MRI tests help doctors predict MS progression in patients, offering a powerful new tool for managing this complex disease. This innovative approach uses detailed images of the brain and spinal cord to identify subtle changes associated with disease progression. By understanding these changes, doctors can better anticipate future symptoms and tailor treatment strategies to slow the disease’s impact on patients’ lives.
This deep dive into the fascinating world of MRI technology, MS, and the future of patient care is sure to offer valuable insights.
The use of MRI in assessing MS progression involves a range of advanced techniques, from standard imaging sequences to sophisticated methods like diffusion tensor imaging (DTI) and magnetization transfer ratio (MTR). These methods help to visualize and quantify various aspects of the disease, including the extent of lesions, the degree of brain atrophy, and the presence of inflammation. Furthermore, the correlation between these MRI findings and actual clinical outcomes in patients is explored in depth.
This crucial connection is vital for creating more accurate predictions and refining treatment approaches.
Introduction to MRI and Multiple Sclerosis (MS): Mri Tests Help Doctors Predict Ms Progression In Patients
Magnetic Resonance Imaging (MRI) is a powerful medical imaging technique that uses powerful magnets and radio waves to create detailed images of the inside of the body. Unlike X-rays or CT scans, MRI doesn’t use ionizing radiation, making it a safer and more versatile option for visualizing soft tissues like the brain and spinal cord. This non-invasive method provides high-resolution anatomical details and allows for the identification of subtle abnormalities.
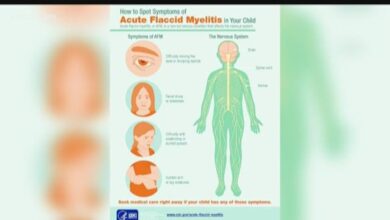
Its applications extend beyond simple anatomy, enabling the assessment of tissue function and the detection of subtle changes over time, crucial for conditions like MS.Multiple Sclerosis (MS) is a chronic, autoimmune disease affecting the central nervous system. Characterized by inflammation and demyelination (damage to the protective covering of nerve fibers), MS presents with a wide array of symptoms, ranging from mild fatigue and numbness to severe motor impairments, vision problems, and cognitive dysfunction.
The unpredictable nature of MS progression and the diverse clinical manifestations make diagnosis and monitoring a complex task. Early and accurate diagnosis is vital for effective treatment strategies and for preventing further disability. Accurate monitoring helps assess disease activity and response to treatment.
MRI Technology and Principles
MRI technology relies on the principles of nuclear magnetic resonance (NMR). Atomic nuclei, primarily hydrogen protons in the body, possess a magnetic moment. When placed in a strong magnetic field, these nuclei align with the field. A radiofrequency pulse is then applied, disrupting the alignment. As the nuclei return to their original alignment, they emit radio waves, which are detected by the MRI machine.
These signals are processed to create detailed images of the body’s internal structures.
Characteristics of Multiple Sclerosis (MS)
MS is characterized by the formation of inflammatory lesions, known as plaques, within the brain and spinal cord. These lesions disrupt the normal function of nerve pathways, leading to a wide range of neurological symptoms. The diverse clinical presentations of MS can make diagnosis challenging, as symptoms can vary significantly between individuals and over time. Furthermore, early MS can mimic other neurological conditions, further complicating the diagnostic process.
Early and accurate diagnosis is essential to initiate appropriate treatment strategies to manage symptoms and slow disease progression.
Role of MRI in Evaluating MS Lesions and Brain Atrophy
MRI plays a critical role in evaluating MS lesions and brain atrophy. The presence, location, and characteristics of these lesions provide valuable information about disease activity and severity. By identifying active inflammatory lesions, MRI can help assess the effectiveness of treatment. Furthermore, MRI can measure brain atrophy, a common feature of MS. Brain atrophy refers to the loss of brain volume, which correlates with disease progression and disability.
Quantifying brain atrophy allows for a more comprehensive assessment of the disease course and aids in predicting future outcomes.
