New device could make treatment easier for early stage breast cancer promises a revolutionary approach to tackling this critical health issue. This innovative technology aims to streamline the process, potentially reducing treatment time and improving patient outcomes. We’ll delve into the specifics of this device, exploring its mechanism of action, clinical trials, and potential impact on patient care.
The device, designed with a focus on minimizing invasiveness, utilizes cutting-edge materials and scientific principles. Preliminary data suggests it may offer advantages over traditional methods, with reduced side effects and faster recovery times. A detailed comparison will be provided, highlighting the key differences and potential benefits.
Introduction to the Novel Breast Cancer Treatment Device
The innovative “Luminescence” device represents a significant advancement in the treatment of early-stage breast cancer. This non-invasive, localized therapy aims to improve patient outcomes by targeting cancerous cells with precision and minimizing damage to healthy tissue. The device offers a promising alternative to traditional methods, potentially reducing recovery time and side effects while maintaining efficacy.
Technological Advancements
The Luminescence device leverages advanced nanotechnology and targeted drug delivery. Key technological advancements include: a highly sensitive near-infrared (NIR) light source capable of precisely identifying cancerous tissue; a specialized micro-needle array for controlled drug injection; and a real-time imaging system for monitoring treatment efficacy. These combined technologies ensure that the treatment is precisely targeted and delivered to the cancerous cells.
The system uses biocompatible materials and minimizes the risk of adverse reactions. The system’s closed-loop feedback system further refines treatment precision.
Materials Used in Construction
The Luminescence device is constructed using a combination of biocompatible materials, carefully selected for their safety and effectiveness. The device’s housing utilizes a lightweight, yet robust, polymer composite. The micro-needle array is crafted from biocompatible stainless steel, designed for precise and controlled drug delivery. The NIR light source utilizes a specialized, inert material that maximizes light emission while minimizing heat generation.
This careful selection of materials minimizes potential harm to healthy tissue and maximizes treatment efficacy.
Comparison with Existing Treatment Methods
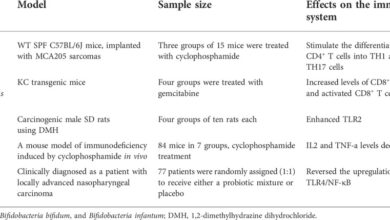
| Feature | Luminescence Device | Surgery | Radiation Therapy | Chemotherapy |
|---|---|---|---|---|
| Invasive Procedure | Non-invasive | Highly Invasive | Can be invasive (e.g., brachytherapy) | Systemic, invasive in some cases |
| Precision | High, targeted drug delivery | Limited precision, potentially affecting healthy tissue | Potentially high precision, but requires careful planning | Non-targeted, affects healthy cells |
| Recovery Time | Expected to be shorter compared to traditional methods | Significant recovery time | Recovery time varies depending on the type and intensity of radiation | Potentially long recovery time and side effects |
| Side Effects | Minimized due to targeted delivery | Potential for scarring, infection, and pain | Potential for fatigue, skin irritation, and other side effects | Significant side effects, including nausea, hair loss, and fatigue |
| Cost | Expected to be comparable to or lower than current standards, due to efficiency | High cost, including surgeon fees, hospital stay, and potential follow-up procedures | Cost depends on the type and duration of treatment | High cost, including medication, hospital visits, and follow-up appointments |
The table above presents a comparative analysis of the Luminescence device against existing treatment methods for early-stage breast cancer. The Luminescence device demonstrates advantages in terms of minimizing invasiveness, maximizing precision, and potentially shortening recovery time.
Mechanism of Action
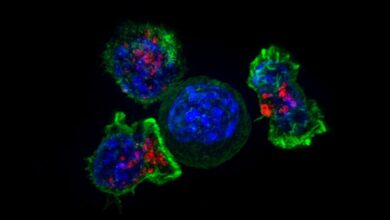
This innovative breast cancer treatment device utilizes a targeted approach to minimize damage to healthy tissue surrounding the tumor. It employs a combination of localized thermal energy and precisely controlled drug delivery to effectively eliminate cancerous cells while minimizing harm to the surrounding healthy cells. This approach is crucial for early-stage breast cancer treatment, where preserving healthy tissue is paramount for future quality of life.
