, often relying on symptom duration, severity, and impact on daily life. The challenge lies in differentiating Long COVID from other conditions with overlapping symptoms, requiring a thorough evaluation that considers the patient’s history, physical examination, and potentially laboratory tests.
Furthermore, the absence of a specific biomarker for Long COVID complicates the diagnostic process.
Comparison with Other Conditions
Long COVID shares some similarities with other post-viral syndromes, but key distinctions exist. While some symptoms might overlap, the duration, severity, and the constellation of symptoms in Long COVID often set it apart. For example, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) has overlapping features but typically involves a more profound fatigue component. Differentiating these conditions requires a careful evaluation of the individual patient’s symptoms and medical history.
Prevalence and Demographics
Long COVID affects a significant portion of individuals who contract COVID-19. Prevalence estimates vary, depending on the study methodologies and criteria employed. Demographics associated with increased risk of developing Long COVID include individuals with underlying health conditions, such as cardiovascular disease, diabetes, and obesity.
Potential Long-Term Effects
The potential long-term effects of Long COVID are still being investigated. Studies are exploring the impact on various organ systems, including the heart, lungs, brain, and gut. The long-term effects can range from mild functional limitations to severe, chronic conditions.
Symptoms of Long COVID
Symptoms of Long COVID can manifest in diverse ways. The following table Artikels some of the common symptoms, particularly those affecting the heart and respiratory system.
| Symptom | Description | Severity | Frequency |
|---|---|---|---|
| Fatigue | Extreme tiredness and lack of energy, impacting daily activities | Mild to Severe | Very Common |
| Brain fog | Difficulty with concentration, memory, and cognitive function | Mild to Moderate | Common |
| Chest pain | Discomfort or pain in the chest, often associated with exertion | Mild to Severe | Variable |
| Shortness of breath | Difficulty breathing, even with minimal exertion | Mild to Severe | Common |
| Palpitations | Rapid or irregular heartbeats | Mild to Moderate | Variable |
| Cough | Persistent cough, sometimes dry or productive | Mild to Moderate | Common |
| Headache | Recurring headaches, often severe | Mild to Severe | Variable |
| Joint pain | Pain and stiffness in the joints | Mild to Moderate | Common |
Cardiovascular Implications of Long COVID
Long COVID, a lingering condition affecting many individuals after an initial infection, presents a complex interplay of symptoms and potential health complications. One area of significant concern is the impact on the cardiovascular system. This often manifests as a range of heart-related issues, demanding further investigation and careful management.
Potential Mechanisms of Cardiovascular Impact
The exact mechanisms by which Long COVID affects the heart remain an active area of research. Several theories attempt to explain the link. Inflammation, a hallmark of the initial infection, is thought to play a crucial role. This systemic inflammation can potentially damage the heart muscle and blood vessels, leading to various cardiovascular complications. Additionally, some researchers suggest that the body’s immune response to the virus may contribute to the development of heart problems.
The viral infection itself may also directly impact the heart’s function, although the specific pathways involved are not yet fully understood. Genetic predisposition and pre-existing conditions may also play a role in influencing the severity and presentation of these complications.
Observed Heart Problems in Long COVID
A variety of heart problems have been observed in individuals with Long COVID. These include myocarditis (inflammation of the heart muscle), pericarditis (inflammation of the outer lining of the heart), and arrhythmias (irregular heartbeats). Furthermore, there are reports of increased blood pressure, altered heart rate variability, and evidence of structural heart changes in some patients. These issues highlight the importance of careful cardiovascular monitoring for those experiencing long-term effects after COVID-19.
Symptoms of Cardiovascular Complications
Symptoms associated with cardiovascular complications in Long COVID can vary greatly. Common symptoms include chest pain, shortness of breath, palpitations, fatigue, dizziness, and swelling in the extremities. These symptoms may be subtle and easily overlooked, potentially delaying diagnosis and appropriate intervention. The severity of these symptoms can also fluctuate over time.
Evidence Supporting the Link
Studies have demonstrated a correlation between Long COVID and cardiovascular issues. Several research papers have reported increased rates of myocarditis and other heart conditions in individuals with Long COVID compared to those without. Observational studies and case reports have documented the occurrence of these complications in individuals following SARS-CoV-2 infection. The accumulating evidence suggests a plausible link, but more robust, longitudinal studies are needed to fully elucidate the nature and extent of this association.
