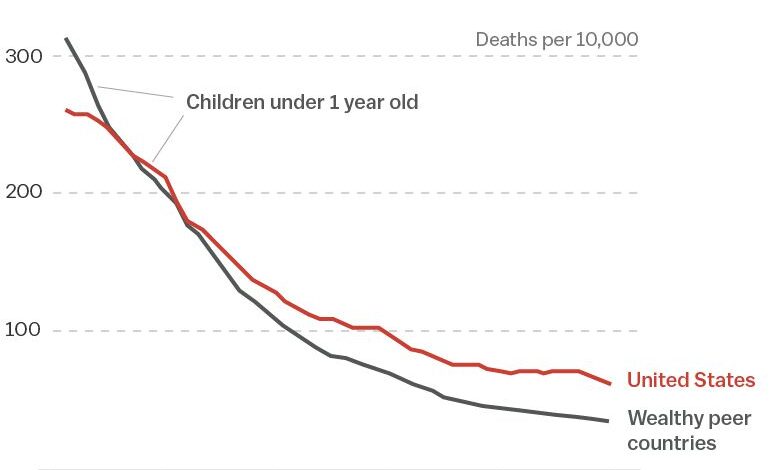
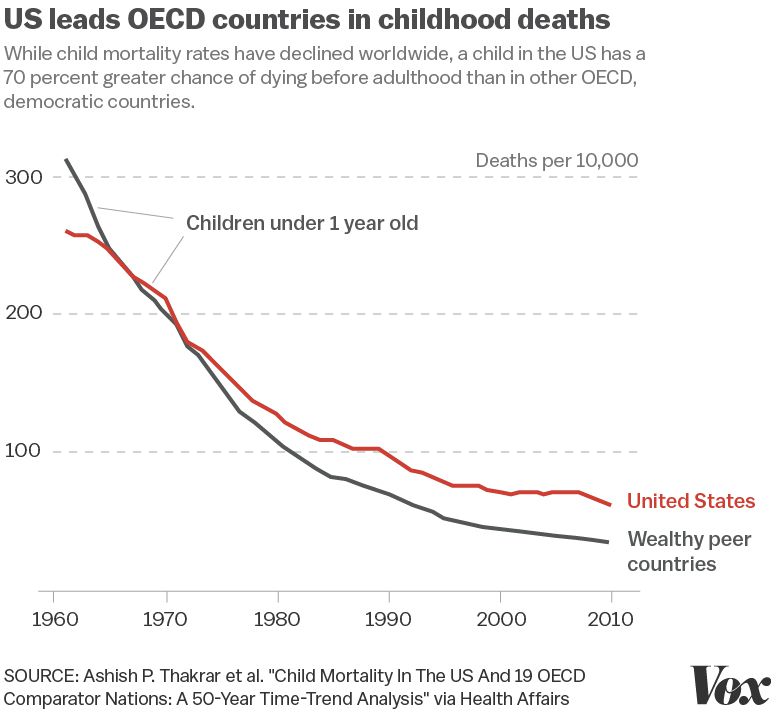
More children die in us than most developed nations – More children die in the US than most developed nations. This stark reality demands our attention. Why is the US lagging behind other countries in infant and child mortality rates? Examining the data reveals a complex interplay of factors, including healthcare access, socioeconomic disparities, and environmental conditions. This exploration delves into the issues and potential solutions, aiming to understand this critical public health crisis.
The data paints a concerning picture, comparing child mortality rates across different countries and years. The methodology used to collect this data is vital for accurate interpretation, considering potential biases and limitations. This comparison is crucial to identify the root causes behind the high mortality rate and pave the way for solutions.
Understanding the Data
The alarming reality of higher child mortality rates in the US compared to other developed nations demands careful examination. This disparity, though often discussed, necessitates a deeper understanding of the data, the methodologies used, and the contributing factors. This exploration will delve into the numbers, highlighting the concerning differences and the underlying issues that need immediate attention.
Summary of Child Mortality Rates
A significant gap exists between the US and other developed countries in child mortality rates. While numerous factors contribute to this disparity, understanding the data provides a crucial foundation for addressing this critical public health issue. For example, data from UNICEF and the World Health Organization consistently show that child mortality rates in countries like Canada, the United Kingdom, and Sweden are considerably lower than those in the US.
