My experience breastfeeding and mental health medications is a journey filled with both challenges and triumphs. It’s a deeply personal one, and I want to share the realities of balancing these crucial aspects of motherhood. From navigating common breastfeeding difficulties to understanding the impact of various medications on milk production and infant health, this exploration delves into the complexities of this sensitive topic.
It also emphasizes the vital role of open communication with healthcare providers and the importance of supportive resources.
This post details my personal experience with breastfeeding and mental health medications. It explores the common breastfeeding challenges, discusses the impact of mental health conditions on breastfeeding, and details the importance of consulting with healthcare professionals. I’ll also discuss potential medication interactions and available support systems. Finally, I share some personal stories and experiences from other breastfeeding mothers.
Breastfeeding Experiences and Medications

Breastfeeding is a beautiful and rewarding journey, but it can also be challenging. Many factors, including maternal health conditions and medication needs, can influence this experience. Understanding the potential impact of medications on breastfeeding is crucial for both the health of the mother and the infant. This discussion delves into the complexities of breastfeeding and medications, emphasizing the importance of professional guidance.
Common Breastfeeding Challenges
Breastfeeding presents a variety of challenges. These range from establishing a consistent milk supply and latch difficulties to potential pain and discomfort. Mothers often experience engorgement, cracked nipples, and milk letdown issues. These challenges, while common, can be frustrating and may require professional support to resolve.
Potential Impacts of Medications on Milk Production and Quality
Medications can cross into breast milk, potentially affecting both its quantity and quality. The extent of this impact varies greatly depending on the specific medication, dosage, and the individual mother’s physiology. Some medications may decrease milk production, while others might alter the taste or texture of the milk. The absorption rate of the medication in the mother’s body also plays a critical role in determining the level of the medication in the breast milk.
Importance of Consulting Healthcare Professionals
Consulting with healthcare professionals before taking any medication during breastfeeding is paramount. This proactive approach allows for careful consideration of potential risks and benefits. Healthcare providers, including lactation consultants and obstetricians, can provide personalized guidance based on individual circumstances. They can assess the mother’s specific needs and the potential effects of the medication on both the mother and the baby.
This personalized advice is essential to making informed decisions.
Comparison of Potential Risks and Benefits
The decision to take a medication during breastfeeding involves weighing the potential risks to the infant against the potential benefits to the mother. For example, a medication may be crucial for managing a serious health condition, but the potential side effects on the infant must be carefully considered. This necessitates a thorough discussion between the mother and her healthcare provider, who can help evaluate the specific risks and benefits.
Medications Generally Considered Safe During Breastfeeding
Certain medications are generally considered safe for use during breastfeeding. These medications typically have a low risk of transferring to breast milk in significant quantities or posing adverse effects on the infant. This safety is often determined through extensive research and clinical trials.
Table of Medications and Potential Effects on Milk
| Medication Name | Potential Effects on Milk | Safety During Breastfeeding | Relevant Precautions |
|---|---|---|---|
| Acetaminophen (Tylenol) | Low risk of transfer to breast milk; minimal impact on milk production. | Generally safe. | Use in recommended dosages. |
| Ibuprofen (Advil) | May decrease milk production; potential for minimal transfer to breast milk. | May be used cautiously. | Monitor infant for any unusual effects. |
| Antibiotics (e.g., penicillin) | Low risk of transfer; minimal impact on milk production. | Generally safe. | Monitor infant for allergic reactions. |
| Some antidepressants (e.g., sertraline) | May have a slight impact on milk production. | May be used cautiously, with close monitoring. | Monitor infant for any unusual effects. Consult with a physician. |
Mental Health Considerations During Breastfeeding
The postpartum period, a time of profound physical and emotional change, can be challenging for many mothers. Navigating the complexities of breastfeeding alongside potential mental health concerns requires understanding the interplay between these two vital aspects of a mother’s well-being. This period often involves significant hormonal shifts, sleep deprivation, and the added responsibility of caring for a newborn.