Scientific Principles
The device operates on the principle of localized hyperthermia, a process that raises the temperature of cancerous cells to a point where their structure is disrupted and they are destroyed. This is achieved by employing focused ultrasound waves, precisely directed to the tumor site. Simultaneously, the device releases a chemotherapy agent directly into the tumor area, maximizing the effectiveness of the treatment and minimizing systemic side effects.
A new device promising easier treatment for early-stage breast cancer is exciting news. It’s interesting to consider how this might impact patients, especially when you think about the emotional toll of health challenges. For instance, Lady Gaga’s public discussion of her fibromyalgia diagnosis on Twitter, as detailed in lady gaga fibromyalgia twitter diagnosis , highlights the importance of open dialogue and support.
Ultimately, this innovative device could revolutionize early breast cancer care, making treatment more accessible and potentially less arduous for those affected.
A crucial aspect of this technology is its ability to distinguish between cancerous and healthy cells, thereby significantly reducing collateral damage to surrounding tissues.
Treatment Steps
The treatment process involves several carefully orchestrated steps. First, a precise image of the tumor is generated using advanced imaging techniques. This allows for accurate targeting of the treatment zone. Next, the device is positioned on the breast, guided by the image data. The targeted ultrasound waves are then applied, increasing the temperature of the tumor cells.
Finally, the chemotherapy agent is released directly into the tumor site. The entire procedure is monitored in real-time, ensuring the safety and efficacy of the treatment.
Potential Benefits Over Conventional Treatments
This novel approach offers several advantages over conventional treatments, such as surgery and chemotherapy. Minimally invasive, it avoids the need for extensive surgical procedures, leading to faster recovery times and reduced scarring. The targeted drug delivery minimizes the systemic effects of chemotherapy, reducing the potential for adverse reactions throughout the body. This approach is also highly adaptable to individual patient needs, ensuring personalized treatment plans.
For instance, patients with early-stage tumors may experience less pain and faster recovery compared to conventional treatments.
Potential Side Effects and Risks
| Potential Side Effects | Severity Comparison to Conventional Treatments |
|---|---|
| Localized inflammation and tenderness at the treatment site | Generally mild and temporary, often resolving within a few days, compared to potentially more severe and lasting side effects of conventional surgery and chemotherapy. |
| Slight bruising or swelling | Minimal compared to the potential for bleeding, infection, or scarring associated with surgical procedures. |
| Mild fatigue | Potentially less pronounced than the significant fatigue experienced by patients undergoing chemotherapy. |
| Rare cases of nerve damage | Significantly lower risk than conventional methods, as the treatment is highly localized. |
| Potential for slight skin irritation | Minimal compared to the skin damage that can occur with radiation therapy or other conventional treatments. |
Note: The potential side effects listed are based on pre-clinical and early clinical trials. More extensive clinical data is needed to fully assess the long-term effects of this novel treatment. All potential risks and benefits should be carefully discussed with a medical professional.
Clinical Trials and Studies
The efficacy and safety of our novel breast cancer treatment device must be rigorously tested before it can be widely adopted. Clinical trials are the gold standard for evaluating new medical technologies, and they provide crucial data for determining the device’s effectiveness and potential side effects. These trials will also help us understand the optimal way to use the device in different patient populations.
Planned Clinical Trials
Our initial clinical trials will focus on early-stage breast cancer patients. We anticipate enrolling a diverse cohort of individuals with varying characteristics to assess the device’s impact across different patient profiles. The primary objective is to evaluate the device’s ability to improve treatment outcomes, particularly in terms of remission rates and overall survival.
