New research diabetes distress unveils the complexities of emotional burdens faced by those living with diabetes. This exploration delves into the various facets of diabetes distress, from its defining characteristics to the profound impact it has on overall well-being and treatment adherence. We’ll examine emerging research trends, analyze the effectiveness of interventions, and discuss the future of research in this critical area.
The research highlights the importance of understanding and addressing this significant issue within the healthcare system.
The research explores the intricate relationship between diabetes distress and a range of factors, including the types of diabetes, individual experiences, and available support systems. The study also emphasizes the importance of tailored interventions to effectively manage diabetes distress and improve the quality of life for individuals with diabetes. Furthermore, the study examines the crucial role of healthcare professionals in identifying and addressing diabetes distress in a proactive manner.
Defining Diabetes Distress
Diabetes distress is a significant emotional burden experienced by many individuals living with diabetes. It’s more than just the frustration of managing a chronic condition; it’s a complex interplay of emotions, anxieties, and psychological challenges that can significantly impact daily life. Understanding the nuances of diabetes distress is crucial for providing effective support and care to those affected.Diabetes distress encompasses a wide range of negative emotional responses related to the management and living with diabetes.
This can manifest in various ways, from feelings of anger and frustration to anxiety and depression. It’s a critical aspect of diabetes care that often goes unrecognized or unaddressed, leading to poorer health outcomes and reduced quality of life.
New research is shedding light on diabetes distress, a significant emotional burden for many living with the condition. While the exact causes are complex, understanding the interplay of factors is key. Interestingly, some studies explore links to hereditary conditions, like whether pituitary tumors are inherited are pituitary tumors hereditary , which can further complicate the picture.
Ultimately, this new research is crucial for developing more effective support systems and treatments for diabetes distress.
Understanding the Facets of Diabetes Distress
Diabetes distress is not a single entity; it presents itself in diverse forms. These variations can be categorized into different types, each with its own set of associated symptoms and contributing factors. Recognizing these facets is vital for tailored interventions and support.
Types of Diabetes Distress
Several types of diabetes distress exist, each with unique characteristics.
- Emotional Distress: This encompasses a broad range of negative emotions like fear, anger, guilt, and sadness related to the diagnosis, treatment, and daily management of diabetes. These feelings can be triggered by various factors, including treatment side effects, challenges in maintaining blood sugar levels, or the social stigma associated with the condition.
- Behavioral Distress: This manifests as problematic coping mechanisms and behaviors related to diabetes management. These may include poor adherence to treatment plans, unhealthy eating habits, and avoidance of self-monitoring or seeking medical help. This can be linked to feelings of powerlessness or overwhelm in managing the condition.
- Cognitive Distress: This involves negative thought patterns, distorted beliefs, and difficulties in problem-solving related to diabetes. Individuals might experience feelings of hopelessness, helplessness, or inadequacy regarding their ability to manage their condition effectively.
Symptoms of Diabetes Distress
Diabetes distress presents a wide array of symptoms, impacting both physical and mental well-being. Identifying these symptoms is essential for early intervention and support.
- Emotional Symptoms: These include feelings of anxiety, fear, anger, frustration, depression, and hopelessness. Individuals may experience heightened emotional reactivity to daily stressors or challenges associated with diabetes.
- Behavioral Symptoms: These may include poor adherence to treatment plans, changes in eating habits, increased alcohol or substance use, social isolation, or avoidance of situations related to diabetes management.
- Cognitive Symptoms: These manifest as negative thoughts, difficulty concentrating, poor problem-solving skills, and feelings of inadequacy or helplessness in managing the condition. Individuals might experience distorted perceptions of their abilities or circumstances related to diabetes.
Comparing Diabetes Distress with Other Emotional Burdens
Distinguishing diabetes distress from other emotional burdens is crucial for appropriate support. While feelings of stress, anxiety, and depression are common, diabetes distress is specifically related to the experience of living with diabetes.