Recognizing the signs and understanding the resources available can significantly impact a mother’s experience during this crucial time.The link between postpartum mental health and breastfeeding is complex and multifaceted. Fluctuations in hormones, sleep deprivation, and the emotional adjustments of motherhood can contribute to the development or exacerbation of existing mental health conditions. Conversely, mental health conditions can negatively impact a mother’s ability to successfully breastfeed, affecting both her physical and emotional state.
Addressing these interconnected challenges is essential for optimal maternal and infant well-being.
Postpartum Mental Health Conditions
Postpartum mental health conditions encompass a range of concerns, from the relatively common “baby blues” to more severe conditions like postpartum depression and postpartum psychosis. These conditions are characterized by a constellation of emotional, behavioral, and physical symptoms. Understanding the various forms of these conditions allows for appropriate intervention and support.
Common Postpartum Mental Health Concerns
- Postpartum “baby blues”: Characterized by mood swings, tearfulness, anxiety, and irritability, these typically resolve within a few weeks without intervention. It’s important to acknowledge these common feelings and recognize that they often subside naturally. Support and understanding are crucial.
- Postpartum depression (PPD): A more severe condition, PPD involves persistent sadness, loss of interest in activities, feelings of worthlessness, and changes in sleep and appetite. Symptoms can persist for weeks or months and significantly impact a mother’s ability to care for herself and her baby. Seeking professional help is vital.
- Postpartum anxiety: Characterized by excessive worry, fear, and panic attacks, postpartum anxiety can interfere with daily life and negatively impact a mother’s ability to bond with her baby. It is often accompanied by physical symptoms like racing heart and shortness of breath.
- Postpartum psychosis: A rare but serious condition, postpartum psychosis involves severe mood swings, hallucinations, delusions, and disorganized thinking. It requires immediate medical attention to ensure the safety of both the mother and the baby.
Importance of Seeking Support
Acknowledging and addressing mental health challenges during breastfeeding is crucial. Open communication with healthcare providers, support groups, and loved ones can provide a safety net and facilitate appropriate intervention. Seeking support demonstrates strength and commitment to one’s well-being and the well-being of the child. Early intervention can significantly improve outcomes and minimize the impact on both mother and child.
Resources for Mothers Experiencing Mental Health Challenges
Numerous resources are available to support mothers experiencing mental health challenges during breastfeeding. These include:
- Healthcare providers: Obstetricians, pediatricians, and mental health professionals are vital sources of information and support. Open communication with these professionals is essential for developing a personalized treatment plan.
- Support groups: Connecting with other mothers experiencing similar challenges can provide emotional support and practical advice. Support groups offer a safe space to share experiences and learn from others.
- Online resources: Websites and online forums can offer information, coping strategies, and connection with other mothers. However, it’s important to verify the accuracy and reliability of the information found online.
Support Options for Postpartum Mental Health Concerns
| Mental Health Concern | Common Symptoms | Support Options | Relevant Resources |
|---|---|---|---|
| Postpartum “baby blues” | Mood swings, tearfulness, anxiety, irritability | Rest, support from loved ones, and reassurance | Healthcare providers, support groups |
| Postpartum Depression (PPD) | Persistent sadness, loss of interest, worthlessness, sleep/appetite changes | Therapy, medication (if appropriate), support groups | Mental health professionals, PPD support groups, national helplines |
| Postpartum Anxiety | Excessive worry, fear, panic attacks, physical symptoms | Therapy, medication (if appropriate), relaxation techniques | Anxiety support groups, mental health professionals |
| Postpartum Psychosis | Severe mood swings, hallucinations, delusions, disorganized thinking | Hospitalization, medication, and intensive support | Emergency services, psychiatric hospitals |
Medication Interactions and Breastfeeding

Navigating the world of breastfeeding while managing mental health can be challenging, especially when medication is involved. Understanding potential interactions between medications and breast milk is crucial for both the health of the mother and the infant. This section delves into the specifics of medication interactions, focusing on the importance of consulting healthcare professionals and tailoring medication choices to minimize risks.Medication interactions during breastfeeding are complex, and a one-size-fits-all approach isn’t viable.