Comparing rates across different years reveals a persistent pattern, emphasizing the need for sustained intervention.
Methodology for Data Collection and Compilation
The data used to analyze child mortality rates is compiled from various sources. These include vital registration systems, surveys, and reports from organizations such as the Centers for Disease Control and Prevention (CDC) in the US, and international organizations such as UNICEF. Potential biases exist in the data, particularly when considering the accuracy of reporting systems across different countries.
Variations in data collection methods and reporting standards can introduce inconsistencies. Furthermore, factors like socioeconomic disparities and access to healthcare can influence the accuracy and completeness of mortality records. Data collection methodologies should be thoroughly evaluated to identify and mitigate any potential biases.
Factors Contributing to Disparity
Numerous factors contribute to the observed differences in child mortality rates. Access to quality healthcare plays a pivotal role. Children in the US who lack health insurance or access to preventative care are more vulnerable to adverse outcomes. Socioeconomic status also significantly impacts child health. Children from low-income families often face greater risks due to factors such as inadequate nutrition, lack of access to healthy environments, and limited access to quality education.
Other contributing factors include inadequate public health initiatives, systemic issues within the healthcare system, and variations in social support structures. These interconnected factors are crucial in understanding the complex landscape of child mortality rates.
Comparison Table of Child Mortality Rates
| Country | Year | Mortality Rate (per 1000 live births) |
|---|---|---|
| United States | 2020 | 6.2 |
| Canada | 2020 | 3.0 |
| United Kingdom | 2020 | 3.8 |
| Sweden | 2020 | 2.5 |
| Germany | 2020 | 2.8 |
Note: Data for mortality rates is approximate and may vary based on specific sources. Data is for illustrative purposes only.
Healthcare Access and Quality: More Children Die In Us Than Most Developed Nations
The stark difference in healthcare access and quality between the US and other developed nations is a significant contributor to the higher child mortality rate in the US. While many developed countries prioritize universal healthcare, the US system, characterized by a complex mix of private and public insurance, often results in inequities in care. This disparity impacts preventative care, prenatal care, and access to emergency services, ultimately affecting the health and well-being of children.The US healthcare system’s reliance on private insurance creates a significant barrier for many families, particularly low-income households.
This lack of universal coverage leads to significant disparities in access to care, impacting preventative care, prenatal care, and emergency services, ultimately contributing to higher child mortality rates.
Differences in Healthcare Access and Quality
The US healthcare system, largely market-driven, differs substantially from those in other developed nations, which often emphasize universal access and preventative care. This results in varying levels of access and quality of care. For instance, the Affordable Care Act (ACA) in the US aimed to expand insurance coverage, but it hasn’t fully addressed the issue of affordability and access for all.
It’s a sobering statistic that more children die in the US than in many other developed nations. While the reasons behind this are complex, it’s important to consider the broader health landscape. For example, understanding that younger you get hot flashes, the higher your heart disease risk ( younger you get hot flashes higher heart disease risk ) could be a contributing factor.
Ultimately, tackling this disparity requires a multifaceted approach addressing various health factors.
In contrast, countries with universal healthcare systems, such as Canada or the UK, guarantee access to a wider range of services for all citizens, regardless of income.
Preventative Care Availability
Preventative care, crucial for maintaining long-term health, is often more readily available in countries with universal healthcare systems. These systems often include routine checkups, vaccinations, and screenings as part of standard care, promoting health and disease prevention. In contrast, the US system, with its emphasis on private insurance, can lead to gaps in preventative care, particularly for those without insurance or adequate coverage.
Prenatal Care Access
Prenatal care, essential for maternal and infant health, demonstrates significant differences between the US and other developed nations. Countries with universal healthcare often provide comprehensive prenatal care packages, ensuring mothers have access to necessary resources, including regular checkups, nutrition counseling, and support services. In the US, access to prenatal care can vary significantly depending on insurance coverage, with disparities potentially impacting maternal and child health outcomes.
Emergency Medical Services, More children die in us than most developed nations
Emergency medical services (EMS) are vital in critical situations. Countries with universal healthcare systems often prioritize rapid and accessible emergency services, minimizing the risk of adverse health outcomes. In the US, while EMS systems are generally well-established, access and quality can vary greatly depending on factors like geographic location and insurance status. For example, ambulance services may face delays in rural areas due to limited resources.