Comparison of Heart Conditions in Long COVID vs. Non-Long COVID Patients
| Condition | Long COVID Prevalence | Non-Long COVID Prevalence | Risk Factors |
|---|---|---|---|
| Myocarditis | Potentially elevated | Generally lower | Viral infection, inflammation, pre-existing conditions |
| Pericarditis | Potentially elevated | Generally lower | Viral infection, inflammation, pre-existing conditions |
| Arrhythmias | Potentially elevated | Variable, depending on underlying factors | Inflammation, altered autonomic nervous system function, pre-existing conditions |
| Increased Blood Pressure | Potentially elevated | Variable, depending on underlying factors | Inflammation, altered vascular function, pre-existing conditions |
| Structural Heart Changes | Potentially present in some cases | Variable, depending on underlying factors | Inflammation, viral damage, pre-existing conditions |
Potential Risk Factors for Heart Problems after Long COVID
Several factors might increase the risk of developing heart problems after experiencing Long COVID. These include the severity of the initial infection, pre-existing cardiovascular conditions, a history of other health problems, and individual genetic predisposition. Furthermore, certain lifestyle factors, such as poor diet, lack of exercise, and smoking, may also contribute to the development of these complications. Understanding these risk factors is crucial for developing preventative strategies and personalized care plans.
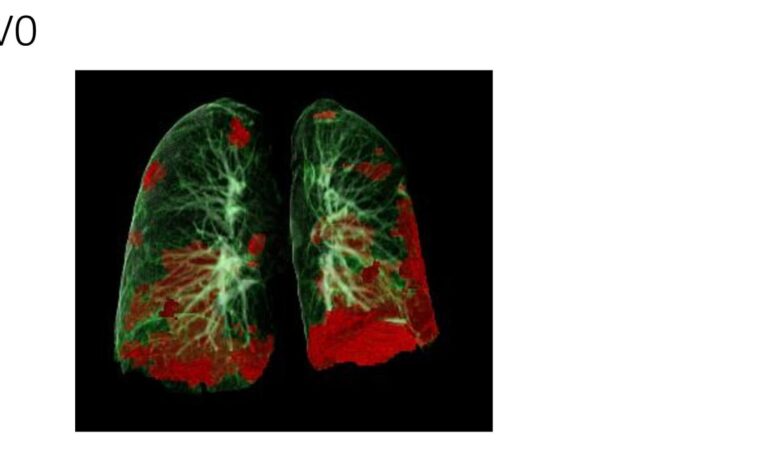
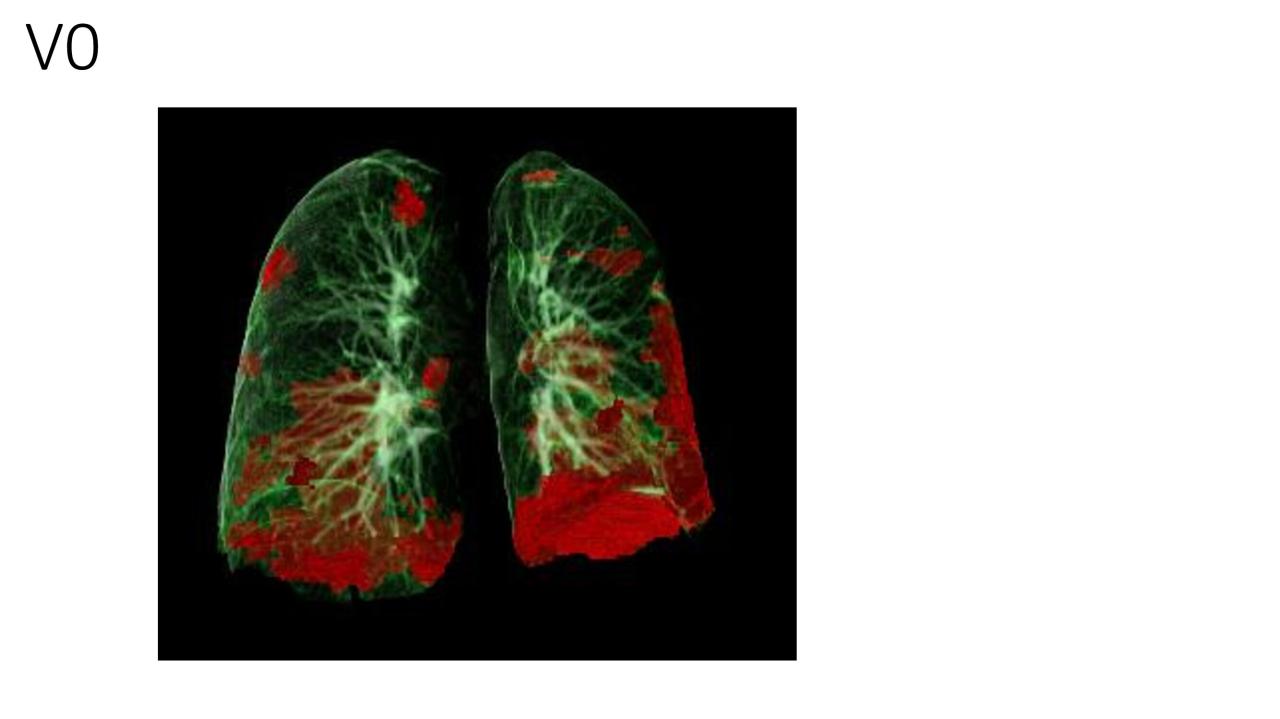
Respiratory Issues in Long COVID: Long Covid Can Cause Heart Problems Along With Breathing Difficulties
Long COVID presents a complex range of symptoms, and respiratory difficulties are a significant concern for many patients. Understanding the various respiratory problems, their underlying mechanisms, and the impact on daily life is crucial for effective management and support. This exploration delves into the respiratory challenges associated with Long COVID, highlighting the diverse experiences and the importance of personalized care.Respiratory issues in Long COVID manifest in a multitude of ways, impacting the ability to breathe comfortably and efficiently.
These difficulties can stem from a variety of underlying mechanisms, including inflammation, damage to lung tissue, and altered function of the respiratory system. The severity and duration of these symptoms can vary greatly, requiring tailored approaches to treatment and management.
Types of Respiratory Problems