- General Stress: General stress can stem from various life events and is not necessarily diabetes-specific. Diabetes distress, however, is directly linked to the challenges of diabetes management.
- Depression: Depression involves persistent sadness and loss of interest in activities. While depression can coexist with diabetes distress, the latter is specifically rooted in the diabetes-related experiences.
- Anxiety: Anxiety encompasses feelings of worry and apprehension. While anxiety can be triggered by diabetes-related concerns, diabetes distress is a more focused and persistent reaction to the specific demands of living with diabetes.
Factors Contributing to Diabetes Distress
Several factors can contribute to the development of diabetes distress. Understanding these factors is essential for developing preventative and supportive strategies.
- Lack of social support: Limited support networks can exacerbate feelings of isolation and vulnerability, potentially leading to diabetes distress.
- Poor diabetes self-management education: Insufficient knowledge and skills in diabetes management can lead to feelings of inadequacy and overwhelm.
- Treatment-related side effects: Adverse reactions to medications or treatment plans can contribute to feelings of distress and frustration.
- Perceived barriers to care: Challenges accessing healthcare services or experiencing difficulties with communication can contribute to the development of diabetes distress.
Key Elements of Diabetes Distress
| Element | Description |
|---|---|
| Emotional distress | Negative emotions related to diabetes diagnosis, treatment, and management. |
| Behavioral distress | Problematic coping mechanisms and behaviors impacting diabetes management. |
| Cognitive distress | Negative thought patterns, distorted beliefs, and difficulties in problem-solving. |
| Social factors | Lack of social support, limited access to resources, and social stigma. |
| Treatment-related factors | Side effects of medications, complexity of treatment plans, and barriers to care. |
Impact on Well-being
Diabetes distress significantly impacts the overall well-being of individuals living with diabetes. It’s not just about the physical challenges; the emotional and psychological toll can be substantial. This distress can profoundly affect their ability to manage their condition effectively, leading to poorer health outcomes and reduced quality of life. Understanding the multifaceted nature of this distress is crucial for developing effective support strategies and interventions.Diabetes distress creates a vicious cycle.
The burden of managing a chronic condition, coupled with the fear of complications and the emotional strain, can lead to decreased adherence to treatment plans and lifestyle changes. This, in turn, exacerbates the condition and further fuels the distress, highlighting the interconnectedness of physical and mental health in diabetes management.
Negative Impacts on Overall Well-being
Diabetes distress negatively affects various aspects of daily life, including physical, emotional, and social well-being. The constant worry, frustration, and fear associated with diabetes can lead to a decline in overall quality of life. This can manifest as fatigue, sleep disturbances, and decreased participation in social activities.
New research on diabetes distress is fascinating, highlighting the emotional toll of the condition. One key area being explored is how different types of dietary fiber impact overall well-being, and, importantly, how to manage the stress related to diabetes. For example, understanding that not all dietary fibers are equal, as detailed in this helpful article ( not all dietary fibers are equal heres why ), is crucial for tailoring a healthy eating plan.
Ultimately, this knowledge can contribute significantly to improving diabetes management and reducing distress.
Impact on Treatment Adherence
Diabetes distress directly correlates with poor adherence to treatment plans. Individuals experiencing high levels of distress may struggle to consistently take medications, monitor blood sugar levels, or follow recommended dietary guidelines. This lack of adherence can lead to uncontrolled blood sugar levels, increasing the risk of developing diabetes-related complications. For example, a person struggling with the emotional weight of managing their diabetes might skip insulin injections, or neglect regular exercise, ultimately leading to poor control of their blood sugar.
Correlation with Diabetes Complications
The relationship between diabetes distress and complications is well-documented. Chronic stress and elevated cortisol levels, frequently associated with diabetes distress, can negatively impact blood vessel function, increasing the risk of cardiovascular disease, neuropathy, and nephropathy. This is further evidenced by studies showing a strong correlation between distress levels and the occurrence of complications like diabetic retinopathy.
