Narcolepsy and your brain: Understanding this sleep disorder requires delving into the neurological processes that govern sleep and wakefulness. This exploration will cover the fundamental mechanisms of narcolepsy, highlighting the specific brain regions affected and the neurotransmitter imbalances that cause its distinctive symptoms. We’ll also look at how narcolepsy disrupts the sleep-wake cycle and discuss diagnostic procedures and treatment options.
The journey into the intricate workings of the brain and the impact of narcolepsy on daily life is about to begin.
This detailed look at narcolepsy’s effects on the brain will unravel the complex interplay between brain regions, neurochemicals, and sleep patterns. We’ll compare and contrast narcolepsy with other sleep disorders to better understand its unique characteristics. By examining the various diagnostic methods and treatment strategies, we’ll provide a comprehensive understanding of this condition and its management.
Understanding Narcolepsy
Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness and disruptions in the brain’s control of sleep-wake cycles. It significantly impacts a person’s ability to function normally throughout the day, often leading to difficulties in maintaining employment, education, and social interactions. Understanding the underlying mechanisms and symptoms is crucial for effective management and support.
Fundamental Mechanisms of Narcolepsy
Narcolepsy stems from a complex interplay of genetic predisposition and environmental factors. The core issue lies in the malfunctioning of specific brain cells that produce the neurotransmitter hypocretin (orexin). These cells, primarily located in the hypothalamus, play a critical role in regulating wakefulness and preventing excessive sleep. In individuals with narcolepsy, these hypocretin neurons are either destroyed or malfunction, leading to a deficiency in the neurotransmitter.
This deficiency disrupts the normal sleep-wake cycle, resulting in the characteristic symptoms of narcolepsy.
Neurological Processes in Narcolepsy
The absence or dysfunction of hypocretin neurons disrupts the normal balance between wakefulness and sleep. This imbalance affects various neurological pathways involved in sleep regulation. The loss of hypocretin significantly impacts the brain regions responsible for coordinating rapid eye movement (REM) sleep and wakefulness. This disconnection contributes to the involuntary transitions between sleep and wakefulness, often resulting in cataplexy (sudden loss of muscle tone), hallucinations, and sleep paralysis.
Understanding narcolepsy is all about how your brain’s systems aren’t quite working in sync. Sometimes, helping kids overcome anxieties is remarkably similar; just like learning how to manage narcolepsy, parents can help anxious kids face their fears by teaching coping mechanisms and building confidence. how parents can help anxious kids face their fears provides practical strategies to support kids.
Ultimately, it’s all about understanding how the brain functions, whether it’s dealing with sleep disorders or childhood anxieties.
The exact mechanisms of how these disruptions manifest are still under investigation.
Types of Narcolepsy and Symptoms
Narcolepsy is categorized into different types, each with its unique symptom profile. The most common type is narcolepsy type 1, which typically involves cataplexy, sleep paralysis, and hypnagogic/hypnopompic hallucinations. Cataplexy manifests as sudden muscle weakness triggered by strong emotions, ranging from laughter to anger. Sleep paralysis involves the inability to move or speak upon falling asleep or waking up.
Hypnagogic and hypnopompic hallucinations are vivid sensory experiences that occur during the transition between wakefulness and sleep. Narcolepsy type 2 lacks cataplexy but exhibits the other symptoms. The variations in symptom presentation highlight the complex nature of the disorder.
Impact on Brain Function
Narcolepsy significantly impacts brain function by disrupting the normal sleep-wake cycle. The irregular sleep patterns often lead to cognitive impairment, such as difficulty concentrating, memory problems, and reduced alertness. These effects can vary from person to person, depending on the severity of the disorder and the individual’s response to treatment. The brain’s executive functions, responsible for planning, organizing, and problem-solving, can be affected, potentially leading to challenges in daily life.