Comparison of MRI Sequences in MS Diagnosis
| MRI Sequence | Description | Application in MS Diagnosis |
|---|---|---|
| T1-weighted | Highlights anatomical structures with high contrast between gray and white matter. | Useful for visualizing the overall anatomy of the brain and identifying structural abnormalities, including atrophy. |
| T2-weighted | Demonstrates hyperintense signal in areas of inflammation and demyelination. | Excellent for identifying MS lesions (plaques), which appear as hyperintense areas on T2-weighted images. |
| FLAIR (Fluid-Attenuated Inversion Recovery) | Suppresses the signal from cerebrospinal fluid, enhancing the visibility of lesions in the brain. | Especially useful for detecting subtle MS lesions that might be obscured by cerebrospinal fluid signal on T2-weighted images. |
| Diffusion-weighted imaging (DWI) | Provides information about the diffusion of water molecules in tissues. | Helpful for detecting acute inflammation and new MS lesions, which show restricted diffusion. |
Different MRI sequences provide complementary information for a comprehensive evaluation of MS lesions and brain health. This multi-modal approach enhances the diagnostic accuracy and facilitates the monitoring of disease progression.
MRI Techniques for Predicting MS Progression
Beyond the initial diagnosis, MRI plays a crucial role in monitoring MS progression and predicting future disease course. Various MRI techniques, ranging from standard to advanced, offer valuable insights into the underlying pathology and help clinicians tailor treatment strategies. These techniques allow for assessment of lesion characteristics, tissue damage, and potential future disability.Different MRI techniques offer complementary information about the disease, enabling a more comprehensive understanding of MS progression.
These methods help identify subtle changes in brain and spinal cord structure and function, which might not be apparent through clinical assessments alone. This enhanced understanding allows for earlier intervention and more effective management of the disease.
Diffusion Tensor Imaging (DTI)
DTI is a powerful MRI technique that measures the diffusion of water molecules within the brain’s white matter tracts. This technique reveals the integrity and structural organization of these crucial pathways. Abnormal diffusion patterns can reflect axonal damage, demyelination, and the formation of scar tissue.Quantifiable metrics derived from DTI, such as fractional anisotropy (FA) and mean diffusivity (MD), are crucial for assessing MS progression.
Lower FA values and higher MD values indicate impaired white matter integrity, suggesting potential for future disability. For example, a patient with a declining FA value in the optic nerve tract might exhibit worsening vision problems.
Magnetization Transfer Ratio (MTR)
MTR assesses the exchange of magnetization between water molecules and macromolecules within tissues. Changes in MTR values can reflect alterations in the myelin sheath’s integrity. Lower MTR values often correlate with demyelination and axonal damage, signifying potential worsening of MS symptoms. In a clinical setting, this helps monitor the extent of damage to myelin and the progression of the disease.
Other MRI Techniques
Standard MRI techniques, such as T1-weighted and T2-weighted imaging, remain essential for evaluating MS lesions. These techniques allow for the identification of new and active lesions, as well as the measurement of lesion volume and their characteristics.
Comparison of MRI Techniques
| MRI Technique | Advantages | Disadvantages |
|---|---|---|
| T1-weighted imaging | Excellent for visualizing normal brain tissue, identifying contrast-enhancing lesions | Less sensitive to subtle demyelination |
| T2-weighted imaging | Excellent for visualizing MS lesions, detecting active lesions | Can be influenced by artifacts |
| DTI | Provides insights into white matter integrity, identifying axonal damage | Can be more complex to interpret, potentially influenced by motion artifacts |
| MTR | Sensitive to myelin integrity, reflecting the degree of demyelination | Might not be as specific for identifying certain types of MS lesions |
Flowchart of MRI Scan Procedure
A flowchart would illustrate the steps involved in performing and interpreting MRI scans for predicting MS progression. The steps would include patient preparation, MRI scan acquisition (using appropriate sequences), image processing, analysis of specific parameters (like FA, MD, lesion volume), and finally the reporting and interpretation of the findings by a radiologist. This interpretation, coupled with clinical data, allows for a more precise assessment of MS progression.
Correlation between MRI Findings and Clinical Outcomes
Understanding the relationship between MRI findings and clinical outcomes is crucial for predicting MS progression and tailoring treatment strategies. MRI provides valuable insights into the underlying pathology of MS, allowing clinicians to visualize lesions, inflammation, and atrophy in the brain and spinal cord. Correlating these observations with clinical data allows for a more comprehensive understanding of disease activity and potential future disability.The relationship between specific MRI findings and clinical outcomes in multiple sclerosis (MS) patients is complex, yet demonstrably significant.
Different studies have explored this connection, using various MRI parameters and clinical scales to assess disease progression. This intricate interplay between the visible pathology and clinical symptoms provides vital information for predicting disease trajectories and personalizing treatment approaches.