Psychological Consequences
Diabetes distress can have profound psychological consequences, potentially leading to anxiety and depression. The chronic nature of the condition, coupled with the responsibility of managing it, can contribute to feelings of helplessness, hopelessness, and isolation. For instance, the fear of developing complications, the social stigma associated with diabetes, and the emotional burden of daily management can significantly impact mental health.
Table: Multifaceted Effects of Diabetes Distress
| Aspect of Daily Life | Impact of Diabetes Distress |
|---|---|
| Physical Health | Increased risk of complications, fatigue, sleep disturbances |
| Emotional Well-being | Anxiety, depression, irritability, feelings of hopelessness |
| Social Life | Reduced participation in social activities, social isolation, difficulty maintaining relationships |
| Mental Health | Decreased quality of life, decreased self-esteem, cognitive impairment |
| Adherence to Treatment | Decreased adherence to medication schedules, dietary plans, and exercise regimens |
Research Trends and Studies: New Research Diabetes Distress
The research landscape surrounding diabetes distress is constantly evolving, driven by a growing recognition of its significant impact on patients’ lives. Researchers are exploring various aspects of the condition, from identifying risk factors and effective interventions to understanding the diverse experiences of individuals living with diabetes. This exploration promises to lead to improved support systems and ultimately better outcomes for those affected.Recent studies are revealing key insights into the multifaceted nature of diabetes distress, moving beyond simple definitions to encompass the complex interplay of psychological, social, and physiological factors.
Researchers are increasingly utilizing sophisticated methodologies to delve deeper into the experiences and needs of individuals with diabetes.
Emerging Trends in Research
Researchers are increasingly adopting mixed-methods approaches, combining quantitative and qualitative data collection techniques. This allows for a more comprehensive understanding of the experiences and perceptions associated with diabetes distress, offering richer insights than either method alone. Furthermore, there’s a noticeable shift towards longitudinal studies, tracking individuals over time to examine the trajectory of diabetes distress and its potential long-term consequences.
This approach is crucial for identifying factors that predict or mitigate the development of distress.
Key Findings from Recent Studies
A growing body of evidence highlights the significant correlation between diabetes distress and poor glycemic control. Studies have shown that individuals experiencing high levels of diabetes distress often struggle to maintain healthy blood sugar levels, impacting their overall health and well-being. Furthermore, these studies frequently reveal a link between diabetes distress and psychological comorbidities, such as anxiety and depression.
The cumulative effect of these factors can exacerbate the challenges faced by individuals living with diabetes.
Methodologies Used in Research Studies
The methodologies employed in studies on diabetes distress vary, reflecting the complexity of the topic. Quantitative studies often utilize standardized questionnaires to measure levels of distress, while qualitative research employs interviews and focus groups to gain deeper insights into the lived experiences of individuals. The strengths of these methods lie in their ability to quantify distress levels and uncover the nuanced perspectives of those affected, respectively.
Limitations, however, often include potential biases in self-reporting, or difficulties in generalizing findings from smaller samples.
Diverse Populations Studied
Studies have examined various populations, including individuals with type 1 and type 2 diabetes, spanning different ages, ethnicities, and socioeconomic backgrounds. Findings indicate disparities in diabetes distress levels across these groups. For instance, individuals from marginalized communities may face additional stressors that contribute to higher levels of distress. Recognizing and addressing these disparities is critical to developing targeted interventions.
Interventions Explored in Studies
Researchers are investigating various interventions to mitigate diabetes distress. These interventions include psychoeducational programs, mindfulness-based stress reduction techniques, and social support groups. Some studies have also explored the efficacy of telehealth interventions in providing accessible and convenient support. The success of these interventions varies depending on the specific population and the design of the study, indicating the need for tailored approaches.