Respiratory problems in Long COVID patients are diverse and can significantly affect daily life. This section Artikels the common respiratory issues, emphasizing the spectrum of severity and potential treatment strategies.
Long COVID can really mess with your respiratory system, causing breathing difficulties and, unfortunately, heart problems too. It’s a sobering reminder that taking care of your heart health starts young, and habits like drinking and smoking when young can prematurely age your heart, potentially leading to similar issues later on. So, while Long COVID highlights the fragility of our cardiovascular system, it also emphasizes the importance of proactive healthy habits for a long, healthy life.
- Dyspnea (shortness of breath): This is a common complaint, characterized by an uncomfortable sensation of needing to breathe more than usual. Dyspnea can vary in intensity, from mild to severe, impacting activities such as walking, climbing stairs, or even simple conversations. The intensity can fluctuate throughout the day and even with the slightest exertion.
- Cough: A persistent cough, often dry or productive of mucus, is another frequent symptom. This cough can persist for months or even years after the initial COVID-19 infection. The cough can be debilitating, disrupting sleep and overall well-being. Some individuals may experience a chronic cough that does not respond to conventional treatments.
- Chest tightness and pain: Many Long COVID patients report chest tightness or pain, which can be associated with breathing difficulties. This sensation can range from a mild discomfort to a severe, constricting feeling, making it challenging to breathe deeply. This symptom can mimic other conditions, necessitating a thorough evaluation to differentiate it from other underlying causes.
- Wheezing and Bronchospasm: Wheezing, a whistling sound during breathing, and bronchospasm, a tightening of the airways, are also observed in some individuals with Long COVID. These symptoms often worsen with exertion or exposure to triggers such as allergens. The symptoms can resemble those of asthma, highlighting the need for careful diagnosis and management.
Mechanisms Contributing to Breathing Difficulties
The exact mechanisms behind respiratory issues in Long COVID are still under investigation, but several factors are suspected. These include persistent inflammation in the lungs, damage to the alveoli (air sacs), and altered immune responses.
“Ongoing inflammation and immune dysregulation could contribute to the chronic respiratory symptoms observed in Long COVID patients.”