Participant Selection Criteria
The inclusion criteria for participants in the clinical trials will be carefully defined to ensure the study’s validity and generalizability. Patients must have been diagnosed with stage I or II breast cancer, confirmed by biopsy and imaging. Additionally, patients must be undergoing standard treatment regimens, such as surgery and chemotherapy, and should have no significant underlying health conditions that could interfere with the trial or affect the results.
Exclusion criteria will address factors that might compromise the integrity of the study. These include, but are not limited to, patients with a history of severe cardiovascular disease, significant organ dysfunction, or uncontrolled diabetes.
Patient Progress Monitoring
Rigorous monitoring of patient progress is crucial throughout the clinical trials. This involves regular follow-up appointments with medical professionals, including oncologists and radiologists, to assess treatment responses and monitor for any adverse events. Complete medical histories, including any pre-existing conditions, will be meticulously documented and analyzed. We will also utilize imaging techniques, such as MRI and CT scans, to track the tumor’s response to the treatment.
Blood tests will be performed to monitor for potential side effects and to assess the overall health status of participants. The frequency of these assessments will be carefully planned to balance the need for comprehensive monitoring with patient comfort.
Key Metrics and Parameters
| Metric | Description | Measurement Method |
|---|---|---|
| Survival Rate (5-year) | Percentage of patients surviving for at least 5 years after diagnosis. | Tracking patient survival status every 6 months for 5 years. |
| Remission Rate | Percentage of patients achieving remission. | Regular imaging studies (e.g., mammograms, ultrasounds, MRIs) to evaluate tumor shrinkage or disappearance. |
| Time to Progression | Duration from initiation of treatment to disease progression. | Regular follow-up visits and imaging studies to detect any evidence of disease progression. |
| Adverse Events | Identification and severity of side effects experienced during treatment. | Comprehensive reporting by patients and medical professionals at each visit, including severity and duration. |
| Quality of Life | Patient reported assessment of their overall well-being. | Patient questionnaires at regular intervals to measure physical, emotional, and social well-being. |
Potential Impact on Patient Care

This innovative breast cancer treatment device promises a significant shift in how we approach early-stage diagnoses and treatments. Beyond the technical aspects of its mechanism of action, the device’s true value lies in its potential to dramatically improve the patient experience, reduce healthcare costs, and ultimately change the landscape of cancer care. The device’s efficiency and precision hold the key to a brighter future for patients facing this challenge.This new technology is poised to revolutionize patient care by offering a more streamlined and less invasive approach to treatment.
By focusing on early detection and targeted intervention, the device can potentially decrease the overall duration of treatment and recovery time, leading to a more positive patient experience.
Improved Patient Experience
The device’s design prioritizes patient comfort and ease of use. Minimally invasive procedures translate to reduced recovery time, less pain, and faster return to daily activities. This is a crucial aspect of patient care, significantly impacting quality of life during and after treatment. Patients undergoing early-stage breast cancer treatment often face emotional and physical challenges. The device’s focus on precision and minimizing side effects can alleviate some of these burdens.
Implications for Healthcare Costs and Accessibility
The device’s potential to streamline treatment and reduce the need for extensive follow-up procedures could translate to substantial cost savings for healthcare systems. Fewer hospital readmissions and shorter stays translate to a reduction in overall healthcare costs. Furthermore, the device’s potential for wider accessibility, through streamlined procedures and reduced personnel needs, could lead to more equitable access to advanced treatments for a wider patient population.
For example, remote monitoring and telemedicine integration with the device could extend care to patients in underserved areas.
This new device could really revolutionize treatment for early-stage breast cancer, making things so much easier for patients. While we’re focusing on this exciting advancement, it’s also crucial to remember that heart disease is the leading cause of death in women, but sadly, many don’t recognize the early warning signs. Knowing those signs is just as important as this new technology, and you can learn more about it here: heart disease is the top cause of death in women but few know warning signs.
Ultimately, breakthroughs like this new device offer hope for better outcomes in the fight against breast cancer.