For example, a program focusing on diabetes self-management education might show promising results in reducing distress among certain groups, while another program focusing on social support might be more effective for others.
Interventions and Support

Navigating the complexities of diabetes can be emotionally challenging, leading to distress. Understanding and addressing this distress is crucial for improving overall well-being and diabetes management. Effective interventions and supportive strategies are vital in helping individuals cope with the emotional and practical aspects of living with diabetes.Interventions for diabetes distress are not a one-size-fits-all approach. They should be tailored to the individual’s specific needs, preferences, and cultural context.
This requires a holistic approach that considers the interplay of psychological, social, and medical factors. The goal is not only to reduce distress but also to enhance coping mechanisms and resilience, ultimately empowering individuals to effectively manage their diabetes.
Interventions to Mitigate Diabetes Distress
Tailored interventions are essential for addressing the diverse needs of individuals experiencing diabetes distress. These interventions can encompass a wide range of strategies, from individual therapy to support groups. Effective interventions often combine multiple approaches to create a comprehensive support system.
| Intervention Type | Description | Examples |
|---|---|---|
| Individual Therapy | Provides a safe space for individuals to explore their feelings and develop coping strategies. Therapy can address anxiety, depression, and other mental health concerns that often accompany diabetes distress. | Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), Mindfulness-based stress reduction (MBSR) |
| Support Groups | Offer a sense of community and shared experience. Participants can learn from others’ experiences, provide mutual support, and share coping strategies. | Diabetes support groups, online forums, and local chapters of diabetes organizations |
| Educational Programs | Empower individuals with knowledge and skills to better manage their diabetes. Comprehensive education can address the physical and emotional aspects of living with diabetes. | Workshops on diabetes self-management, nutrition, and stress management. |
| Mindfulness and Relaxation Techniques | Promote stress reduction and emotional regulation. Practices like meditation and deep breathing can help manage anxiety and improve overall well-being. | Guided meditation apps, yoga classes, progressive muscle relaxation. |
| Assertive Communication Training | Equip individuals with the skills to effectively communicate their needs and concerns to healthcare providers and family members. | Role-playing exercises, communication workshops. |
Coping Mechanisms and Resilience Enhancement
Developing effective coping mechanisms is crucial for managing diabetes distress. These mechanisms can help individuals navigate challenges, build resilience, and maintain a positive outlook.
- Problem-solving skills training: Identifying and addressing the specific issues contributing to diabetes distress. This involves breaking down problems into smaller, manageable steps and exploring various solutions.
- Social support network building: Cultivating strong relationships with family, friends, and support groups. These connections provide emotional encouragement and practical assistance.
- Positive self-talk and affirmations: Replacing negative thoughts with positive and encouraging self-statements. This promotes a more optimistic and resilient mindset.
- Time management techniques: Prioritizing tasks, setting realistic goals, and allocating time effectively. This helps individuals feel more in control and reduces stress associated with diabetes management.
Support Systems for Individuals with Diabetes Distress
Strong support systems are vital for navigating the challenges of diabetes. These systems can provide emotional, practical, and informational support, helping individuals feel empowered and connected.
- Family and friends: Providing emotional support, practical assistance, and understanding are key components of a supportive network. Encouraging open communication and shared responsibility is important.
- Healthcare professionals: Diabetes educators, endocrinologists, and mental health professionals can provide guidance, support, and resources. Open communication and collaboration are essential for effective management.
- Support groups and online communities: These platforms offer a sense of community and shared experience. Individuals can connect with others facing similar challenges and learn from their experiences.
Role of Healthcare Professionals in Addressing Diabetes Distress
Healthcare professionals play a critical role in recognizing and addressing diabetes distress. Their expertise is vital in creating a supportive environment and providing appropriate interventions.
- Screening for diabetes distress: Regularly assessing patients for emotional and psychological distress. This can be achieved through standardized questionnaires or direct conversations.