Severity and Duration of Symptoms
The severity and duration of respiratory symptoms in Long COVID vary considerably. Some patients experience mild symptoms that resolve within a few months, while others experience persistent and severe symptoms that significantly impact their quality of life. The duration of symptoms can extend for years after the initial infection, making it challenging to predict long-term outcomes.
Impact on Daily Life and Quality of Life
Respiratory issues in Long COVID can significantly impact daily life and quality of life. Activities that were once routine, such as walking, climbing stairs, or even simple conversations, can become challenging or impossible due to breathlessness and fatigue. This can lead to social isolation, decreased participation in social activities, and a decline in overall well-being.
Examples of Breathing Difficulties, Long covid can cause heart problems along with breathing difficulties
- Post-exertional malaise (PEM): This describes a symptom where significant exertion leads to a worsening of respiratory symptoms, including dyspnea, fatigue, and muscle aches.
“PEM is a key symptom to consider when assessing respiratory issues in Long COVID patients.”
- Exercise-induced breathlessness: Difficulty breathing after physical activity, even mild activity, is common. This can range from mild shortness of breath to severe gasping.
Comparison with Other Respiratory Illnesses
| Symptom | Long COVID Description | Other Respiratory Illness Description | Treatment Options |
|---|---|---|---|
| Cough | Persistent, dry or productive, lasting months to years | Can be acute or chronic, associated with various respiratory conditions | Symptomatic relief, addressing underlying causes |
| Dyspnea | Variable intensity, worsened by exertion | Shortness of breath can vary depending on the cause | Supplemental oxygen, pulmonary rehabilitation |
| Chest Tightness | Can mimic other conditions; may worsen with exertion | May be present in various conditions, including asthma and anxiety | Addressing underlying causes, medications, relaxation techniques |
| Wheezing | Can be intermittent, triggered by exertion or triggers | May be a symptom of asthma or other airway conditions | Bronchodilators, inhalers, allergy management |
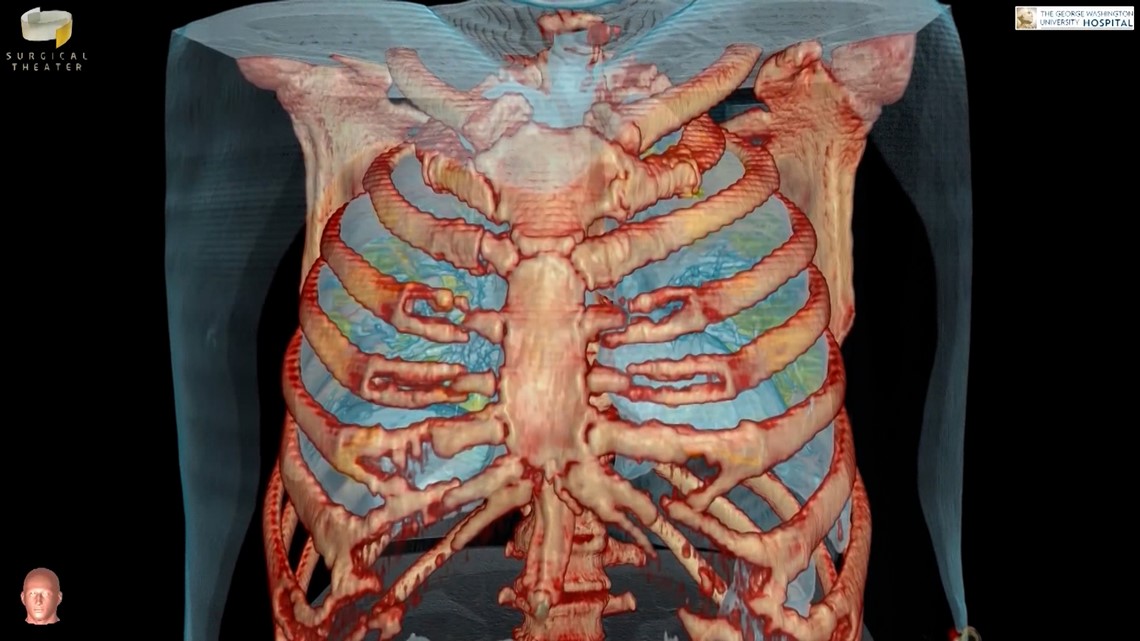
Interrelation of Heart and Lung Problems in Long COVID
Long COVID’s impact extends beyond the initial infection, often manifesting in lingering cardiovascular and respiratory issues. This complex interplay between heart and lung problems can significantly complicate diagnosis and treatment, demanding a nuanced understanding of the shared symptoms and potential mechanisms. Understanding these interrelations is crucial for developing effective management strategies and improving long-term health outcomes for affected individuals.The cardiovascular and respiratory systems are intricately connected.