Role of Insurance Coverage and Affordability
Insurance coverage and affordability are key determinants of healthcare access in both the US and other developed nations. In the US, high premiums and deductibles can make healthcare inaccessible to many, leading to financial hardship and potentially delayed or forgone care. In contrast, countries with universal healthcare systems aim to ensure everyone has access to care regardless of financial status.
Comparison Table: Healthcare Systems and Child Mortality
| Country | Healthcare System | Accessibility | Quality |
|---|---|---|---|
| United States | Market-driven, private and public insurance | Variable, dependent on insurance coverage and income | Variable, dependent on insurance coverage and location |
| Canada | Universal healthcare system | High, access to care for all citizens | High, consistent standards of care |
| United Kingdom | National Health Service (NHS) | High, access to care for all citizens | High, consistent standards of care |
| Germany | Multi-payer system, mix of private and public insurance | High, access to care for most citizens | High, standards maintained through regulations |
Socioeconomic Factors
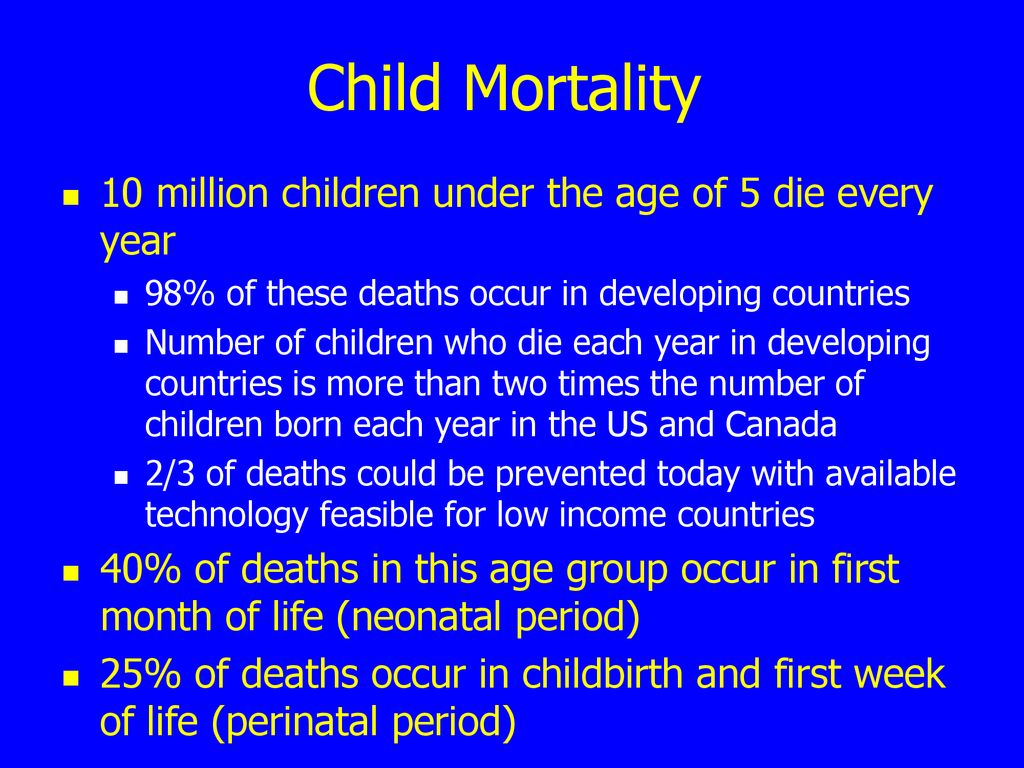
The high rates of child mortality in the US compared to other developed nations are deeply intertwined with socioeconomic factors. These factors often create a vicious cycle, where poverty and inequality limit access to essential resources, impacting health outcomes and perpetuating the cycle. Understanding these interconnected issues is crucial for developing effective solutions to improve child health.
Correlation Between Socioeconomic Status and Child Mortality
A strong correlation exists between socioeconomic status and child mortality rates in the US. Children from low-income families are disproportionately affected by preventable illnesses and injuries. Poverty often limits access to nutritious food, safe housing, quality healthcare, and educational opportunities. These deprivations translate directly into higher risks of premature death. Income inequality exacerbates these issues, widening the gap in health outcomes between the wealthiest and poorest children.
