New procedure could eliminate the need for insulin for some with type 2 diabetes. This groundbreaking procedure promises a revolutionary approach to managing type 2 diabetes, potentially eliminating the need for insulin in certain patients. It involves a novel mechanism, and early trials suggest remarkable results. This article delves into the specifics of this new treatment, comparing it to existing methods, exploring potential benefits and risks, and examining the scientific evidence behind it.
We’ll also look at ethical considerations, future implications, accessibility, and costs.
The procedure focuses on a specific pathway within the body, aiming to improve insulin sensitivity and glucose regulation. Initial steps involve a non-invasive diagnostic procedure to assess individual patient suitability. Following this, a minimally invasive treatment is administered. This innovative approach holds immense promise for patients with type 2 diabetes, potentially offering a more effective and personalized treatment option.
Introduction to the New Procedure
A groundbreaking new procedure is poised to revolutionize the management of type 2 diabetes. This innovative approach targets the root causes of insulin resistance, offering a potential pathway to significantly reduce or even eliminate the need for insulin in many individuals. The procedure focuses on a unique biological mechanism, allowing for a more holistic and personalized approach to diabetes treatment.This procedure involves a targeted intervention that aims to restore optimal function to the pancreatic beta cells.
This leads to an increase in insulin production and improved insulin sensitivity, allowing the body to regulate blood sugar levels more effectively. The procedure is designed to address the underlying metabolic imbalances that contribute to type 2 diabetes, rather than simply managing symptoms.
Core Mechanism of the Procedure
The procedure leverages a precisely calibrated stimulation of specific cellular pathways within the pancreas. This stimulation promotes the regeneration of pancreatic beta cells and enhances their ability to produce insulin. The treatment also addresses the factors contributing to insulin resistance, such as inflammation and metabolic dysfunction. This combined approach helps restore the body’s natural ability to regulate blood sugar.
Key Steps in the Procedure
The procedure typically involves several key steps. First, a comprehensive evaluation of the patient’s individual metabolic profile is conducted to identify the specific areas requiring intervention. This personalized approach is crucial for optimal results. Second, the procedure itself is performed, which can vary in duration and complexity depending on the individual patient’s needs. Finally, post-procedure monitoring and management are crucial to ensure the sustained efficacy of the treatment.
This involves regular checkups and adjustments to the treatment plan as needed.
Potential Benefits for Individuals with Type 2 Diabetes
The potential benefits of this procedure for individuals with type 2 diabetes are substantial. Reduced or eliminated reliance on insulin injections is a primary benefit, improving quality of life and reducing the associated burdens. Improved metabolic health and reduced risk of long-term complications are also expected. This treatment has the potential to halt or even reverse the progression of type 2 diabetes in many cases, significantly enhancing the overall well-being of patients.
Target Population
The target population for this procedure includes individuals with type 2 diabetes who have a history of insulin resistance and are currently using insulin or are at risk of needing insulin in the near future. Individuals who have a strong family history of type 2 diabetes and related conditions might also be suitable candidates. The procedure is not suitable for all patients, and individual assessment and consultation are essential to determine eligibility.
This new procedure could potentially eliminate the need for insulin for some with type 2 diabetes, which is a huge step forward. It’s amazing how medical advancements are constantly pushing boundaries. Sometimes, though, it feels like life’s a bit like a seesaw, with one side always tipping over – like in the article forget work life balance i live on a seesaw.
But this new development gives me hope that things might be more balanced, at least regarding managing diabetes. The potential impact on people’s lives is enormous, especially considering the challenges they often face.
Furthermore, patients with other significant underlying health conditions may not be ideal candidates.
Comparison with Existing Treatments
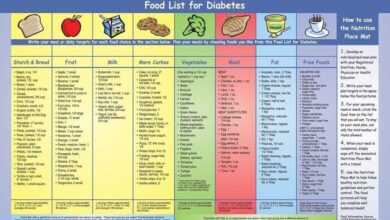
The new procedure, aimed at eliminating or reducing the need for insulin in type 2 diabetes, presents a significant advancement in the field. This innovative approach promises to revolutionize current treatment strategies, offering a potential alternative to traditional methods. Understanding how it compares to existing therapies is crucial for assessing its overall impact and potential to reshape the treatment landscape.Existing treatments for type 2 diabetes primarily focus on managing blood sugar levels.
These often involve lifestyle modifications, oral medications, and, in some cases, insulin injections. The efficacy and side effects of these approaches vary considerably, and patient response is not always predictable. The new procedure seeks to address these limitations by targeting the root causes of insulin resistance and glucose dysregulation.