Differences Between Narcolepsy and Other Sleep Disorders
Narcolepsy differs from other sleep disorders in its unique symptom profile, particularly the presence of cataplexy, sleep paralysis, and hypnagogic/hypnopompic hallucinations. Other sleep disorders, such as insomnia or sleep apnea, primarily involve difficulty falling or staying asleep, whereas narcolepsy is characterized by excessive daytime sleepiness and intrusions of sleep into wakefulness. Distinguishing narcolepsy from other sleep disorders requires a comprehensive evaluation of symptoms, sleep study results, and medical history.
Comparison of Narcolepsy with Other Sleep Disorders
| Disorder | Symptoms | Brain Regions Affected | Treatment |
|---|---|---|---|
| Narcolepsy | Excessive daytime sleepiness, cataplexy, sleep paralysis, hallucinations | Hypothalamus, brainstem, areas controlling REM sleep | Stimulants, antidepressants, lifestyle modifications |
| Insomnia | Difficulty falling or staying asleep | Areas regulating sleep-wake cycle, emotional centers | Cognitive behavioral therapy, sleep hygiene, medications |
| Sleep Apnea | Repeated pauses in breathing during sleep | Brainstem, respiratory centers | CPAP therapy, weight loss, surgery |
| Restless Legs Syndrome | Uncomfortable sensations in legs, urge to move them | Motor areas, sensory pathways | Medications, lifestyle changes |
Brain Regions Affected by Narcolepsy
Narcolepsy, a chronic sleep disorder, significantly impacts various brain regions, leading to a complex interplay of symptoms. Understanding these affected areas and the underlying neurochemical imbalances is crucial for comprehending the disorder’s multifaceted nature. This exploration will delve into the key brain regions involved, their specific functions, and the specific ways narcolepsy disrupts their normal operation.The intricate dance of neurotransmitters within the brain is essential for regulating our sleep-wake cycles.
In narcolepsy, this delicate balance is disrupted, primarily due to a deficiency in the neurotransmitter hypocretin (orexin). This deficiency cascades through the brain, affecting various regions and functions, resulting in the characteristic symptoms of narcolepsy.
Key Brain Regions Impacted
The brain regions most directly involved in narcolepsy are those responsible for regulating sleep-wake cycles, alertness, and motor control. These regions are interconnected and their dysfunction in narcolepsy creates a chain reaction, impacting various aspects of daily life.
Neurochemical Imbalances in Narcolepsy
The core neurochemical imbalance in narcolepsy revolves around the deficiency of hypocretin (orexin). This crucial neurotransmitter plays a vital role in regulating wakefulness and preventing excessive daytime sleepiness. A lack of hypocretin disrupts the normal functioning of the brain regions responsible for maintaining alertness, leading to the characteristic symptoms of narcolepsy. Hypocretin neurons are primarily located in the hypothalamus.
Hypothalamus and Sleep-Wake Regulation
The hypothalamus, a small but vital structure in the brain, acts as the central control center for many bodily functions, including sleep-wake cycles. It contains specialized neurons that produce and release hypocretin (orexin), which is critical for maintaining wakefulness. In narcolepsy, the loss of these hypocretin-producing neurons in the hypothalamus disrupts the intricate interplay of neurochemicals and brain regions, contributing to the disorder’s characteristic symptoms.
Relationship Between Affected Brain Regions and Symptoms
| Brain Region | Function | Narcolepsy Impact | Symptoms |
|---|---|---|---|
| Hypothalamus | Regulates sleep-wake cycles, hunger, thirst, body temperature | Loss of hypocretin-producing neurons, disrupting sleep-wake balance | Excessive daytime sleepiness, cataplexy, sleep paralysis, hallucinations |
| Brainstem | Controls vital functions like breathing and heart rate, relays sensory information | Affected by the disrupted sleep-wake cycle, impacting alertness | Sleep attacks, abrupt loss of muscle tone (cataplexy) |
| Cerebellum | Coordinates movement and balance | Disruption of hypocretin pathways affecting motor control | Possible coordination problems, difficulty with motor tasks |
| Amygdala | Processes emotions, especially fear | Possible altered emotional responses due to the lack of neurotransmitter balance | Hallucinations, emotional lability |
Neurotransmitters and Narcolepsy
Understanding the intricate dance of neurotransmitters is crucial to comprehending narcolepsy. These chemical messengers act as vital communication signals within the brain, orchestrating various functions, including sleep-wake regulation. Disruptions in these intricate pathways can lead to significant neurological disorders, and narcolepsy is a prime example of this phenomenon.Neurotransmitter imbalances play a central role in the pathophysiology of narcolepsy.