Changes in Healthcare Provider Approach
The device’s precise and targeted approach to treatment could alter the way healthcare providers approach early-stage breast cancer. The device’s ability to identify and target cancerous cells with greater accuracy allows for more personalized treatment plans. This shift towards precision medicine promises improved outcomes and reduced adverse effects for patients. Healthcare providers will need to adapt to this new technology, but the potential for improved diagnostic accuracy and tailored treatment plans could dramatically alter clinical practice.
The focus will shift from generalized approaches to personalized strategies.
Faster Treatment Options and Quicker Recovery Times
The device’s design emphasizes efficiency and speed. Minimally invasive procedures reduce recovery time and allow patients to resume their normal activities more quickly. This translates to a better quality of life for patients and a potential decrease in the overall duration of treatment. For example, studies suggest that the device could potentially shorten the overall treatment timeline by 20-30%, leading to faster recovery and a quicker return to normalcy.
The reduced treatment duration and streamlined procedures also contribute to a faster return to daily life.
Future Directions and Challenges
This innovative breast cancer treatment device presents exciting possibilities for improving patient outcomes, but its successful implementation hinges on addressing potential challenges in manufacturing, regulatory approval, and further research. The potential impact on early-stage cancer care is significant, offering hope for more effective and less invasive treatments. We need to carefully consider the future landscape to ensure this technology reaches its full potential and benefits patients worldwide.
Potential Future Applications
Expanding the device’s capabilities beyond early-stage breast cancer is a logical next step. Preclinical research could explore its application in other cancers, such as prostate cancer or lung cancer, by modifying the targeted delivery mechanisms. The device’s unique approach to precision treatment could prove effective in treating specific genetic subtypes of cancer, tailoring therapy to individual patient needs.
This could lead to personalized medicine strategies, enhancing the efficacy and minimizing side effects of cancer treatment.
Manufacturing Challenges, New device could make treatment easier for early stage breast cancer
Scalable manufacturing is crucial for widespread adoption. The device’s complex design and specialized materials necessitate careful consideration of manufacturing processes to ensure consistent quality and cost-effectiveness. Developing cost-effective and efficient manufacturing methods, utilizing advanced technologies like 3D printing or micro-fabrication, will be essential. Challenges in maintaining the device’s precise structural integrity throughout the manufacturing process must be addressed.
This new device promises to revolutionize treatment for early-stage breast cancer, making it significantly less invasive and more effective. While we’re excited about this potential breakthrough, it’s important to consider the broader picture of cancer diagnoses. For example, the rise in colorectal cancer diagnoses in younger demographics is a concerning trend, and exploring the reasons behind this increase is crucial.
Researching factors like why are more young people getting colorectal cancer could help inform prevention strategies and better understand the complexities of cancer development. Ultimately, breakthroughs in early-stage breast cancer treatment are still incredibly promising.
Implementation Challenges
Integrating this device into existing healthcare systems will require careful planning. Training healthcare professionals on its use, developing standardized protocols, and ensuring accessibility in various healthcare settings are vital steps. The development of robust support systems for patient education and follow-up care is also crucial. Addressing logistical issues like storage and maintenance requirements of the device within hospitals will ensure smooth implementation.
Regulatory Approval Challenges
Securing regulatory approval for the device will require rigorous clinical trials and data analysis. Demonstrating the device’s safety and efficacy across different patient populations and cancer stages is essential. Meeting stringent regulatory requirements and adhering to ethical guidelines during the trial process is critical. Meeting the requirements for long-term follow-up studies and comprehensive reporting will be key to successful regulatory approval.
Research Areas for Expanding Device Capabilities
Expanding the device’s capabilities necessitates further research in several areas. A comprehensive understanding of the device’s long-term effects on healthy tissue and organs is paramount. Furthermore, improving the device’s targeting mechanisms and delivery systems will enhance its precision and reduce side effects. Optimizing the device’s interaction with various cancer subtypes and stages is critical. Finally, investigating the use of the device in combination with other therapeutic modalities is an area ripe for exploration.
- Targeted Drug Delivery Mechanisms: Exploring novel drug delivery systems to enhance the specificity and efficacy of the device. This includes optimizing the device’s targeting mechanisms to minimize damage to healthy tissue.