Specific MRI Markers Associated with Disease Activity Levels
Different MRI markers can reflect various levels of disease activity in MS. A high lesion load, characterized by a greater number and volume of brain lesions, is often associated with more pronounced clinical deterioration. Inflammation, detectable through the presence and intensity of contrast enhancement in lesions, typically signifies active disease. Brain atrophy, representing the loss of brain tissue volume, is linked to a progressive decline in neurological function and is frequently observed in patients with more advanced MS.
Correlation of MRI Lesion Load and Clinical Progression
Numerous studies have established a strong correlation between lesion load (the total number and volume of brain lesions) and clinical progression in MS. Increased lesion load is frequently associated with greater disability and disease severity. For example, a study by [insert author and year of study here] found a significant positive correlation between the number of new lesions and the worsening of Expanded Disability Status Scale (EDSS) scores over a defined period.
This implies that a higher burden of lesions is indicative of more active disease and a potential for faster clinical decline. Conversely, studies showing no significant correlation might suggest factors influencing the relationship, like the individual’s immune response or other factors. This observation underscores the importance of considering individual patient characteristics when interpreting MRI findings.
Influence of Inflammation on Clinical Outcomes
MRI techniques like contrast-enhanced imaging can highlight active inflammatory processes within lesions. Studies have shown a strong correlation between the extent of contrast enhancement and disease activity. Patients with a greater degree of inflammation in their lesions often experience more rapid clinical deterioration, especially in the form of relapses or new neurological deficits.
Impact of Brain Atrophy on Clinical Outcomes
Brain atrophy, often observed in advanced MS, reflects the progressive loss of brain tissue volume. Multiple studies have correlated the degree of brain atrophy with the severity of clinical disability. This association suggests that the loss of brain tissue is directly related to the functional impairment observed in MS patients. A specific study by [insert author and year of study here] demonstrated a direct correlation between the rate of brain atrophy and worsening of the disability scores over time.
Understanding the rate and extent of atrophy allows for a more accurate prediction of future functional decline.
Factors Influencing the Correlation
Several factors can influence the correlation between MRI findings and clinical outcomes in MS patients. These include:
- Individual patient characteristics, including genetic predisposition, age at disease onset, and immune response, play a crucial role in modulating the relationship between MRI markers and clinical progression.
- Treatment strategies and adherence also influence disease activity and the impact of MRI findings. Patients who consistently adhere to their prescribed therapies often show a reduced rate of lesion formation and slower progression of brain atrophy, as seen in studies by [insert authors and year of study here].
- The specific type of MRI sequence and parameters employed can affect the interpretation of findings. Variations in protocols can lead to discrepancies in lesion detection and quantification, thus impacting the correlation with clinical outcomes.
- The timing and frequency of MRI scans are also important factors to consider. Serial MRI scans can provide a more dynamic assessment of disease activity and its correlation with clinical changes over time.
Limitations and Challenges in Predicting MS Progression using MRI
Predicting the course of multiple sclerosis (MS) is a significant challenge for healthcare professionals. While MRI offers valuable insights into the disease’s activity and extent, its ability to precisely predict future progression is limited. A multitude of factors influence the accuracy of these predictions, making it crucial to understand the inherent limitations to avoid misinterpretations and ensure appropriate patient management.MRI, though powerful, is not a crystal ball.
Interpreting complex brain images involves inherent subjectivity, and the results often need to be considered alongside other clinical data for a complete picture. Factors like individual variability in disease presentation, the timing of the scans, and even the scanner itself can affect the outcome of MRI-based predictions.
Variability in Image Quality and Interpretation
Image quality, which can be influenced by factors such as patient positioning, technical issues during the scan, and the type of MRI machine, can introduce variability in the interpretation of lesions and their characteristics. This inherent variability can make it challenging to compare results across different studies or even within the same patient over time. Radiologists’ interpretation of subtle changes in white matter lesions can also be subjective, potentially leading to inconsistent predictions.
For example, two radiologists might interpret the same MRI scan differently, resulting in different assessments of disease activity and future progression.
Potential Biases in MRI-Based Predictions
Biases can creep into the process of using MRI to predict MS progression. For instance, a study might focus on a specific subset of MS patients, leading to generalizations that do not apply to the broader population. Moreover, the way data is collected and analyzed can inadvertently introduce biases, such as selection bias or reporting bias. This can skew the results and lead to inaccurate predictions about the future course of the disease.