Each medication has unique characteristics, and its interaction with breast milk depends on factors such as the medication’s half-life, dosage, and timing of administration. A thorough understanding of these elements is essential for safe and informed decision-making.
Breastfeeding and mental health meds can be tricky, especially when you’re navigating potential side effects. I was curious about whether these medications might end up in my breast milk, and wondered if there was a connection to things like e-cigarettes containing prescription drugs, as it seemed like a logical parallel. Thankfully, I found some good information on the topic of do e cigarettes contain prescription drugs that helped put my mind at ease.
Ultimately, I felt more confident in my decision to continue breastfeeding while on my medication, with the right support and research.
Potential Medication Interactions
Understanding potential interactions is paramount for a safe breastfeeding journey. Many medications can pass into breast milk, potentially affecting the infant. The extent of this transfer varies significantly based on the medication’s properties.
Common Medications with Potential Interactions
A range of medications can potentially interact with breastfeeding. It’s important to note that this is not an exhaustive list, and individual circumstances may differ. Always consult with a healthcare professional for personalized guidance.
- Antidepressants: Some antidepressants, like selective serotonin reuptake inhibitors (SSRIs), have been reported to pass into breast milk, although generally at low concentrations. However, individual responses can vary. Careful monitoring and consultation with a healthcare professional are recommended.
- Antipsychotics: Certain antipsychotic medications may be present in breast milk. The potential impact on the infant needs careful consideration, and close monitoring by a healthcare professional is advisable.
- Anti-anxiety medications: Similar to antidepressants, some anti-anxiety medications can be found in breast milk. The specific impact on the infant depends on the medication and its dosage. Consultation with a healthcare professional is necessary.
- Pain relievers: Over-the-counter pain relievers, like ibuprofen, can pass into breast milk. Dosage and frequency need to be carefully considered.
Medication Half-Life and Milk Composition
Medication half-life significantly impacts the concentration of medication in breast milk. The half-life is the time it takes for the concentration of a medication to decrease by half. Medications with shorter half-lives generally have lower concentrations in breast milk compared to those with longer half-lives.
The longer the half-life, the more prolonged the potential exposure of the infant.
Understanding half-life is crucial for determining the appropriate timing of medication administration relative to breastfeeding. For example, administering a medication with a short half-life closer to breastfeeding sessions might reduce the infant’s exposure.
Dosage and Timing Considerations
Medication dosage and timing directly influence the concentration of medication in breast milk. Higher dosages generally result in higher concentrations in breast milk. Timing, in relation to breastfeeding sessions, is also crucial. Administering medication several hours before or after breastfeeding can help reduce infant exposure.
- Dosage adjustments: In some cases, dosage adjustments might be necessary to balance the mother’s health needs with the infant’s safety.
- Frequency and timing: Medication frequency and the time of administration relative to breastfeeding sessions are essential factors to consider.
Medication Interactions Table, My experience breastfeeding and mental health medications
This table provides a summary of potential interactions for common medications and breastfeeding. It’s crucial to remember that this is not an exhaustive list and individual responses can vary. Always consult with a healthcare professional for personalized advice.