Disruptions in one system can cascade into the other, creating a complex web of symptoms and complications. In Long COVID, this interconnectedness is particularly apparent, as individuals often experience overlapping symptoms affecting both the heart and lungs. This can lead to challenges in accurately identifying the primary source of the problem and implementing targeted interventions.
Potential Interplay of Cardiovascular and Respiratory Problems
The intricate relationship between the heart and lungs is fundamental to human physiology. Oxygenated blood is pumped by the heart to the lungs, where it releases carbon dioxide and picks up oxygen. Disruptions in either organ can lead to a cascade of effects on the other. In Long COVID, this intricate relationship is often disrupted, leading to a complex interplay between cardiovascular and respiratory problems.
This interplay can manifest in various ways, including shared symptoms, overlapping conditions, and distinct but related pathological processes.
Shared Symptoms and Overlapping Conditions
Patients with Long COVID may experience a range of symptoms affecting both the heart and lungs, leading to diagnostic challenges. Symptoms such as fatigue, shortness of breath, chest pain, palpitations, and dizziness can be indicative of both cardiovascular and respiratory issues. Furthermore, some conditions, like myocarditis (inflammation of the heart muscle) and pulmonary fibrosis (scarring of lung tissue), can co-occur in Long COVID patients, making accurate diagnosis and treatment even more intricate.
Examples of Co-occurring Heart and Lung Problems in Long COVID
| Patient Case | Cardiovascular Problems | Respiratory Problems | Key Characteristics |
|---|---|---|---|
| Patient A | Myocarditis, elevated cardiac biomarkers | Chronic cough, dyspnea (shortness of breath) | Experienced significant exertion intolerance. Symptoms worsened with physical activity. |
| Patient B | Atrial fibrillation, tachycardia | Bronchitis, reduced lung capacity | Presented with persistent chest discomfort and irregular heartbeat, along with recurring respiratory infections. |
| Patient C | Dilated cardiomyopathy, reduced ejection fraction | Interstitial lung disease, impaired gas exchange | Showed progressive heart weakening alongside gradual deterioration of lung function, requiring frequent hospitalizations. |
Impact on Long-Term Health Outcomes
The co-occurrence of heart and lung problems in Long COVID can significantly impact long-term health outcomes. Patients may experience reduced quality of life, increased risk of future cardiovascular events (like heart attacks or strokes), and impaired ability to perform daily activities. This combination of issues can also lead to increased healthcare costs and the need for ongoing management.
Long COVID can really mess with your body, impacting everything from breathing to heart health. Imagine a future where a wearable sensor, like a wearable sensor that measures glucose alcohol could it become a reality , could potentially monitor these kinds of issues. This kind of technology could give us a real-time insight into how our bodies are responding to illnesses like long COVID, potentially helping doctors better manage symptoms and improve patient outcomes.
Still, more research is needed to fully understand the long-term effects of long COVID and develop effective treatments.
Potential Mechanisms Linking Heart and Lung Problems
Several potential mechanisms may link heart and lung problems in Long COVID. These include:
- Immune-mediated inflammation: The immune system’s response to the initial infection may trigger widespread inflammation, impacting both the heart and lungs.
- Microvascular dysfunction: Damage to the tiny blood vessels in both organs can impair blood flow and oxygen delivery.
- Oxidative stress: Increased oxidative stress can contribute to cellular damage in both the heart and lungs.
- Viral persistence: Possible persistence of the virus within the tissues may contribute to ongoing inflammation and damage.
Severity Variations Based on Individual Factors
The severity of heart and lung problems in Long COVID varies considerably among individuals. Factors like age, pre-existing health conditions, severity of initial infection, and individual immune responses can influence the degree of organ involvement. This variability highlights the need for personalized approaches to diagnosis and management.