Specifically, the disruption of specific neurotransmitter systems, particularly those involved in regulating arousal and sleep, leads to the characteristic symptoms observed in individuals with this condition. These imbalances manifest as a dysregulation of the brain’s sleep-wake cycle, resulting in excessive daytime sleepiness and cataplexy, among other symptoms.
The Role of Neurotransmitters in Normal Sleep-Wake Cycles
Neurotransmitters are essential for maintaining a healthy sleep-wake cycle. They act as chemical messengers, transmitting signals between neurons, influencing various brain regions responsible for arousal, sleep onset, and maintenance. The precise interplay of these neurotransmitters creates a delicate balance that regulates our natural sleep-wake rhythm. For instance, norepinephrine and histamine are key players in promoting wakefulness, while GABA and adenosine promote sleep.
A disruption in this delicate balance can lead to sleep disorders, like narcolepsy.
Neurotransmitter Imbalances in Narcolepsy
Narcolepsy is characterized by significant imbalances in specific neurotransmitter systems, primarily involving the neurotransmitter orexin. The dysfunction in these systems is linked to the underlying cause of the disorder. Orexin, often referred to as hypocretin, is a crucial neurotransmitter for maintaining wakefulness. A deficiency in orexin is a hallmark of narcolepsy, resulting in a compromised ability to regulate the sleep-wake cycle.
This deficiency allows sleep-related processes to inappropriately occur during wakefulness, causing symptoms like cataplexy and sleep attacks.
Specific Neurotransmitters Affected in Narcolepsy
The most prominent neurotransmitter affected in narcolepsy is orexin (hypocretin). Orexin plays a critical role in promoting wakefulness and regulating various aspects of sleep. Its deficiency in narcolepsy is associated with the excessive daytime sleepiness characteristic of the disorder. Furthermore, the disruption in orexin pathways leads to a cascade of effects on other neurotransmitter systems, contributing to the wide range of symptoms experienced by individuals with narcolepsy.
Other neurotransmitters, like serotonin, dopamine, and histamine, also play a role, though their exact involvement is still under investigation.
Summary Table: Key Neurotransmitters in Narcolepsy
| Neurotransmitter | Normal Function | Narcolepsy Impact | Symptoms |
|---|---|---|---|
| Orexin (Hypocretin) | Promotes wakefulness, regulates appetite, and plays a role in learning and memory. | Severe deficiency; crucial for maintaining wakefulness. Its absence disrupts the brain’s sleep-wake regulatory mechanisms. | Excessive daytime sleepiness, cataplexy, sleep paralysis, hypnagogic hallucinations. |
| GABA | Inhibitory neurotransmitter; crucial for promoting relaxation and sleep. | Potential imbalance; might contribute to excessive sleepiness or disrupted sleep stages. | Possible sleep disturbances, but the exact role is not fully understood. |
| Norepinephrine | Promotes wakefulness, alertness, and focus. | Possible dysfunction; might be affected by orexin deficiency, contributing to daytime sleepiness. | Excessive daytime sleepiness, difficulty concentrating, impaired alertness. |
| Histamine | Promotes wakefulness and alertness. | Potential disruption; likely affected by orexin deficiency, influencing wakefulness. | Excessive daytime sleepiness, impaired alertness, difficulty staying awake. |
Sleep-Wake Cycle Disruptions
Narcolepsy significantly disrupts the normal sleep-wake cycle, leading to a complex interplay of excessive daytime sleepiness and unusual sleep patterns. These disruptions aren’t simply a matter of feeling tired; they involve fundamental changes in the brain’s activity during sleep and wakefulness. Understanding these changes is crucial for diagnosis and effective management of this challenging condition.The sleep-wake cycle in narcolepsy is characterized by a profound mismatch between the body’s internal clock and its need for sleep.