| Medication | Potential Interaction with Breastfeeding | Dosage Considerations | Precautions |
|---|---|---|---|
| SSRIs (e.g., Sertraline) | Generally low concentrations in breast milk; potential for mild side effects in infant; individual variation | Consult with healthcare provider regarding dosage and potential impact on infant | Close monitoring of infant for any unusual symptoms |
| Antipsychotics (e.g., Risperidone) | Can be present in breast milk; potential for side effects in infant | Dosage should be minimized when possible | Monitor infant for potential side effects; consider alternative medications if possible |
| Ibuprofen | Can pass into breast milk; potential for gastrointestinal issues in infant at high doses | Use lowest effective dose; consider timing relative to breastfeeding | Monitor infant for any unusual symptoms |
| Codeine | Potential for side effects in infant; may interfere with infant sleep | Use lowest effective dose; consider timing relative to breastfeeding | Monitor infant for any unusual symptoms |
Support Systems and Resources
Navigating breastfeeding while taking medication can feel isolating. Understanding the available support systems and resources is crucial for both maintaining a healthy breastfeeding relationship and managing your mental health. Knowing where to turn for guidance and encouragement can make a significant difference in the journey.Finding support is essential to ensure both the health of the mother and the baby.
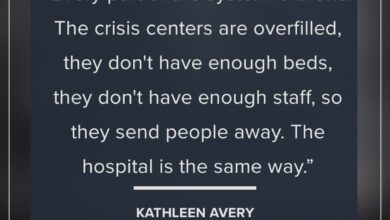
Breastfeeding while on mental health medications was a rollercoaster. Finding the right balance was tough, and I felt like there weren’t enough resources readily available to help navigate the unique challenges. This is especially true considering the often-overlooked services lacking for mental health support during and after pregnancy, particularly for mothers, which can make the whole experience even more isolating.
services lacking for mental health Ultimately, I felt like I was stumbling through the process, hoping for more support systems, which highlights the need for more comprehensive resources for breastfeeding mothers managing mental health conditions.
Accessing reliable information and connecting with others who share similar experiences can ease anxiety and provide practical strategies for success. It’s important to remember that you are not alone in this process.
Available Support Systems
Support systems play a vital role in providing emotional and practical assistance to breastfeeding mothers on medication. These systems offer a network of understanding and encouragement, addressing concerns and offering solutions tailored to individual needs.
- Support Groups: Support groups, both in-person and online, offer a safe space to share experiences, ask questions, and receive encouragement from others facing similar challenges. These groups can be invaluable in validating feelings and providing a sense of community, helping to normalize the experience and address anxieties about breastfeeding and medication. The collective knowledge and shared wisdom of group members can provide practical advice and strategies for navigating specific situations.
Breastfeeding and mental health meds were a tricky combo. I was worried about potential side effects on my little one, and it was tough juggling everything. Interestingly, research shows similar complexities with other health challenges, like the relationship between smoking and non small cell lung cancer smoking and non small cell lung cancer. Thankfully, my doctor was very supportive in navigating the choices, and I ultimately felt comfortable with my decisions.
My experience highlights the need for open communication and support when facing such decisions.
- Healthcare Providers: Open communication with your healthcare provider is paramount. They can provide personalized advice on managing medication and breastfeeding, and can help address any concerns or complications that may arise. They are an essential part of your support network, offering expert guidance and tailored solutions.
- Lactation Consultants: Lactation consultants are specialists in breastfeeding. They can provide personalized guidance on breastfeeding techniques, identify potential challenges, and offer solutions tailored to your individual circumstances. They can also address concerns related to medication use and its impact on breastfeeding.
Online Resources and Communities
The internet provides a wealth of information and support for breastfeeding mothers. Online communities and resources can connect you with a broader network of support and provide access to a diverse range of experiences and perspectives.
- Online Forums and Communities: Online forums and communities dedicated to breastfeeding and/or mental health can provide a valuable platform for connecting with others facing similar challenges. These spaces offer a platform to share experiences, ask questions, and receive support and advice from a larger community.
- Websites and Articles: Many websites and articles provide comprehensive information on breastfeeding and medication interactions. These resources can offer a wealth of knowledge, enabling you to make informed decisions about your healthcare and breastfeeding journey.
Importance of Open Communication
Open communication with healthcare providers is crucial for managing breastfeeding and medication use effectively. Regular check-ins and honest discussions about concerns can ensure the safety and well-being of both mother and child.