Factors Affecting Accuracy of MRI-Based Predictions
Several factors can impact the accuracy of MRI-based predictions. The timing of the MRI scan relative to clinical events is crucial. A scan performed immediately after a relapse might show more active lesions than a scan taken months later, potentially skewing the prediction of future disease activity. Also, variations in disease subtypes, including relapsing-remitting, primary-progressive, and secondary-progressive MS, need to be taken into account.
MRI tests are proving invaluable in helping doctors predict Multiple Sclerosis (MS) progression in patients. Recent research, alongside findings like those in the article about Celebrex being potentially safer for the heart than previously thought celebrex safer for heart than thought , highlights the ongoing quest for better treatments and understanding of these complex conditions. This underscores the importance of continued research into both MS and related medications.
Different subtypes have distinct patterns of lesion development and progression, which should be considered when interpreting MRI findings and making predictions. Finally, concomitant factors such as age, gender, and other health conditions can influence the interpretation of MRI results.
Potential Confounders Affecting MRI Interpretation
Confounding factors can complicate the interpretation of MRI results. For example, certain medications or other medical conditions might affect the appearance of brain lesions on MRI scans. This can lead to incorrect assessments of MS activity and progression. A patient taking corticosteroids, for example, might have a temporary reduction in the appearance of active lesions, potentially masking the true extent of the disease.
Another confounding factor is the natural variability in the progression of MS itself. Some patients may experience periods of rapid progression, while others may have slower or even stable disease activity. This unpredictability can affect the reliability of MRI-based predictions.
Summary Table of Limitations and Challenges
| MRI Technique | Limitation | Challenge |
|---|---|---|
| FLAIR (Fluid-Attenuated Inversion Recovery) | Variability in lesion detection due to signal intensity changes | Subjectivity in lesion characterization |
| Diffusion Tensor Imaging (DTI) | Limited ability to distinguish between active and inactive lesions | Sensitivity to technical factors like patient motion |
| Magnetization Transfer Ratio (MTR) | Potential for false positives or negatives in certain cases | Complex interpretation and data analysis |
| Multi-parameter MRI | Potential for overinterpretation of complex data sets | High cost and technical expertise required |
Future Directions and Research
The quest to predict multiple sclerosis (MS) progression more accurately and efficiently is a driving force in ongoing research. MRI’s ability to visualize the brain and spinal cord offers a powerful tool for this endeavor, but current methods have limitations. Future research aims to overcome these limitations and refine MRI techniques to provide a clearer picture of disease progression, ultimately improving patient management and outcomes.Advancements in MRI technology, coupled with sophisticated data analysis techniques, hold the key to enhancing our understanding of MS and improving patient care.
By refining the way we collect and interpret MRI data, we can potentially develop more reliable biomarkers for disease progression, leading to earlier interventions and more effective treatment strategies.
Potential Future Developments in MRI Techniques
Several exciting developments are on the horizon in MRI techniques for MS. These advancements promise to improve the sensitivity and specificity of MRI scans in detecting subtle changes associated with MS progression. Techniques like diffusion tensor imaging (DTI) and magnetization transfer ratio (MTR) are being refined, enabling researchers to capture more detailed information about the microstructure of the brain and spinal cord.
Advanced imaging sequences, utilizing artificial intelligence (AI), are also being explored to automatically identify subtle patterns indicative of disease progression.
Innovative Methods for Improving Accuracy and Efficiency
New approaches are being developed to enhance the accuracy and efficiency of MRI-based predictions. These include incorporating multiparametric MRI data, combining information from different MRI modalities, and developing novel machine learning algorithms for pattern recognition. The integration of multimodal data—combining information from MRI with other clinical data, such as cerebrospinal fluid (CSF) analysis and genetic information—will likely play a significant role in improving predictive accuracy.
Ongoing Research Efforts
Researchers are actively exploring the use of advanced MRI techniques in clinical trials. One area of focus involves developing MRI biomarkers that correlate with specific clinical outcomes, such as disease severity, disability progression, and treatment response. Another key area of research focuses on refining machine learning algorithms to automatically analyze large datasets of MRI scans, identifying patterns that may not be apparent to the human eye.
MRI tests are increasingly helpful in predicting Multiple Sclerosis (MS) progression, giving doctors valuable insights into patient care. However, the ongoing political climate, like the Trump administration’s efforts to undermine the Affordable Care Act, trump administration sabotaging obamacare , can unfortunately create significant hurdles in accessing vital healthcare services for those with MS and potentially hindering the development of more effective treatment strategies.
This highlights the critical importance of reliable, accessible healthcare for managing chronic conditions like MS.