- Providing referrals to mental health professionals: Connecting patients with mental health specialists when needed. Early intervention is crucial for managing and preventing more severe mental health concerns.
- Educating patients about diabetes distress: Increasing awareness and understanding of the emotional challenges associated with diabetes can help patients feel supported and empowered to seek help.
- Creating a supportive and empathetic care environment: Prioritizing open communication and addressing patient concerns with empathy and understanding.
Resources and Support Groups, New research diabetes distress
Numerous resources and support groups are available to help individuals manage diabetes distress. These resources can provide valuable information, support, and coping strategies.
- Diabetes organizations: National organizations and local chapters often offer support groups, educational programs, and resources for individuals with diabetes.
- Online forums and support groups: Many online platforms provide a space for individuals to connect with others, share experiences, and receive support.
- Mental health professionals: Psychologists, psychiatrists, and other mental health specialists can provide individual therapy and support for diabetes distress.
Future Directions for Research
Unraveling the complexities of diabetes distress requires a proactive and forward-thinking approach to research. Current research has laid a strong foundation, but there are still critical gaps in our understanding that need to be addressed to improve the lives of those affected. This exploration into future directions will highlight key areas for investigation, emphasizing the importance of culturally sensitive approaches, longitudinal studies, technological integration, and a comprehensive approach to research gaps.Further research on diabetes distress should focus on identifying nuanced factors that contribute to its development and severity.
New research is highlighting the significant emotional toll of diabetes distress. It’s a complex issue, and while there’s no magic bullet, exploring natural remedies like the top benefits of prunes prune juice 2 could potentially offer some support. This research suggests that incorporating dietary changes, like those found in top benefits of prunes prune juice 2 , might help manage some of the associated stress.
Ultimately, further research into these connections between diet and diabetes distress is needed.
For instance, the interplay between psychosocial stressors, diabetes management challenges, and individual coping mechanisms warrants deeper investigation. This will help tailor interventions more effectively to specific needs and circumstances.
Potential Areas for Future Research
Addressing the multifaceted nature of diabetes distress requires a comprehensive approach. This involves delving into the specific impact of various factors on individuals, and developing targeted interventions. Research should explore how different demographic characteristics, cultural backgrounds, and socioeconomic factors influence the experience of diabetes distress.
- Exploring the impact of specific diabetes-related challenges, such as fluctuating blood glucose levels, hypoglycemia, or treatment regimen complexity, on the development of distress.
- Investigating the role of social support networks and the influence of family dynamics on diabetes distress.
- Examining the relationship between diabetes distress and mental health conditions, including anxiety and depression.
- Assessing the effectiveness of different coping mechanisms in mitigating diabetes distress and promoting well-being.
Culturally Sensitive Approaches
Recognizing the diverse experiences of individuals with diabetes is crucial. Research must acknowledge the influence of cultural beliefs, values, and practices on diabetes management and the manifestation of distress.
- Incorporating diverse perspectives and cultural sensitivities into study design, recruitment, and data analysis is paramount.
- Developing culturally adapted interventions and support resources is essential for promoting engagement and effectiveness.
- Conducting studies in diverse communities to gain a deeper understanding of the unique challenges faced by different cultural groups.
- Collaborating with community leaders and cultural experts to ensure the cultural appropriateness and relevance of research findings.
Importance of Longitudinal Studies
Understanding the trajectory of diabetes distress over time is crucial for developing effective long-term strategies. Longitudinal studies allow researchers to track the development, progression, and potential predictors of distress over extended periods.
- Tracking individuals with diabetes over time to observe how distress evolves and how it impacts adherence to treatment plans.
- Identifying early warning signs and indicators of increasing distress to facilitate early intervention.
- Evaluating the effectiveness of interventions in maintaining improved well-being over time.
Role of Technology in Supporting Individuals
Technological advancements offer new avenues for supporting individuals with diabetes distress. Mobile health applications, telehealth platforms, and online support groups can provide convenient and accessible resources.