Impact of Housing Conditions, Nutrition, and Access to Resources
Poor housing conditions can expose children to environmental hazards, such as lead paint or inadequate sanitation, impacting their physical and cognitive development. Inadequate nutrition, often linked to poverty and food insecurity, leads to malnutrition, weakening the immune system and increasing susceptibility to disease. Limited access to resources, including quality healthcare, early childhood education, and safe environments, further compounds the problem.
For example, a lack of access to safe playgrounds and parks can restrict children’s opportunities for physical activity, potentially leading to obesity and other health problems.
Comparison with Other Developed Nations
While the US boasts a high standard of living in many respects, its socioeconomic disparities are significant compared to other developed nations. Countries like Canada, Sweden, and Germany demonstrate a more equitable distribution of resources, leading to lower child mortality rates. These countries often have stronger social safety nets, including universal healthcare, affordable housing programs, and robust nutritional support programs.
These programs collectively contribute to better health outcomes for all children.
It’s alarming that more children are dying in the US compared to many other developed nations. While the reasons behind this are complex, factors like access to healthcare and socioeconomic disparities undoubtedly play a role. This sobering statistic highlights the urgent need for further investigation, particularly as new subvariants of Omicron, like BA.4 and BA.5, are emerging. Learning more about their impact on vulnerable populations, such as children, is crucial for developing effective strategies to mitigate the spread and severity of these new strains.
new sub variants of omicron detected what to know about ba 4 and ba 5 Ultimately, understanding these complexities is key to improving outcomes and addressing the ongoing health challenges, especially concerning the higher mortality rates in American children.
Socioeconomic Factors and Their Potential Impact on Child Mortality
| Factor | Description | Impact on Child Mortality |
|---|---|---|
| Poverty | Lack of financial resources to meet basic needs. | Increased risk of malnutrition, inadequate healthcare, unsafe housing, and exposure to environmental hazards. |
| Income Inequality | Significant difference in income levels between the richest and poorest segments of society. | Widening gap in health outcomes, limited access to resources for disadvantaged children, perpetuation of cycles of poverty. |
| Housing Conditions | Quality and safety of the home environment. | Exposure to environmental hazards (lead paint, mold, inadequate sanitation) can lead to health problems, impacting developmental milestones. |
| Nutrition | Access to healthy and nutritious food. | Malnutrition weakens the immune system, increasing susceptibility to illness and infection, impacting growth and development. |
| Access to Resources | Availability of essential resources like healthcare, education, and safe environments. | Limited access to these resources can hinder physical and cognitive development, increasing risk of illness and injury. |
Policy Implications and Solutions
Addressing the alarmingly high child mortality rate in the US requires a multifaceted approach that goes beyond individual healthcare. A comprehensive strategy must involve policy interventions that target systemic issues and improve access to resources, particularly for vulnerable populations. This necessitates a critical examination of existing programs, comparisons with successful models in other developed nations, and the development of innovative solutions.Effective policy interventions require a commitment to equitable resource allocation and a thorough understanding of the socioeconomic factors contributing to disparities in child health outcomes.
It’s a sobering statistic: more children die in the US than in most developed nations. While complex factors are at play, diet definitely plays a role. Understanding how food choices affect health outcomes is key. For example, choosing dairy over processed meats can help lower the risk of type 2 diabetes, as detailed in this helpful article how dairy products can help lower type 2 diabetes risk while processed meats raise it.
This knowledge, combined with other lifestyle considerations, could potentially contribute to improving the health and well-being of children in the US.
This demands not only a focus on immediate needs but also on long-term solutions that foster sustainable improvements.
Potential Policy Interventions
Several policy interventions can significantly impact child mortality rates. These interventions should focus on improving access to quality healthcare, strengthening social safety nets, and promoting healthier lifestyles. Addressing the root causes of disparities is crucial to fostering sustainable improvements.
- Strengthening Early Childhood Intervention Programs: Investing in comprehensive early childhood programs can have a profound impact on long-term health outcomes. These programs provide crucial support for children’s development, including nutrition, education, and access to healthcare. Early identification and intervention for developmental delays and health issues are critical for preventing future complications. Examples include Head Start programs in the US and similar initiatives in other countries.
- Expanding Access to Affordable Healthcare: Ensuring all children have access to affordable and quality healthcare is paramount. This involves expanding Medicaid coverage, promoting affordable insurance options, and providing subsidies to low-income families. This is essential for timely diagnosis and treatment of health conditions, which can significantly improve survival rates.