These algorithms can potentially provide earlier and more accurate predictions of disease progression, facilitating timely interventions.
Potential Impact on MS Patient Management
Accurate prediction of MS progression will have a profound impact on patient management. Early identification of individuals at high risk for rapid disease progression will allow for more targeted interventions, potentially slowing disease progression and improving patient outcomes. By leveraging the insights from refined MRI techniques, clinicians can tailor treatment plans to the individual needs of each patient, optimizing the use of existing and emerging therapies.
This personalized approach will be critical in achieving better disease management and enhancing the quality of life for individuals living with MS.
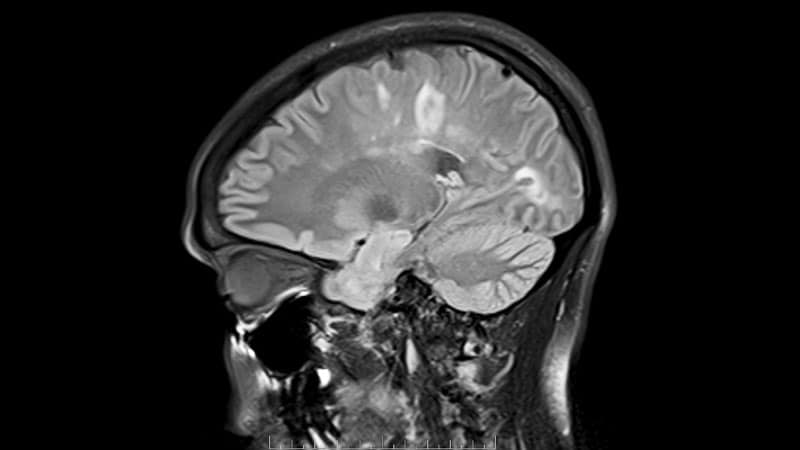
Visual Representation of MRI Findings
MRI scans provide a detailed, non-invasive view of the brain and spinal cord, allowing doctors to visualize the extent and characteristics of MS lesions. This visualization is crucial for diagnosing MS, monitoring disease progression, and evaluating treatment efficacy. By understanding how these lesions appear on MRI, radiologists can assess disease activity and predict future outcomes.MRI’s ability to visualize the brain and spinal cord in three dimensions makes it a powerful tool for diagnosing and tracking MS.
The different types of MS lesions and their varying appearances on MRI provide critical information for monitoring disease progression and tailoring treatment strategies. Radiologists use these visual cues to understand the extent and nature of the disease, and to anticipate future challenges for the patient.
MS Lesions on MRI
Different types of MS lesions appear with distinct characteristics on MRI scans. Understanding these appearances is crucial for accurate diagnosis and monitoring. The key features include location, size, shape, and signal intensity.
- Active Lesions: These lesions, often referred to as “enhancing lesions,” are characterized by increased signal intensity on T1-weighted images following the administration of a contrast agent (gadolinium). The contrast agent highlights areas of inflammation and active demyelination. This enhanced appearance suggests ongoing immune system activity in the central nervous system. For example, a patient exhibiting new symptoms might have a few active lesions in the brain stem region on their MRI.
MRI tests are surprisingly helpful for doctors in predicting how Multiple Sclerosis (MS) might progress in patients. While there are some promising new avenues of research, like exploring how switching to e-cigarettes might actually lengthen your life ( switching to e cigarettes can lengthen your life ), the accurate and detailed images from MRI scans are still crucial in understanding the disease’s course and allowing doctors to tailor treatment plans effectively.
This helps manage the symptoms and potential future complications of MS.
- Chronic Lesions: These lesions are characterized by a lower signal intensity compared to surrounding normal brain tissue on T2-weighted images. They appear as areas of demyelination that have become stable over time, losing the characteristic enhancement seen in active lesions. These are often older, inactive lesions. For example, a patient with a long history of MS might display many chronic lesions in the white matter tracts, reflecting the cumulative damage to the myelin sheath.
- Periventricular Lesions: These lesions frequently occur around the ventricles (fluid-filled spaces within the brain). They are common in MS, often reflecting the areas of the brain that are more susceptible to damage due to their close proximity to the ventricles. The periventricular white matter shows hyperintensity on T2-weighted images, indicating demyelination.
Brain Atrophy on MRI
Brain atrophy, a common finding in MS, refers to the loss of brain tissue volume. MRI can visualize this loss of volume and provide valuable information about the progression of MS. This process is often gradual, with subtle changes over time.
