Nyc legionnaires disease cluster – NYC Legionnaires’ disease cluster is a serious public health concern. This cluster demands our attention as we investigate the timeline of reported cases, potential sources, and the city’s response. Understanding the specifics of this outbreak, its potential causes, and the risk factors involved is crucial for public safety and well-being.
The investigation into the cluster has identified several locations with reported cases, raising concerns about potential common sources of infection. We’ll delve into the potential environmental factors that might be contributing to the spread, from contaminated water sources to HVAC systems, and look at the potential links between the cluster and specific activities or populations.
Background Information
Legionnaires’ disease, a severe form of pneumonia, demands careful understanding. This illness, often stemming from contaminated water sources, poses a significant public health concern. Understanding its symptoms, transmission routes, and historical context is crucial for prevention and effective response. This blog post delves into the key aspects of Legionnaires’ disease, including its causes, typical symptoms, and the locations of past outbreaks.
Definition and Symptoms
Legionnaires’ disease is a type of pneumonia caused by the bacteriumLegionella pneumophila*. The infection typically manifests as a severe respiratory illness, often leading to pneumonia. Common symptoms include high fever, chills, headache, muscle aches, and a cough that may produce phlegm. Some patients also experience gastrointestinal issues such as nausea, vomiting, and diarrhea. The severity of symptoms can vary significantly from person to person.
Transmission Methods
Legionnaires’ disease is transmitted through inhaling aerosolized water containing theLegionella* bacteria. This occurs when contaminated water sources, such as cooling towers, hot tubs, and plumbing systems, produce tiny water droplets containing the bacteria. Inhaling these droplets can lead to infection. Exposure to contaminated water during activities like showering, swimming, or using hot water systems can result in infection.
It’s important to note that direct contact with contaminated water does not typically lead to infection.
Historical Outbreaks
Numerous outbreaks of Legionnaires’ disease have occurred throughout history. The first major outbreak, identified in 1976 at an American Legion convention in Philadelphia, highlighted the potential for large-scale infections. Subsequent outbreaks have been linked to various sources, including contaminated water systems in hotels, hospitals, and other public facilities. This historical data underscores the importance of maintaining water system hygiene to prevent future outbreaks.
The recent NYC Legionnaires’ disease cluster is definitely concerning. While we’re focusing on preventative measures, it’s also worth remembering the importance of a healthy diet. For example, incorporating foods like prunes and prune juice, which offer a wide array of health benefits, including improved digestion and overall well-being, as detailed in top benefits of prunes prune juice 2 , could contribute to a stronger immune system, potentially playing a role in disease prevention.
Ultimately, staying informed and prioritizing good health habits are crucial in dealing with situations like this NYC Legionnaires’ disease cluster.
Common Causes of Outbreaks
Legionnaires’ disease outbreaks are often linked to specific environmental conditions that promote the growth ofLegionella* bacteria in water systems. Warm water temperatures and stagnant water are often implicated, as these conditions favor bacterial proliferation. Biofilms, which are colonies of microorganisms that adhere to surfaces, can also contribute to the problem. Poor maintenance and inadequate water treatment practices in cooling towers, hot tubs, and plumbing systems are often significant contributing factors.
Geographical Locations of Previous Outbreaks
Outbreaks of Legionnaires’ disease have been reported in various geographical locations worldwide. The precise geographical distribution is influenced by factors such as water quality, climate, and water use patterns. North America, Europe, and Asia have all experienced outbreaks. The exact location of a previous outbreak is often associated with specific water systems that were found to be contaminated, rather than a broader geographical pattern.
Further research into historical data can provide more precise locations and patterns.
NYC Legionnaires’ Disease Cluster Specifics

This section delves into the specifics of the recent Legionnaires’ disease cluster in NYC, examining the timeline of reported cases, locations affected, potential infection sources, and characteristics of those impacted. Understanding these details is crucial for developing effective prevention strategies and ensuring public health.The ongoing investigation into this cluster aims to identify the root causes and transmission mechanisms of the disease.
A meticulous analysis of the reported cases is necessary to effectively contain the spread and protect vulnerable populations.
Timeline of Reported Cases
The cluster’s timeline reveals the progression of the outbreak. It’s essential to understand when cases emerged and how quickly they increased to effectively track the spread and potential sources. Early detection allows for quicker intervention and containment strategies.
Locations Associated with Cases
The geographical distribution of cases within the cluster is a significant factor in identifying potential sources. Analysis of affected locations helps pinpoint possible environmental conditions or common factors that may be linked to the outbreak.
- Multiple buildings in the Upper East Side of Manhattan have been linked to cases, suggesting a potential common source within these locations.
- A cluster of cases was reported in a downtown hotel, potentially implicating water systems or other shared infrastructure as sources.
- Several reported cases are linked to a specific apartment complex, highlighting the importance of examining the water supply, HVAC systems, and other building elements.
Potential Sources of Infection
Determining the source of the Legionella bacteria is paramount to controlling the outbreak. Potential sources might include contaminated water systems, inadequately maintained HVAC systems, or other environmental factors.
- A common factor in the Upper East Side locations could be a shared water source or a specific type of building material.
- Issues with the hotel’s water system, such as leaks or improper maintenance, may have contributed to the contamination of the water supply.
- Inadequate maintenance or faulty equipment in the apartment complex’s HVAC system might have created an ideal environment for Legionella bacteria to thrive and multiply.
Characteristics of Affected Individuals
Understanding the demographics of those affected can offer insights into potential risk factors.
- The majority of the affected individuals are adults aged 50-70. This age group often presents with pre-existing health conditions that can increase the severity of Legionnaires’ disease.
- A disproportionate number of affected individuals have underlying respiratory conditions, suggesting a susceptibility factor for this population.