Long COVID can really mess with your health, causing heart problems and breathing difficulties. It’s a serious concern, and while initiatives like Kaiser Permanente building health hubs instead of traditional hospitals kaiser building hubs instead of hospitals could potentially improve access to care, the underlying issue of long COVID’s impact on the heart and lungs remains a critical challenge for patients.
Potential Treatment Strategies
Navigating the complex landscape of Long COVID, especially when heart and lung function are compromised, requires a multifaceted approach. Effective treatment strategies must address the underlying inflammatory processes, manage symptoms, and support overall well-being. This requires a personalized approach, considering individual patient needs and the unique interplay of heart and lung complications.Currently, there’s no single “cure” for Long COVID, and the search for effective treatments is an active area of research.
Therapeutic options are often tailored to specific symptoms and complications, acknowledging the heterogeneity of the condition. Finding the right combination of interventions is crucial for improving quality of life for those affected.
Therapeutic Strategies for Cardiovascular Issues
Addressing cardiovascular complications arising from Long COVID involves a combination of pharmacological and non-pharmacological interventions. These approaches aim to mitigate the effects of inflammation, improve blood flow, and reduce the risk of further complications. For example, anti-inflammatory medications, such as certain types of corticosteroids, may play a role in reducing inflammation. However, their use must be carefully evaluated due to potential side effects.
Therapeutic Strategies for Respiratory Issues
Managing respiratory symptoms in Long COVID often involves a combination of supportive therapies and medications. These strategies aim to improve lung function, reduce inflammation, and enhance overall respiratory capacity. Pulmonary rehabilitation programs, which combine exercise, education, and counseling, can significantly benefit individuals experiencing respiratory challenges. In addition, bronchodilators and other medications may be prescribed to help open airways and improve breathing.
Challenges in Developing Effective Treatments
Developing effective treatments for Long COVID-related heart and lung problems presents significant challenges. The heterogeneity of the condition, with varying symptom presentations and underlying mechanisms, makes it difficult to design targeted therapies. Furthermore, the lack of clear diagnostic markers for Long COVID complicates the selection of appropriate treatments. Longitudinal studies are essential to understand the long-term effects of these interventions.
Comparison with Existing Treatments for Similar Conditions
Treatments for Long COVID-related heart and lung issues are often inspired by existing treatments for similar conditions, such as chronic heart failure or chronic obstructive pulmonary disease (COPD). While some therapies show promise, they need to be adapted and further investigated to ensure safety and efficacy in the Long COVID context. For instance, therapies targeting inflammation and oxidative stress, common in both Long COVID and other chronic conditions, are being explored.
Role of Supportive Care
Supportive care plays a vital role in managing Long COVID symptoms, particularly when dealing with both heart and lung complications. This includes psychological support, lifestyle modifications, and patient education. Addressing the emotional and psychological toll of chronic illness is essential. Nutrition plays a crucial role in overall health and should be carefully considered to support energy levels and well-being.
Potential Treatment Options Table
| Treatment Type | Description | Potential Benefits | Potential Side Effects |
|---|---|---|---|
| Anti-inflammatory Medications (e.g., corticosteroids) | Reduce inflammation throughout the body. | May help alleviate some symptoms and reduce inflammation. | Potential for increased risk of infections, high blood pressure, and stomach ulcers. |
| Pulmonary Rehabilitation | Structured program combining exercise, education, and counseling. | Improves lung function, reduces symptoms, and improves quality of life. | Requires commitment and adherence to the program. |
| Bronchodilators | Medications that help open airways. | Improve breathing and reduce shortness of breath. | Potential for side effects such as tremors, palpitations, and anxiety. |
| Lifestyle Modifications (e.g., Diet, Exercise) | Changes in diet and exercise routines. | Supports overall health and reduces symptoms. | Requires consistent effort and commitment to change. |
Final Review
In conclusion, Long COVID’s impact on the heart and lungs is a serious concern requiring further research and improved treatment options. Understanding the multifaceted nature of these complications is crucial for providing comprehensive care to those experiencing these lingering symptoms. The interplay between cardiovascular and respiratory issues adds another layer of complexity to the management of Long COVID.