- Developing mobile applications that provide personalized support, education, and coping strategies.
- Utilizing telehealth platforms for remote monitoring and management of diabetes distress, fostering improved communication with healthcare providers.
- Creating online support groups to connect individuals with shared experiences, fostering a sense of community and shared coping strategies.
Research Gaps and Priorities
This table summarizes key areas where research is needed to address diabetes distress:
| Research Gap | Priority |
|---|---|
| Lack of culturally sensitive interventions | Developing culturally adapted interventions and support resources. |
| Limited understanding of the longitudinal trajectory of distress | Conducting longitudinal studies to track the development and progression of distress. |
| Insufficient utilization of technology for support | Developing and implementing mobile health applications and telehealth platforms. |
| Inadequate understanding of the interplay between diabetes management challenges and psychosocial factors | Investigating the interplay between psychosocial stressors, diabetes management challenges, and individual coping mechanisms. |
Practical Implications for Healthcare
Diabetes distress significantly impacts patients’ ability to manage their condition effectively. Understanding this distress and its effects is crucial for healthcare providers to offer comprehensive care. Recognizing the emotional and psychological burden associated with diabetes is vital for improving patient outcomes and overall well-being.
Applying Findings in Healthcare Settings
Healthcare professionals can use research findings on diabetes distress to tailor interventions that address the emotional and psychological aspects of diabetes management. This proactive approach can lead to better patient adherence to treatment plans, improved blood glucose control, and ultimately, reduced long-term complications. A crucial step is recognizing the importance of a patient-centered approach, where individual needs and preferences are considered when designing interventions.
Importance of Screening for Diabetes Distress
Routine screening for diabetes distress is essential in clinical practice. Early identification of distress allows for timely intervention and support, preventing the escalation of negative emotions and behaviors. This early detection is crucial for preventing emotional issues from interfering with treatment adherence and blood glucose control. For instance, a patient experiencing high levels of diabetes distress may struggle to adhere to medication regimens or dietary recommendations.
Integrating Support Services for Diabetes Distress
Integrating support services for diabetes distress into clinical practice is paramount. This can involve offering access to mental health professionals, support groups, or online resources tailored to diabetes distress. These services can provide a safe space for patients to discuss their concerns, receive emotional support, and develop coping mechanisms. For example, a diabetes support group could provide a forum for sharing experiences, offering encouragement, and learning from others facing similar challenges.
Role of Patient Education in Managing Diabetes Distress
Patient education plays a vital role in managing diabetes distress. Education should not only focus on the technical aspects of diabetes management but also on stress management techniques, coping mechanisms, and emotional well-being. This holistic approach empowers patients to actively participate in their care and develop strategies to effectively manage the emotional burden of diabetes. For example, teaching relaxation techniques, mindfulness exercises, or stress reduction strategies can significantly aid in mitigating diabetes distress.