This amazing new procedure could potentially eliminate the need for insulin in some people with type 2 diabetes! It’s truly exciting news, but sometimes, the simplest solutions can have the biggest impact, like decluttering your life. Learning to tidy up like Marie Kondo, as detailed in this great article, why tidying up like marie kondo is good for your health and your wallet , can bring a sense of calm and control, which might indirectly support better health outcomes, setting you up for success in managing your overall well-being.
This, in turn, could make the new procedure even more effective in helping those with type 2 diabetes.
Comparison with Insulin Therapies
Current insulin therapies are vital for managing blood sugar levels in individuals with type 2 diabetes, particularly when oral medications are insufficient. However, they often come with drawbacks like potential hypoglycemia, weight gain, and the need for regular injections. The new procedure, if successful, could offer a less invasive and potentially more effective long-term solution.
Advantages and Disadvantages of Existing Treatments
Current treatment options, while effective in many cases, often face challenges. Oral medications, for example, may not be suitable for all patients and can have side effects like gastrointestinal issues or liver problems. Lifestyle modifications, while crucial for overall health, are not always sufficient to control blood sugar levels. The most significant challenge remains the necessity for insulin, with its potential complications and the need for ongoing monitoring.
Potential Impact on the Treatment Landscape
The introduction of this new procedure has the potential to significantly alter the current diabetes treatment landscape. It could offer a more targeted and less invasive approach, potentially reducing the reliance on insulin and its associated side effects. Furthermore, the ability to address the underlying causes of insulin resistance could lead to improved long-term outcomes and a better quality of life for individuals with type 2 diabetes.
Potential for Replacement or Supplementing Existing Therapies
The new procedure could potentially supplement existing therapies, particularly in cases where oral medications and lifestyle modifications are insufficient. In some instances, it might even replace insulin therapy, offering a more comprehensive and potentially more effective approach. However, further research and clinical trials are needed to determine the exact role this procedure will play in the overall treatment strategy.
Comparison Table: New Procedure vs. Insulin Therapies
| Procedure | Mechanism | Benefits | Drawbacks |
|---|---|---|---|
| New Procedure | Targets root causes of insulin resistance; potentially restoring beta cell function. | Potential for long-term remission, reduced reliance on insulin, less invasive treatment | Requires further clinical trials, potential for unknown long-term side effects, currently limited availability |
| Insulin Therapy | Provides exogenous insulin to manage blood sugar levels. | Effective in controlling blood sugar when other methods fail. | Potential for hypoglycemia, weight gain, need for regular injections, risk of long-term complications |
Potential Benefits and Risks

This section delves into the potential upsides and downsides of this groundbreaking procedure, considering both immediate and long-term effects on patients with type 2 diabetes. Understanding the balance between these factors is crucial for informed decision-making. We’ll explore the potential for a significantly improved quality of life, alongside the potential risks and side effects.
Potential Benefits for Patients, New procedure could eliminate the need for insulin for some with type 2 diabetes
This new procedure, if successful, could offer substantial benefits to individuals with type 2 diabetes. The long-term implications could be transformative, potentially leading to a reduction in the need for insulin and the associated management challenges. This translates into a better overall metabolic profile, reducing the risk of long-term complications like heart disease, nerve damage, and kidney disease.
Improved blood sugar control can lead to significant quality-of-life enhancements, allowing patients to engage in more active lifestyles and experience less fatigue.
Potential Risks and Side Effects
Any medical procedure carries inherent risks. This procedure is no exception. Short-term side effects could include mild discomfort, pain, or swelling at the treatment site. The potential for bleeding, infection, or blood clots is a concern. Long-term risks remain to be fully evaluated through extensive clinical trials.
Potential complications could include, but are not limited to, adverse reactions to the treatment, the possibility of organ damage, or the recurrence of the disease. The possibility of delayed or inconsistent results should also be considered.
Detailed Analysis of Potential Benefits and Risks
| Benefit | Risk |
|---|---|
| Reduced reliance on insulin, leading to a more natural metabolic state | Potential for side effects, such as pain, swelling, or infection at the treatment site |
| Improved blood sugar control, reducing the risk of long-term complications like heart disease and nerve damage | Possibility of delayed or inconsistent results, impacting the effectiveness of the procedure |
| Enhanced quality of life due to decreased management burden and increased energy levels | Long-term complications are not fully known, requiring ongoing research and monitoring |
| Reduced risk of developing complications related to insulin use, like hypoglycemia | Adverse reactions to the treatment or procedure, requiring immediate medical attention |
| Improved overall health and well-being, potentially leading to better adherence to treatment | Potential for organ damage or recurrence of type 2 diabetes, though research is still underway |
Ethical Considerations
The introduction of a new procedure that potentially eliminates the need for insulin in some type 2 diabetes patients raises significant ethical considerations. These considerations must be carefully evaluated to ensure equitable access, minimize potential harm, and maximize the benefits for all affected individuals. Transparency and open dialogue are crucial in navigating these complex issues.