This leads to an irregular and unpredictable sleep-wake schedule, impacting daily life significantly. The underlying neurological mechanisms responsible for this disruption involve imbalances in specific neurotransmitters, primarily impacting the sleep stages.
Disruptions in Sleep Stages
The typical sleep cycle consists of several stages, each characterized by unique brainwave patterns and physiological responses. In narcolepsy, these stages are often disrupted, leading to intrusions of REM sleep (Rapid Eye Movement) into wakefulness. This is a crucial factor differentiating narcolepsy from other sleep disorders.
| Sleep Stage | Normal Brain Activity | Narcolepsy Disruption | Symptoms |
|---|---|---|---|
| Wakefulness | High-frequency, low-amplitude brain waves. Brain is active, processing information. | Sudden, unexpected transitions to sleep (sleep attacks). Difficulty staying awake, especially in monotonous situations. | Excessive daytime sleepiness, sudden lapses into sleep, cataplexy (loss of muscle tone). |
| Non-REM Stage 1 | Transitional stage between wakefulness and sleep, characterized by slowing brain waves. | Possible intrusion of REM sleep characteristics (hallucinations, hypnagogic/hypnopompic hallucinations). | Sleep paralysis, vivid dreams just before or after sleep, fragmented sleep. |
| Non-REM Stages 2-4 | Progressive slowing of brain waves, deep sleep. Important for physical restoration. | Possible disruption of deep sleep, fragmented sleep, less restorative sleep. | Difficulty reaching deep sleep, waking up feeling unrested, sleep inertia. |
| REM Sleep | High-frequency brain waves similar to wakefulness, associated with dreaming. Important for cognitive function. | Sudden and unexpected transitions into REM sleep during wakefulness, known as cataplexy, or brief episodes of paralysis. | Cataplexy, sleep paralysis, vivid dreams. |
Role of Circadian Rhythm
The circadian rhythm, the internal biological clock regulating sleep-wake cycles, plays a critical role in narcolepsy. Disruptions in this rhythm can contribute to the excessive daytime sleepiness and unpredictable sleep patterns seen in narcolepsy. The body’s natural sleep-wake cycle is often out of sync with the external environment. This can lead to difficulties with regulating sleep times and consistency.For example, individuals with narcolepsy might experience a strong urge to sleep at unusual times, regardless of their daily schedule.
This is because the circadian rhythm, which normally regulates sleep-wake cycles, is affected. A misalignment between the circadian rhythm and the sleep-wake cycle can lead to a variety of symptoms, including excessive daytime sleepiness and difficulty maintaining regular sleep patterns.
Understanding narcolepsy involves looking at how your brain’s reward system and sleep-wake cycles are affected. This can sometimes mirror the complex challenges faced by long haul breast cancer survivors, like the exhaustion and brain fog described in articles like long haul for breast cancer survivors. Ultimately, both situations highlight how debilitating chronic conditions can impact the brain’s function and overall well-being.
Diagnostic Procedures and Tests

Unraveling the mystery of narcolepsy often begins with a thorough diagnostic process. A combination of patient history, physical examination, and specialized sleep studies are crucial in confirming a diagnosis and ruling out other potential conditions. This meticulous approach ensures accurate identification and tailored treatment plans.The diagnostic journey for narcolepsy involves a careful evaluation of symptoms, lifestyle factors, and medical history.
This process is designed to differentiate narcolepsy from other sleep disorders and medical conditions that may present with similar symptoms. Understanding the specific patterns and frequency of symptoms is essential for accurate diagnosis.
Diagnostic Procedures
A comprehensive evaluation typically begins with a detailed discussion of the patient’s symptoms. This includes a thorough history of sleep patterns, daytime sleepiness, cataplexy episodes, hallucinations, and other related experiences. Physicians also consider any medications or underlying medical conditions that might contribute to the symptoms. A physical examination is often conducted to rule out any other potential causes of the symptoms.