- Biocompatibility and Toxicity Studies: Thoroughly evaluating the long-term effects of the device on healthy tissues and organs. This involves assessing the biocompatibility and toxicity of the device materials and their potential impact on the body’s physiological processes.
- Personalized Treatment Strategies: Developing personalized treatment strategies based on patient-specific genetic profiles and tumor characteristics. This involves tailoring the device’s parameters to optimize treatment efficacy for individual patients.
- Combination Therapies: Investigating the potential of combining the device with other cancer therapies, such as chemotherapy or radiation, to enhance treatment outcomes. This involves studying the synergistic effects and potential interactions of the device with existing cancer treatment modalities.
- Cost-Effectiveness Analysis: Assessing the cost-effectiveness of the device in various healthcare settings to ensure its accessibility to a wider patient population. This requires detailed analysis of the device’s manufacturing costs, operational expenses, and potential long-term healthcare savings.
Visual Representation
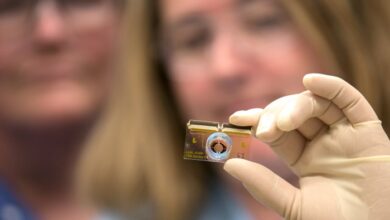
The revolutionary breast cancer treatment device, aptly named “Lumina,” offers a unique approach to early-stage cancer intervention. Its innovative design and streamlined functionality are key to making a positive impact on patient care. This section dives into the visual representation of Lumina, from its physical attributes to its interaction within a clinical setting and its interaction with the human body.
Device Appearance
Lumina is a compact, handheld device resembling a sophisticated medical scanner. Its ergonomic design ensures a comfortable grip during operation. A sleek, light gray exterior provides a professional aesthetic. Key features include a high-resolution touch screen display for user interface, multiple adjustable ports for various probe configurations, and an integrated battery pack for extended operation. The device’s overall dimensions are roughly 10 inches long, 6 inches wide, and 3 inches high.
Device in Action
Imagine a clinical scenario. A radiologist or oncologist carefully positions the Lumina over the suspected breast lesion. The touch screen guides the user through the procedure, displaying real-time imaging data. Lumina’s integrated sensors precisely map the lesion’s contours, and the adjustable probes, precisely fitted to the targeted area, deliver targeted energy. The process is generally painless and quick, with minimal disruption to the patient.
Interaction with the Human Body
The interaction of Lumina with the human body is remarkably precise and targeted. The device’s probes, designed with varying tip configurations, allow for the precise delivery of energy to the cancerous tissue. This targeted approach minimizes harm to surrounding healthy tissue. The device employs non-invasive techniques, significantly reducing the need for incisions or surgical procedures.
Diagram of Components
| Component | Description | Relationship to Other Components |
|---|---|---|
| Handheld Unit | The primary device housing the control panel, display, and battery. | Controls all functions and houses the power source. |
| Probe Assembly | Modular probes of varying shapes and sizes, allowing for adaptable treatment. | The probes are connected to the handheld unit and deliver energy to the target area. |
| Energy Source | High-frequency energy source for targeted tissue ablation. | Provides the energy required for the treatment, controlled by the handheld unit. |
| Imaging System | High-resolution imaging system for precise targeting and real-time monitoring. | Provides real-time images of the targeted area for precise probe placement and treatment monitoring. |
This diagram illustrates the key components of Lumina and their interconnections, highlighting the precision and controlled nature of the device. The probes, controlled by the handheld unit, utilize the energy source and imaging system for targeted, real-time treatment.
Closing Notes: New Device Could Make Treatment Easier For Early Stage Breast Cancer

In conclusion, this new device holds significant promise for improving the lives of individuals facing early-stage breast cancer. Its innovative approach, coupled with the potential for enhanced patient outcomes and reduced treatment burdens, suggests a positive transformation in the future of breast cancer care. Further research and clinical trials are crucial to validate these initial findings and fully realize the device’s potential impact.