Practical Steps for Healthcare Providers
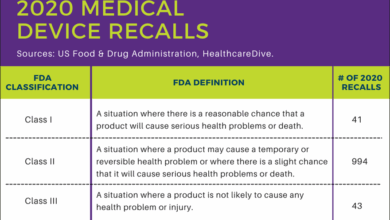
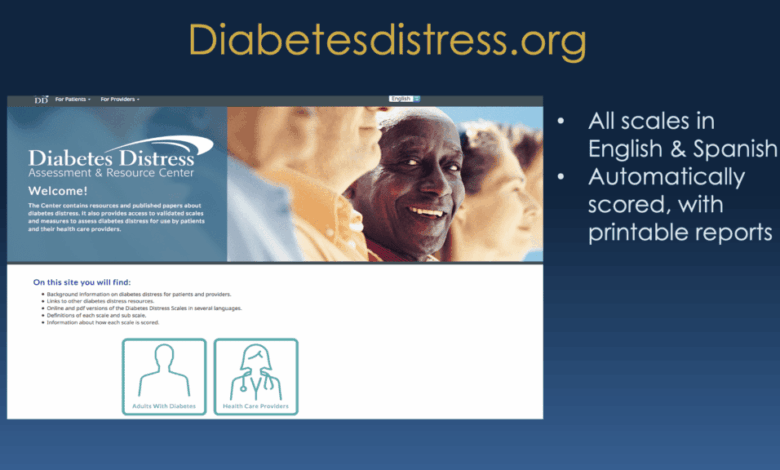
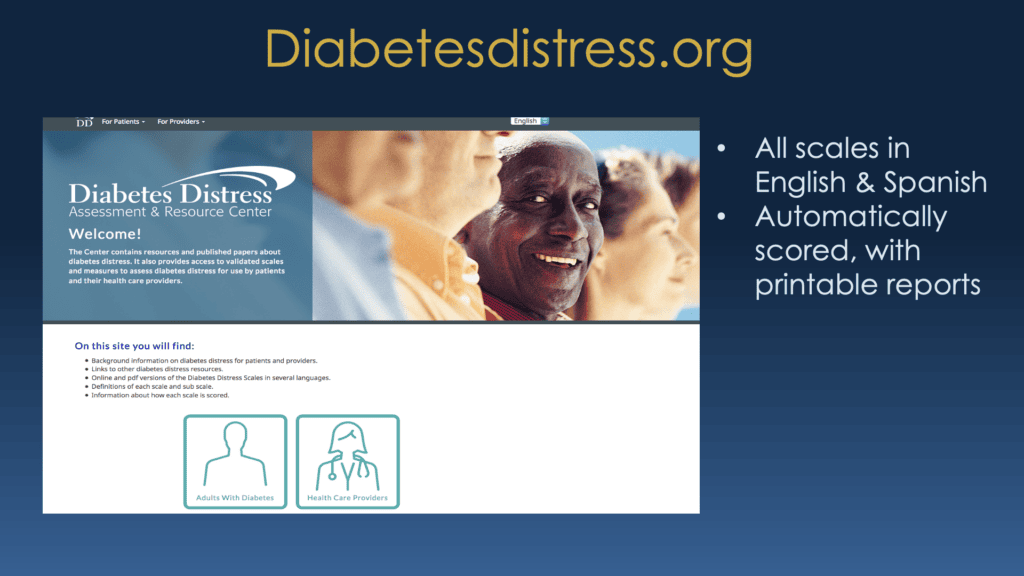
- Implement Routine Screening: Incorporate standardized questionnaires to identify patients experiencing diabetes distress. Examples include the Diabetes Distress Scale (DDS) or similar validated instruments. This ensures timely intervention and reduces the risk of prolonged distress.
- Offer Supportive Resources: Provide access to mental health professionals, support groups, and online resources specifically addressing diabetes distress. This may include referrals to counselors, psychologists, or diabetes support groups.
- Tailor Education: Develop patient education programs that address both the technical aspects of diabetes management and emotional well-being. This should include stress management techniques, coping mechanisms, and positive self-talk strategies.
- Promote Self-Management Skills: Encourage patients to develop self-management skills, including problem-solving, time management, and effective communication strategies. These strategies help patients navigate the challenges associated with diabetes.
- Foster a Supportive Environment: Create a supportive and empathetic environment within the healthcare setting. This includes encouraging open communication between patients and healthcare providers, ensuring a safe space for patients to express their concerns, and providing regular opportunities for emotional support.
Conclusion
In conclusion, new research diabetes distress reveals a multifaceted problem requiring a comprehensive approach. The research highlights the urgent need for healthcare professionals to understand the factors contributing to diabetes distress and to develop effective interventions. This knowledge is critical to improving the well-being of people with diabetes and promoting better health outcomes. Moving forward, the research suggests a path towards more compassionate and effective care, empowering individuals with diabetes to thrive.