Sleep Studies
Sleep studies play a vital role in diagnosing narcolepsy. These studies meticulously monitor various physiological parameters during sleep to identify patterns and abnormalities. Different types of sleep studies provide valuable insights into sleep architecture and behavior.
Polysomnography
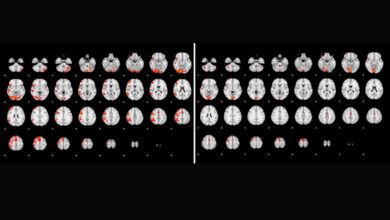
Polysomnography (PSG) is a cornerstone of sleep studies. It records various physiological signals, including brain waves (EEG), eye movements (EOG), muscle activity (EMG), and heart rate. PSG helps evaluate sleep stages and identify potential sleep disorders. The data collected during PSG is crucial for evaluating the quality and quantity of sleep, revealing any disruptions or unusual patterns.
- Electroencephalography (EEG): Measures electrical activity in the brain, revealing sleep stages and potential abnormalities. Variations in brainwave patterns during different sleep stages can suggest underlying sleep disorders.
- Electrooculography (EOG): Tracks eye movements during sleep. Rapid eye movements (REM) are typically associated with dreaming and can be affected in certain sleep disorders.
- Electromyography (EMG): Monitors muscle activity during sleep. The absence of muscle tone during REM sleep, or unusual muscle activity, can point to specific sleep disorders.
- Electrocardiogram (ECG): Monitors heart activity, helping identify any cardiac issues that might be contributing to sleep disturbances or daytime sleepiness.
- Respiratory Monitoring: Tracks breathing patterns during sleep, identifying potential sleep-related breathing disorders. Apnea events, for example, might affect sleep quality and contribute to daytime fatigue.
The data obtained from PSG is analyzed to determine sleep efficiency, latency to sleep onset, and presence of sleep disorders. Quantitative analysis of sleep stages and characteristics of sleep episodes provide insights into the quality and architecture of sleep. A comprehensive sleep study report typically includes graphs and charts visualizing the data, allowing physicians to interpret and evaluate the collected information.
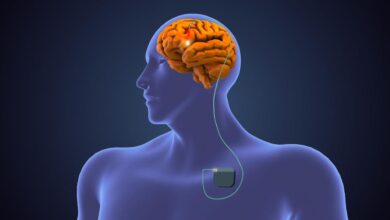
Understanding narcolepsy involves looking at how it affects your brain’s complex control systems. One potential avenue for treatment, like deep brain stimulation DBS , is being explored for its ability to target specific brain regions impacting the regulation of sleep and wakefulness. Ultimately, though, the focus must always return to understanding and managing the specific ways narcolepsy disrupts your brain’s natural functions.
Flowchart of Diagnostic Process
This flowchart illustrates the diagnostic process, highlighting different paths based on sleep study results.
| Step | Action | Possible Results | Next Step |
|---|---|---|---|
| 1 | Patient history and physical examination | Suspected narcolepsy | Proceed to sleep study |
| 2 | Sleep study (Polysomnography) | Presence of REM sleep abnormalities, such as cataplexy, or short sleep latency to REM | Further testing to confirm narcolepsy and rule out other disorders |
| 2 | Sleep study (Polysomnography) | No evidence of narcolepsy | Rule out other sleep disorders or medical conditions |
| 3 | Further testing | Confirmed narcolepsy | Diagnosis of narcolepsy and treatment plan |
| 3 | Further testing | Other sleep disorders or medical conditions | Diagnosis of the identified disorder and treatment plan |
Treatment Strategies: Narcolepsy And Your Brain
Navigating narcolepsy requires a multi-faceted approach that goes beyond simply managing symptoms. Effective treatment involves a combination of lifestyle adjustments, medication, and sometimes, even psychological support. Understanding the specific needs of each individual is key to finding a personalized strategy for optimal well-being.Treatment for narcolepsy focuses on mitigating the impact of the sleep-wake cycle disruptions and controlling the cataplexy episodes.