- Medication Information: Discuss all medications, including prescriptions, over-the-counter drugs, and supplements, with your healthcare provider to ensure safety and effectiveness.
- Breastfeeding Concerns: Communicate any concerns you have about breastfeeding, such as changes in milk supply or difficulty latching, with your healthcare provider. They can help determine if there are underlying causes or potential solutions.
Examples of Resources
Several websites and support groups provide guidance on breastfeeding and medication. Some reputable resources include La Leche League International and websites of major medical organizations. Consulting these resources can help you make informed decisions.
| Support System | Contact Information | Support Types | Location |
|---|---|---|---|
| La Leche League International | [Website address] | Support groups, articles, workshops | International |
| International Lactation Consultant Association (ILCA) | [Website address] | Certified lactation consultant referrals | International |
| Your Healthcare Provider | [Your provider’s contact information] | Personalized advice, medication management | Your location |
Individual Experiences and Stories: My Experience Breastfeeding And Mental Health Medications
Breastfeeding while managing mental health medications can be a deeply personal and often challenging journey. Mothers face a complex web of emotions, practical concerns, and uncertainties. Sharing personal experiences can offer invaluable support and understanding for those navigating similar situations. This section aims to illuminate the diverse realities of breastfeeding mothers on medication, showcasing both the hurdles and triumphs encountered.
The experiences Artikeld below are not intended as medical advice. Always consult with your healthcare provider for personalized guidance on breastfeeding and medication interactions. These stories highlight the importance of open communication and support systems in fostering successful breastfeeding while managing mental health conditions.
Diverse Breastfeeding Experiences
Mothers’ experiences with breastfeeding while taking mental health medications vary significantly. Some find that medication has minimal impact on their milk supply or their baby’s health, while others encounter challenges that require careful management and adjustments.
Challenges and Triumphs
Breastfeeding mothers on medication often encounter challenges like fluctuating milk supply, concerns about potential medication transfer to the baby, and the emotional toll of navigating complex medical decisions. Simultaneously, many report remarkable triumphs, finding ways to successfully breastfeed while maintaining their mental health and providing nourishment to their infants. These positive experiences often hinge on a robust support network and open communication with healthcare professionals.
Personal Experiences (Anonymized)
- One mother, identified as “Sarah,” experienced a decrease in milk supply after starting an antidepressant. She successfully adjusted her diet and hydration, alongside close monitoring from her lactation consultant, to maintain a sufficient milk supply for her baby.
- “Emily” found that her anxiety medication caused some mild discomfort during breastfeeding, but the benefits of managing her anxiety outweighed the temporary inconvenience. She diligently documented her observations and communicated with her physician to ensure the safety of her infant.
- “Olivia” experienced significant fluctuations in milk production after starting a mood stabilizer. Through a combination of support from her partner and lactation support groups, she successfully maintained breastfeeding with the help of supplemental feedings. She discovered that patience and perseverance were key to her breastfeeding journey.
Strategies for Overcoming Challenges
Many mothers have found success by employing various strategies to overcome breastfeeding challenges while on medication. These include seeking expert lactation consultation, adjusting their medication schedules, and prioritizing open communication with their healthcare providers. They also highlight the significance of building a strong support network, fostering self-care, and acknowledging the emotional complexity of the situation.
Importance of Positive Role Models and Support Networks
Positive role models and strong support networks are crucial for navigating the emotional and practical complexities of breastfeeding while on medication. Sharing experiences with other mothers who have been in similar situations can provide invaluable encouragement and practical advice. Support from partners, family, and friends is equally important in easing the burden and promoting a sense of camaraderie.
Navigating the Emotional Journey
The emotional journey of breastfeeding while on medication can be complex and unpredictable. Mothers often experience a mix of emotions, including anxiety, frustration, and feelings of inadequacy. Recognizing and acknowledging these emotions is the first step toward managing them effectively. Building a supportive network and focusing on self-care are crucial for navigating this emotional terrain.