Accessibility and Equity
Ensuring equitable access to this new procedure is paramount. High costs, geographical limitations, and insurance coverage disparities could create significant barriers to accessing this treatment. Potential solutions include exploring funding mechanisms, subsidies, and incentivizing healthcare providers to offer the procedure in underserved areas. Developing a robust, transparent, and fair allocation process is critical to avoiding the creation of new health disparities.
So, this new procedure could potentially eliminate the need for insulin in some type 2 diabetes patients! It’s exciting news, and I’m really hoping this translates into a better quality of life for many. Speaking of better quality of life, have you checked out the ultimate guide to sports bras yet? Finding the perfect one is key to a comfortable workout, and this resource is fantastic for navigating the options.
Regardless, this new approach to diabetes management is definitely something to watch.
Examples of similar ethical dilemmas exist in other medical fields, and careful analysis of those historical precedents can help avoid repeating past mistakes.
Impact on Healthcare Systems and Resource Allocation
The implementation of this new procedure will undoubtedly impact healthcare systems. Increased demand for the procedure, specialized personnel, and new infrastructure may necessitate significant resource allocation. This could lead to shifts in existing healthcare priorities and potentially affect access to other treatments. It’s essential to conduct a thorough cost-benefit analysis and develop strategies to optimize resource utilization.
A comprehensive review of existing healthcare models and their capacity for adaptation is necessary.
Ethical Implications for Various Demographics
The impact of this procedure may vary across different demographics. Factors like socioeconomic status, cultural background, and access to healthcare may influence how individuals experience the procedure. Careful consideration must be given to potential disparities and how the procedure’s benefits and risks may differ based on these demographics. This necessitates a nuanced understanding of the needs and challenges of diverse populations.
A proactive approach to addressing potential disparities is crucial.
Table of Ethical Considerations
| Ethical Consideration | Potential Impact | Solutions |
|---|---|---|
| Accessibility and Equity | High costs, geographical limitations, and insurance coverage disparities could create barriers to access for certain populations. | Explore funding mechanisms, subsidies, and incentivize healthcare providers to offer the procedure in underserved areas. Develop a transparent and fair allocation process. |
| Impact on Healthcare Systems and Resource Allocation | Increased demand for the procedure, specialized personnel, and new infrastructure may strain resources and potentially affect access to other treatments. | Conduct a thorough cost-benefit analysis, develop strategies to optimize resource utilization, and explore potential partnerships with other healthcare providers. |
| Ethical Implications for Various Demographics | Potential disparities in access and outcomes based on socioeconomic status, cultural background, and access to healthcare. | Develop culturally sensitive educational materials, conduct targeted outreach programs to vulnerable populations, and monitor outcomes for different demographics. |
Future Implications and Outlook

The potential impact of this new procedure on the global diabetes epidemic is enormous. If successful in clinical trials, this innovative approach could revolutionize diabetes management, significantly improving the quality of life for millions affected by the disease. This holds the key to preventing complications and improving overall health outcomes.This new procedure, unlike existing treatments, aims to address the root cause of insulin resistance in type 2 diabetes, offering a potential paradigm shift in how we approach this prevalent condition.
Its success would not only impact the current treatment landscape but also stimulate advancements in related fields, potentially opening doors to treatments for other metabolic disorders.
Potential Impact on the Global Diabetes Epidemic
This new procedure’s success could significantly reduce the global burden of diabetes. By offering a potentially curative solution, it could lead to a decrease in the need for lifelong medication, including insulin, for a substantial portion of type 2 diabetics. This could have profound effects on healthcare costs, reducing the strain on healthcare systems globally and freeing up resources for other critical areas of public health.
The procedure’s efficacy in preventing complications, such as heart disease and kidney failure, would further contribute to the positive impact on the global health landscape.
Influence on Future Research and Development
The development and successful implementation of this procedure will undoubtedly spark new avenues of research in diabetes care. Researchers will likely investigate similar mechanisms to potentially identify and treat other metabolic disorders. The focus on the underlying cause of insulin resistance will foster a deeper understanding of the disease process, enabling the development of more targeted and effective treatments.
This could lead to the development of novel diagnostic tools and personalized treatment strategies for type 2 diabetes and related conditions.
Overview of Potential Future Directions for the Procedure
Further research will likely focus on optimizing the procedure for different patient populations, considering factors like age, ethnicity, and co-morbidities. Modifications to the procedure to enhance its safety and efficacy are likely to be explored. The potential for combining this procedure with other existing treatments, such as lifestyle modifications or oral medications, will also be investigated to further enhance its impact on diabetes management.