This approach recognizes the complex interplay between the brain’s neurochemical imbalances and the patient’s overall lifestyle. A comprehensive treatment plan considers not only the immediate symptoms but also the long-term implications of the disorder.
Medications for Narcolepsy
Medications play a crucial role in managing narcolepsy symptoms. They aim to regulate neurotransmitter levels, promote stable sleep patterns, and reduce the frequency and severity of cataplexy episodes. Stimulants, such as modafinil and methylphenidate, are frequently prescribed to combat daytime sleepiness. These medications can improve alertness and cognitive function, allowing individuals to engage in daily activities more effectively.
Managing Daytime Sleepiness
Addressing daytime sleepiness is a key component of narcolepsy management. Strategies include consistent sleep schedules, regular exercise, and optimizing sleep hygiene. Napping strategically, even for short periods, can also be beneficial in mitigating the effects of sleep deprivation. Lifestyle modifications often complement medication regimens, creating a more comprehensive approach to symptom management. For example, a consistent sleep schedule of 7-9 hours per night, combined with regular exercise, can help regulate the body’s natural sleep-wake cycle.
Different Treatment Approaches
Various treatment approaches exist, each with its own set of benefits and drawbacks. The efficacy of a particular treatment depends on the individual’s specific symptoms and response to the medication. A combination of treatments, including medication and lifestyle adjustments, is often the most effective strategy for managing narcolepsy.
Treatment Options and Potential Side Effects
| Treatment | Mechanism | Potential Benefits | Potential Drawbacks |
|---|---|---|---|
| Modafinil (e.g., Provigil) | Increases wakefulness by affecting neurotransmitters, particularly dopamine and histamine | Improved daytime alertness, reduced sleepiness, and enhanced cognitive function. | Potential for headache, nausea, anxiety, insomnia, and allergic reactions. May not be effective for all individuals. |
| Methylphenidate (e.g., Ritalin) | Increases wakefulness by stimulating neurotransmitters, primarily dopamine and norepinephrine | Effective in reducing daytime sleepiness and improving attention. | Potential for anxiety, nervousness, insomnia, decreased appetite, and potential for dependence. |
| Sodium oxybate (e.g., Xyrem) | Increases levels of hypocretin in the brain, which plays a vital role in wakefulness and sleep regulation. | Effective in reducing cataplexy episodes, improving sleep quality, and managing daytime sleepiness. | Potential for side effects such as headache, nausea, and difficulty with coordination. It requires careful monitoring and dosage adjustment. |
| Antidepressants (e.g., selective serotonin reuptake inhibitors – SSRIs) | Affect neurotransmitters involved in mood regulation and cataplexy. | Can help manage cataplexy episodes and improve mood in some cases. | Potential for side effects like nausea, anxiety, and sexual dysfunction. May not be as effective in controlling daytime sleepiness as stimulants. |
Impact on Daily Life
Navigating daily life with narcolepsy can present unique and often significant challenges. The unpredictable nature of the condition, including excessive daytime sleepiness, cataplexy, and sleep paralysis, can impact various aspects of an individual’s routine and well-being. Understanding these impacts is crucial for developing effective coping strategies and support systems.Living with narcolepsy requires adaptation and resilience. Individuals often find themselves needing to modify their routines and expectations to accommodate the fluctuating nature of their symptoms.
This can involve careful planning, adjustments to work schedules, and seeking support from loved ones and healthcare professionals.
Challenges in Daily Activities
The unpredictable nature of narcolepsy can make many daily activities difficult. Episodes of sudden sleep attacks can occur at inopportune moments, disrupting work, school, or social engagements. Cataplexy, the sudden loss of muscle tone, can be embarrassing or even dangerous in certain situations. Sleep paralysis, the inability to move or speak when falling asleep or waking up, can be frightening and disruptive to sleep.