Potential Impacts on Infant Health
Breastfeeding is generally the best source of nutrition for infants, providing essential antibodies and nutrients crucial for their development. However, when a breastfeeding mother takes medication, the possibility exists that the medication will be present in breast milk, potentially affecting the infant. Understanding these potential impacts is vital for both the mother and the infant’s well-being.A crucial aspect of this consideration is the potential for medication to affect the infant’s health.
The infant’s developing organs and systems are susceptible to the effects of medications, and the extent of this impact can vary significantly based on factors like the medication’s properties, the infant’s age, and the mother’s dosage.
Potential Effects of Medications in Breast Milk on Infants
Medications in breast milk can have a wide range of potential effects on infants. Some medications may cause minimal to no observable effects, while others can lead to noticeable side effects, requiring close monitoring. The infant’s immature liver and kidneys may not be equipped to process medications in the same way as an adult, potentially leading to higher concentrations of the medication in the infant’s bloodstream.
Potential Side Effects in Infants
Potential side effects in infants exposed to medications through breast milk can vary significantly depending on the medication. Common side effects might include digestive issues, such as diarrhea or vomiting, or neurological changes, like drowsiness or irritability. In some cases, more severe reactions, such as allergic reactions or respiratory problems, might occur. However, these reactions are usually rare.
Recognizing and understanding these potential side effects is critical for proper monitoring and management.
Comparing Benefits and Risks
Weighing the potential benefits of the mother’s medication against the potential risks to the infant is essential. The mother’s mental health is crucial, and medication can be vital for maintaining her well-being. A healthcare professional should evaluate the potential benefits of the medication for the mother against the potential risks to the infant, considering the specific medication, the infant’s age, and the mother’s dosage.
Open communication and careful monitoring are essential to mitigate any risks.
Managing Potential Infant Reactions
Prompt and appropriate management of potential infant reactions to medication exposure is crucial. Monitoring the infant for any signs of adverse effects is paramount. If any concerning symptoms arise, immediate contact with the pediatrician or healthcare provider is vital. A healthcare professional can provide guidance on managing the situation, potentially adjusting the mother’s medication dosage or frequency or providing alternative approaches.
Monitoring Procedures for Medication Exposure
Careful monitoring of the infant’s health is essential to identify any potential side effects. Regular check-ups with the pediatrician are critical, enabling the pediatrician to observe the infant’s development and detect any unusual reactions. Close observation of the infant for any signs of discomfort, changes in behavior, or physical symptoms is also crucial. These observations can be documented to track the infant’s progress and identify any patterns.
Examples of Medications and Potential Effects
| Medication | Potential Effects on Infant | Necessary Monitoring Procedures | Important Considerations |
|---|---|---|---|
| Codeine | Possible drowsiness, respiratory depression (especially in premature infants). | Close observation for respiratory distress, decreased activity, and feeding difficulties. Consult with the pediatrician regarding appropriate dosage and frequency. | Use cautiously in breastfeeding mothers. Alternative pain management options should be considered. |
| Antidepressants (e.g., SSRIs) | Possible irritability, feeding difficulties, or lethargy. | Monitor for changes in feeding patterns, mood, and overall behavior. Regular check-ups with the pediatrician. | Monitor closely for any signs of unusual behaviors. Consult with the pediatrician and the prescribing physician for the most appropriate medication and dosage. |
| Antibiotics (e.g., penicillin) | Generally considered safe in low doses, but possible allergic reactions. | Monitor for any signs of allergic reactions such as rash, hives, or difficulty breathing. | Monitor for potential impact on the gut microbiome. |
Final Review
In conclusion, breastfeeding while managing mental health concerns and medications is a multifaceted experience. While challenges are inevitable, the importance of support systems, open communication with healthcare professionals, and understanding the potential impacts on both mother and infant are paramount. This journey is unique to each individual, and my hope is that sharing my experience, along with others’, can provide valuable insight and encouragement to those facing similar situations.
Remember, you are not alone.