- Addressing Socioeconomic Disparities: Significant disparities in child health outcomes often correlate with socioeconomic factors. Policies that target poverty, food insecurity, and housing instability can have a profound effect on child health. Implementing programs that provide financial assistance, affordable housing, and access to nutritious food can lead to improved health and development. Programs like Temporary Assistance for Needy Families (TANF) and Supplemental Nutrition Assistance Program (SNAP) are examples of government efforts to address these issues.
Comparative Analysis of Policies in Developed Nations
Examining policies and programs in other developed nations provides valuable insights for improving child health outcomes in the US. Different countries have implemented various strategies to address similar challenges.
- Universal Healthcare Systems: Many developed nations, such as Canada and the UK, have universal healthcare systems that guarantee access to care for all citizens. This contrasts with the US system, which relies on a mix of public and private insurance, leading to disparities in access and quality of care.
- Robust Social Safety Nets: Countries with robust social safety nets, such as Sweden and Norway, provide comprehensive support for families and children. These programs often include generous parental leave, subsidized childcare, and financial assistance for low-income families, which contribute to improved child well-being.
Policy Solutions Table
| Policy | Description | Potential Impact |
|---|---|---|
| Universal Pre-Kindergarten | Providing free preschool education to all 4-year-olds | Improved cognitive and social-emotional development, reduced disparities in school readiness |
| Expanded Medicaid Eligibility | Expanding Medicaid coverage to more low-income families | Increased access to healthcare for vulnerable children, reduced rates of preventable illnesses |
| Increased Funding for Early Intervention Programs | Providing more resources for programs that identify and address developmental delays | Improved developmental outcomes, reduced need for expensive special education services |
| Comprehensive Housing Assistance Programs | Strengthening programs to address housing instability and homelessness | Improved health outcomes by reducing stress, improving access to healthcare, and reducing exposure to environmental hazards |
Public Health Initiatives
Public health initiatives play a crucial role in safeguarding child health, by focusing on preventive measures and addressing the root causes of poor outcomes. Effective strategies encompass a wide range of interventions, from vaccinations to improved sanitation and access to nutritious food. Understanding how these initiatives are implemented and their effectiveness in various contexts is essential for developing tailored solutions to reduce child mortality and improve overall well-being.Public health initiatives are not merely reactive responses to existing health problems; they are proactive strategies designed to promote optimal health outcomes.
By addressing environmental factors, socioeconomic disparities, and access to healthcare, these initiatives aim to create healthier communities where children can thrive. This approach is crucial for mitigating the complex interplay of factors contributing to high child mortality rates in some regions.
The Role of Public Health Initiatives in Promoting Child Health
Public health initiatives are fundamental to promoting child health. They focus on preventing diseases through vaccination campaigns, promoting healthy lifestyles, and ensuring access to essential healthcare services. These initiatives also tackle broader societal factors that impact children’s health, such as poverty, malnutrition, and inadequate sanitation.
Comparing Public Health Strategies and Their Effectiveness in Different Countries
The effectiveness of public health strategies varies significantly across countries, reflecting differences in socioeconomic conditions, healthcare infrastructure, and cultural contexts. Strategies that have proven successful in one country might not yield the same results in another. For instance, a comprehensive immunization program in a country with robust healthcare infrastructure and high vaccination rates will likely be more effective than the same program in a country facing challenges in vaccine distribution or community engagement.
The success of public health strategies hinges on tailoring them to the specific needs and circumstances of the population they are intended to serve.
The Importance of Preventative Measures and Early Intervention
Preventive measures and early intervention are critical components of effective public health initiatives. Early detection and intervention can significantly improve outcomes for children facing health challenges, and prevention programs often have a more profound and sustainable impact than reactive measures. For example, a program focusing on maternal and child nutrition during pregnancy and early childhood can prevent malnutrition and related health problems later in life.
Early childhood development programs are another example of preventative measures that can positively impact a child’s long-term health and well-being.
Public Health Initiatives
- Public Health Initiative: Immunization programs,
Description: Providing free vaccinations to children against preventable diseases. This includes routine vaccinations as well as catch-up campaigns for children who have missed scheduled vaccinations.