Social and Emotional Implications
Narcolepsy can have significant social and emotional implications. The unpredictable nature of symptoms can lead to social isolation or strained relationships with friends and family. Embarrassment and frustration associated with symptoms can impact self-esteem and confidence. The condition can also create feelings of anxiety and depression, particularly if symptoms are poorly managed or if the individual feels misunderstood.
Importance of Support Systems
Strong support systems are essential for individuals living with narcolepsy. These systems can include family members, friends, support groups, and healthcare professionals. The emotional and practical support provided by these networks can significantly improve the quality of life for someone with narcolepsy. Sharing experiences and coping strategies with others facing similar challenges can foster a sense of community and understanding.
Coping Mechanisms and Strategies
Developing effective coping mechanisms is crucial for managing the impact of narcolepsy on daily life. Strategies may include establishing a regular sleep schedule, incorporating short naps into the daily routine, and practicing stress-reduction techniques. Maintaining a healthy diet, engaging in regular exercise, and avoiding stimulants can also contribute to better symptom management.
Support Resources and Organizations
Numerous organizations offer support and resources for individuals with narcolepsy and their families. These resources include information about the condition, support groups, and connections with other individuals facing similar challenges. Access to educational materials and expert advice is vital for navigating the condition.
- The National Sleep Foundation provides valuable information on sleep disorders, including narcolepsy, and offers resources for patients and healthcare providers.
- The American Academy of Sleep Medicine offers educational materials and guidelines for diagnosing and treating sleep disorders.
- Narcolepsy Support Groups: These groups provide a platform for sharing experiences, coping strategies, and building a supportive community.
- Online forums and social media groups can connect individuals with narcolepsy to share information and support.
- Local support groups can offer a sense of community and provide opportunities to connect with others who understand the challenges.
Illustrative Brain Activity
Understanding brain activity, particularly during sleep and wakefulness, is crucial for comprehending narcolepsy. This involves looking at the electrical patterns generated by neurons, which can be measured using electroencephalography (EEG). These patterns reveal the brain’s state and can highlight differences between healthy individuals and those with narcolepsy.Brain activity, both during sleep and wakefulness, is a complex interplay of electrical signals.
Normal sleep involves distinct stages, each characterized by different EEG patterns. Narcolepsy disrupts this natural rhythm, leading to unusual brain activity during sleep and wakefulness.
Typical Brain Activity During Sleep
Sleep stages are characterized by specific EEG patterns. During non-REM sleep, brain waves become slower and more synchronized. REM sleep, on the other hand, is characterized by rapid eye movements and vivid dreams, accompanied by more desynchronized, faster brain waves. The brain undergoes a cyclical transition between these stages throughout the night. This cyclic activity is vital for memory consolidation, restoration, and overall cognitive function.
Brain Activity in Narcolepsy During Sleep and Wakefulness
Narcolepsy presents a significant deviation from typical brain activity. During sleep, individuals with narcolepsy may exhibit an unusual mix of REM and non-REM sleep stages. They might enter REM sleep very quickly, which can manifest as sleep paralysis or hallucinations. Even during wakefulness, there can be intrusions of sleep-related brainwave patterns, leading to sudden lapses in alertness.
The brain’s ability to maintain a stable, consistent sleep-wake cycle is significantly impaired.