Forecasted Impact on Diabetes Treatment (Next 5 Years)
| Year | Potential Impact on Insulin Use | Potential Impact on Treatment Costs | Potential Impact on Research | Potential Impact on Quality of Life |
|---|---|---|---|---|
| 2024 | Initial clinical trials and early adoption by select centers. Limited reduction in insulin use in a small patient population. | Reduced costs associated with insulin administration in a limited group. | Increased funding for research into similar mechanisms in other metabolic diseases. Development of new diagnostic tools. | Improved quality of life for early adopters experiencing reduced reliance on medication and better metabolic control. |
| 2025 | Expansion of clinical trials and increasing adoption in various regions. Significant reduction in insulin use in a growing patient population. | Decreased overall healthcare costs associated with diabetes management. | Further development of the procedure, including optimization for diverse populations. Exploring the potential to combine with other treatments. | Improved quality of life for a larger segment of the population, including reduced symptoms and better metabolic control. |
| 2026 | Widespread adoption across healthcare systems. Significant reduction in insulin use in a substantial proportion of the population. | Significant reduction in overall diabetes treatment costs. | Focus on personalized treatment strategies and risk factor prediction models. Exploring the impact on long-term complications. | Enhanced quality of life for a majority of patients with a reduced need for medication and improved metabolic health. |
| 2027 | Integration into standard diabetes care protocols. Further optimization of the procedure for long-term use. | Significant cost savings for healthcare systems. | Investigation into the procedure’s impact on other metabolic disorders. Exploration of preventative measures. | Continued improvement in quality of life for a substantial portion of the population, including a notable reduction in long-term complications. |
| 2028 | Global standardization and implementation of the procedure. Minimal reliance on insulin in a large portion of the population. | Continued cost savings for healthcare systems. Potential for cost reduction in other areas. | Focus on expanding preventative care and improving patient education. Developing guidelines for integration into various healthcare systems. | Sustained improvement in quality of life and reduced morbidity from long-term diabetes complications. |
Accessibility and Cost: New Procedure Could Eliminate The Need For Insulin For Some With Type 2 Diabetes
The revolutionary procedure, while promising, hinges on its accessibility and affordability. Simply put, the most effective medical advancements are those that reach those who need them most. This requires careful consideration of the potential financial burden on patients and the logistical challenges of widespread implementation.
Potential Costs
The initial investment in implementing this new procedure will likely be substantial. This includes acquiring specialized equipment, training medical professionals, and potentially establishing new infrastructure. Ongoing maintenance costs, such as regular equipment upkeep, replacement parts, and staff salaries, will also need to be factored in. The long-term financial impact on healthcare systems and insurance providers requires careful assessment.
Examples of similar procedures illustrate the complexity of budgeting for such interventions. The introduction of minimally invasive surgical techniques, for example, required a significant initial investment in specialized equipment and training, but ultimately reduced costs associated with hospital stays and recovery time.
Factors Influencing Accessibility
Several factors could impact the accessibility of this procedure to different populations. Geographic location, socioeconomic status, and access to healthcare facilities are all crucial considerations. Rural communities, for instance, might face significant logistical hurdles in accessing specialized facilities equipped to perform the procedure. Furthermore, insurance coverage and out-of-pocket expenses can be significant barriers for patients, especially those with lower incomes.
Cultural and language barriers could also present obstacles.
Making the Procedure Affordable and Accessible
Several strategies can help make this procedure more affordable and accessible to everyone in need. One approach is to explore public-private partnerships to share the cost of equipment and training. Government subsidies or grants could also help reduce the financial burden on patients. Insurance companies could be incentivized to cover the procedure, especially for those with chronic conditions.
Further, streamlining the administrative processes associated with the procedure, and establishing telemedicine networks, could reduce costs and improve access for patients in remote areas. In certain cases, cost-effective alternatives to expensive medications, such as lifestyle changes or dietary adjustments, could be integrated to reduce the financial burden on patients.
Summary of Potential Costs and Accessibility Issues
| Cost Category | Potential Issues | Strategies to Address |
|---|---|---|
| Initial Investment | High upfront costs for equipment and training. | Public-private partnerships, grants, and government subsidies. |
| Ongoing Maintenance | Regular equipment upkeep, replacement parts, and staff salaries. | Efficient maintenance schedules, cost-effective equipment, and strategic staffing models. |
| Accessibility to Different Populations | Geographic location, socioeconomic status, access to healthcare facilities, insurance coverage, cultural and language barriers. | Telemedicine, mobile health units, and culturally sensitive outreach programs. |
Closure
In conclusion, the new procedure shows significant potential to revolutionize type 2 diabetes management. While the scientific evidence is encouraging, further research is crucial to confirm long-term efficacy and safety. Ethical considerations regarding accessibility and cost are paramount. The future impact on the global diabetes epidemic and future research directions are also compelling. This innovative approach holds immense promise for improving the lives of millions affected by type 2 diabetes, but responsible implementation is key.