- Public Health Initiative: Improved sanitation and hygiene,
Description: Implementing strategies to improve water and sanitation infrastructure, educating communities about hygiene practices, and promoting handwashing to prevent the spread of waterborne diseases.
- Public Health Initiative: Nutritional programs,
Description: Providing access to nutritious food and micronutrient supplements to vulnerable children, particularly during critical growth periods. This includes initiatives like food banks, school feeding programs, and maternal nutrition programs.
- Public Health Initiative: Early childhood development programs,
Description: Promoting cognitive, social, and emotional development in young children through initiatives such as preschool programs, parenting education, and access to early intervention services for children with developmental delays.
- Public Health Initiative: Maternal and child health services,
Description: Strengthening maternal health services to ensure safe pregnancies and births, providing antenatal care, postnatal care, and support for breastfeeding. This also includes programs for family planning and reproductive health.
Environmental Factors
Our environment plays a significant role in shaping the health and well-being of children. Exposure to pollutants and limited access to clean water can have profound and lasting effects, contributing to a range of health issues and even increasing mortality rates. Understanding these environmental factors is crucial to addressing the disparities in child health outcomes seen across developed nations.Environmental conditions directly impact the physical and developmental well-being of children.
Factors such as air and water quality, exposure to toxins, and access to green spaces all contribute to a child’s overall health trajectory. Differences in environmental conditions between the US and other developed nations can exacerbate existing health disparities, leading to varying outcomes in child mortality rates. A closer look at these environmental influences is essential to identify specific contributing factors and develop targeted solutions.
Pollution and Child Health
Air pollution, a pervasive environmental concern, poses a significant threat to children’s health. Fine particulate matter, often emitted from vehicles and industrial sources, can penetrate deep into the lungs, causing respiratory illnesses like asthma and bronchitis. Studies have linked increased exposure to air pollution with lower lung function and higher rates of respiratory infections in children. Similarly, water pollution can lead to contaminated drinking water, increasing the risk of waterborne diseases, which can be particularly severe for young children with developing immune systems.
Access to clean, safe water is a fundamental need for healthy development.
Access to Clean Water and Sanitation
Access to clean water and adequate sanitation is essential for preventing waterborne diseases. Lack of access can lead to a range of health problems, including diarrhea, typhoid, and cholera. These diseases can be especially devastating for young children, often leading to dehydration and long-term health complications. In many developing nations, the absence of clean water and sanitation infrastructure poses a significant risk to children’s survival and well-being.
Comparison of Environmental Conditions
Environmental conditions vary significantly between the US and other developed nations. While the US boasts advancements in certain areas, disparities in access to clean water, adequate sanitation, and air quality exist within its borders. For example, certain communities in the US experience disproportionately high levels of air pollution from industrial sources or traffic, creating significant health risks for children.
This contrasts with other developed nations where more comprehensive environmental regulations and public health initiatives may lead to healthier environmental conditions.
Environmental Factors Contributing to Child Mortality
Several examples illustrate the impact of environmental factors on child mortality. A study in a particular US region found a correlation between high levels of air pollution and increased rates of childhood asthma hospitalizations. Similarly, limited access to clean water in certain impoverished areas has been linked to higher rates of diarrheal diseases among children. These instances highlight the crucial role environmental factors play in child mortality rates and the need for targeted interventions.
Summary of Environmental Factors
| Environmental Factor | Description | Impact on Child Mortality |
|---|---|---|
| Air Pollution | Presence of harmful substances in the air, often from vehicles and industrial sources. | Increased risk of respiratory illnesses, lower lung function, higher rates of respiratory infections. |
| Water Pollution | Contamination of water sources with harmful substances. | Increased risk of waterborne diseases, leading to dehydration and long-term health complications. |
| Lack of Clean Water | Limited access to safe and clean drinking water. | Increased risk of diarrheal diseases, typhoid, and cholera, especially for young children. |
| Inadequate Sanitation | Lack of proper sanitation facilities. | Increased risk of waterborne diseases and other health problems. |
Final Wrap-Up
In conclusion, the significantly higher child mortality rate in the US compared to other developed nations highlights critical areas needing improvement. Addressing the multifaceted issues of healthcare access, socioeconomic factors, and environmental conditions is crucial for reducing this disparity. We need a comprehensive approach involving policy changes, public health initiatives, and community engagement to improve child health outcomes.
The path to a healthier future for American children depends on our collective commitment to these issues.