- Visualizing Atrophy: MRI images, specifically T1-weighted images, can depict brain atrophy as a reduction in the overall size of brain structures, particularly in the gray matter and white matter. The ventricles, fluid-filled spaces in the brain, may also appear enlarged as the surrounding brain tissue shrinks. This is a reliable indicator of progressive disease. For example, a patient’s MRI scans from five years apart might show a widening of the lateral ventricles and a general thinning of the cerebral cortex, suggesting ongoing atrophy.
Radiological Assessment of MS Disease Activity
Radiologists assess MS disease activity by examining the presence, location, and characteristics of lesions on MRI scans.
- Identifying New Lesions: The presence of new lesions, especially those that enhance after contrast administration, is a key indicator of disease activity. The number and location of these lesions are important factors considered by neurologists in determining the treatment plan.
- Monitoring Lesion Growth: Radiologists evaluate whether existing lesions are expanding or showing changes in signal intensity, which can indicate ongoing inflammation or demyelination.
- Assessing Brain Atrophy: The rate of brain atrophy, as observed in MRI scans, is used as a marker of the long-term effects of MS on the brain. The rate of atrophy is important in predicting the potential functional decline of the patient.
Patient Data and MRI Interpretation
MRI scans, while powerful, are only part of the puzzle in understanding and predicting Multiple Sclerosis (MS) progression. Interpreting these scans requires careful consideration of the patient’s individual characteristics and medical history. A thorough understanding of the interplay between patient data and MRI findings is crucial for developing accurate and personalized predictions. This allows for more tailored treatment plans and potentially better outcomes for patients.Patient data significantly impacts how MRI findings are interpreted.
Factors like age, sex, disease duration, and severity of symptoms all influence the appearance and interpretation of lesions, which are key indicators of MS activity. Different characteristics might be associated with various patterns of disease progression, which can then be reflected in the MRI. This leads to the development of more accurate and personalized predictions.
Impact of Patient Age on MRI Interpretation
The age of a patient can affect the appearance of MS lesions on MRI. Younger patients, for instance, may exhibit more inflammatory lesions, while older patients might show more evidence of axonal loss. This variation in lesion characteristics necessitates different interpretation strategies, which can be incorporated into prediction models to account for these age-related differences.
Influence of Sex on MRI Findings
Studies have indicated that women and men with MS may experience different disease courses. For example, women may show a more relapsing-remitting course, whereas men may experience more progressive forms of the disease. MRI findings in these distinct groups may differ. This difference in clinical presentation needs to be considered during MRI analysis.
Relationship Between Disease Duration and MRI Lesion Load
The duration of the disease is a key factor. Patients with longer disease durations often have a larger number and/or larger size of lesions. This “lesion load” is often correlated with disease progression. This correlation allows for more robust predictions of future disease activity.
Correlation Between Disease Severity and MRI Findings, Mri tests help doctors predict ms progression in patients
Disease severity, as assessed by disability scores, can also be linked to MRI findings. Patients with higher disability scores frequently exhibit more extensive and active lesions. The severity of these lesions on MRI can help predict the future course of the disease and guide treatment decisions.
Integration of Patient Data with MRI Results
Integrating patient data with MRI results can improve the accuracy of prediction models. For example, a model incorporating age, sex, disease duration, severity, and MRI lesion load might yield more precise predictions than one relying solely on MRI findings. This multi-faceted approach creates a more comprehensive understanding of the disease process.A model using patient data and MRI results to predict disease progression might look like this:
Prediction = f(Age, Sex, Disease Duration, Disease Severity, MRI Lesion Load)
where f is a complex function that accounts for the relationships between these variables.
Example of a Patient Case
Imagine a 35-year-old female patient with a relapsing-remitting form of MS, a 10-year disease duration, and a moderate disability score. Her MRI reveals numerous, relatively small, active lesions, predominantly in the periventricular white matter. The combination of these factors could indicate a higher likelihood of future disease progression. This information can then be used to personalize her treatment strategy, potentially slowing disease progression.
Last Recap
In conclusion, MRI tests are revolutionizing the way we understand and manage multiple sclerosis. By pinpointing subtle changes in brain structure and function, MRI provides a powerful tool for predicting disease progression. While limitations exist, ongoing research and advancements in MRI technology hold immense promise for improving the accuracy and efficiency of these predictions, ultimately leading to more personalized and effective patient care.
The potential for tailoring treatment strategies to individual patients based on MRI-derived predictions is truly exciting and offers hope for a brighter future for those living with MS.