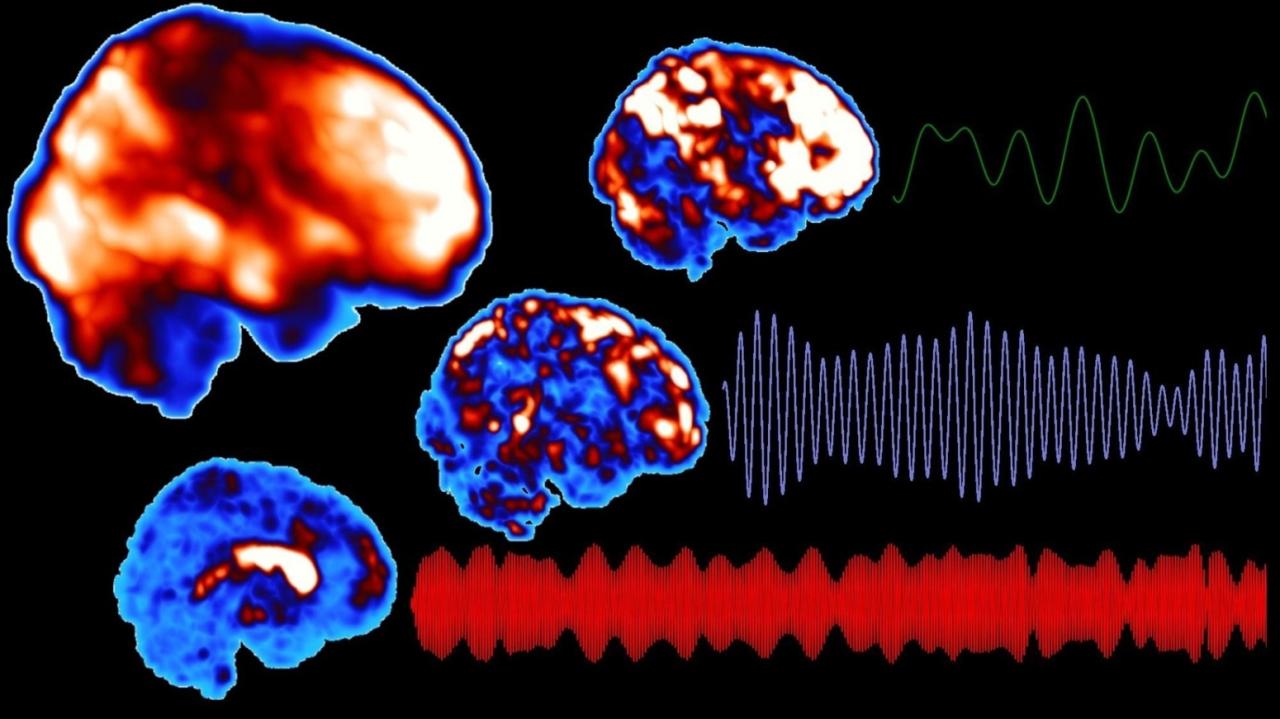
Brain Activity During REM Sleep: Healthy vs. Narcolepsy
This illustration depicts a simplified representation of EEG activity during REM sleep. The top graph represents a healthy individual, showing typical REM sleep patterns with distinct desynchronized brain waves. The bottom graph represents an individual with narcolepsy, exhibiting a more erratic and fragmented pattern of brain waves. The narcolepsy pattern shows frequent transitions between REM and non-REM sleep stages, or even periods of brain activity that are more indicative of wakefulness, even during the REM sleep phase.
This indicates a disturbance in the brain’s ability to regulate the transition between sleep stages.
| Brain Activity | Healthy Individual | Individual with Narcolepsy |
|---|---|---|
| REM Sleep | Regular, rhythmic, desynchronized brain waves. | Irregular, fragmented brain waves, showing frequent transitions between sleep stages. |
Brain Activity During a Narcolepsy Cataplexy Attack, Narcolepsy and your brain
A cataplexy attack involves a sudden loss of muscle tone, triggered by strong emotions or physical exertion. Brain activity during a cataplexy attack is characterized by a temporary suppression of normal brain activity associated with muscle control. There is a sudden shift in the brain’s activity, a significant reduction in the typical patterns associated with voluntary movement, and an increase in slow-wave activity, reflecting a temporary state akin to sleep.
This sudden drop in muscle tone is not directly caused by a lack of consciousness. The brain, in a way, momentarily loses control over the muscles.
Conclusion
In conclusion, narcolepsy presents a fascinating and challenging case study in understanding the brain’s intricate regulation of sleep and wakefulness. The multifaceted nature of this condition, encompassing neurotransmitter imbalances, disrupted sleep-wake cycles, and significant impacts on daily life, underscores the importance of accurate diagnosis and effective treatment. This exploration provides valuable insights into the complex relationship between the brain and sleep, ultimately emphasizing the need for continued research and support for those affected.