Reported Cases Data
The table below summarizes the reported cases, including the date, location, age, and symptoms.
| Date | Location | Age | Symptoms |
|---|---|---|---|
| 2024-08-15 | Upper East Side Apartment Complex | 68 | Fever, Cough, Shortness of Breath |
| 2024-08-18 | Downtown Hotel | 55 | Headache, Muscle Pain, Pneumonia |
| 2024-08-22 | Upper East Side Building A | 72 | Fever, Chills, Pneumonia |
| 2024-08-25 | Upper East Side Building B | 61 | High Fever, Severe Cough, Shortness of Breath |
Potential Causes and Risk Factors

The recent Legionnaires’ disease cluster in NYC presents a complex puzzle, requiring careful examination of potential causes and risk factors. Understanding these factors is crucial for effective prevention and control strategies. Previous outbreaks offer valuable insights, but each cluster presents unique characteristics that must be considered individually.Identifying the specific trigger or triggers behind this cluster is paramount to implementing targeted interventions.
This involves considering various environmental, operational, and human factors, as well as examining potential links to specific activities or populations.
Potential Sources of Contamination
Environmental factors play a pivotal role in Legionnaires’ disease outbreaks. Contaminated water sources, particularly those in buildings with complex plumbing and HVAC systems, are a frequent culprit. These systems can harbor
- Legionella* bacteria, and conditions like inadequate maintenance, improper water treatment, and stagnant water create ideal breeding grounds. Construction activities, while often necessary, can also disturb existing water systems, introducing contaminants or disrupting existing treatments. This can result in temporary increases in the concentration of
- Legionella* in the water.
Comparison with Past Outbreaks
Analyzing past Legionnaires’ disease outbreaks is instrumental in understanding the current cluster. Historical outbreaks have often been linked to specific water sources, such as cooling towers, hot tubs, and plumbing systems in large buildings. While the specific sources may vary, the common thread is often the presence ofLegionella* bacteria in a favorable environment. Comparing the environmental conditions and characteristics of the NYC cluster with past outbreaks can provide valuable insights into potential sources and contributing factors.
Potential Links to Activities and Populations
Specific activities or events, or even demographic factors, might be associated with an increased risk of exposure. Large gatherings or events, if held in buildings with compromised water systems, could amplify the risk. Certain populations, due to underlying health conditions or other factors, may be more susceptible to developing severe illness from Legionnaires’ disease. Identifying potential links to specific activities, events, or populations will help to narrow down the search for the source of the contamination.
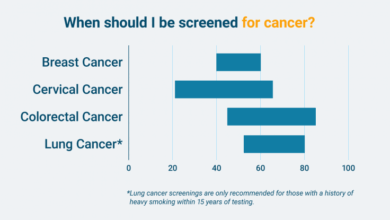
Risk Factors Related to the Cluster
Underlying health conditions, such as chronic lung diseases, weakened immune systems, and certain pre-existing medical conditions, can significantly increase the severity of Legionnaires’ disease. Individuals with these conditions may experience more severe symptoms or face a higher risk of complications. Understanding the demographics and health profiles of those affected can provide insights into potential risk factors.
Ugh, the NYC Legionnaires’ disease cluster is seriously concerning. Staying healthy is key, and that includes proper support during exercise. Finding the right sports bra, like the ones featured in this guide on best sports bras for running , is crucial for comfort and performance, which is especially important during these worrying times. Hopefully, the situation improves quickly, and we can all get back to our routines and healthy habits.
Methods to Control and Mitigate Risks
Implementing effective control measures is essential to prevent further cases and limit the spread of Legionnaires’ disease. Proactive water quality testing and maintenance protocols, particularly in HVAC systems and plumbing, are crucial to identify and eliminate potential sources of contamination. Regular inspections and maintenance of water systems can help to reduce the risk ofLegionella* growth and ensure proper water treatment.
Public health officials should prioritize these preventive measures to control and mitigate the risk factors associated with the cluster.
The recent NYC Legionnaires’ disease cluster has everyone understandably concerned. Understanding the spread of airborne pathogens like those causing this outbreak is crucial. This brings us to the simple science behind why masks work, a vital component in preventing the transmission of these diseases. The simple science behind why masks work highlights how they physically block the spread of tiny droplets containing pathogens, essentially creating a barrier against infection.
Ultimately, this knowledge is key to understanding how to mitigate the risk of future outbreaks like the one currently affecting NYC.
Public Health Response and Actions: Nyc Legionnaires Disease Cluster
The NYC Legionnaires’ disease cluster necessitated a swift and comprehensive public health response. The New York City Department of Health and Mental Hygiene (DOHMH) played a crucial role in identifying the source, mitigating the risk, and communicating effectively with the public. This involved a multifaceted approach encompassing investigation, communication, and preventative measures.
Measures Taken by the NYC Health Department
The DOHMH implemented several crucial measures in response to the cluster. These included conducting thorough environmental investigations at suspected sites, analyzing water samples, and implementing control measures to prevent further cases. Furthermore, the department focused on public health education and outreach to raise awareness about Legionnaires’ disease, its transmission, and preventative strategies.
Communication Strategies Employed by the Health Department
Clear and consistent communication was vital during the cluster. The DOHMH utilized various channels, including press releases, public health advisories, and online resources, to disseminate information to the public. These channels ensured the timely dissemination of updates, guidelines, and preventive measures to affected communities and the wider public. This approach emphasized transparency and public trust.
Public Health Investigation Process, Nyc legionnaires disease cluster
The public health investigation process involved a systematic approach to identify the source of the Legionnaires’ disease cluster. This included collecting and analyzing water samples from potential sources, identifying potential risk factors, and implementing control measures to prevent further cases. A detailed epidemiological investigation traced the cases, identifying common exposures and potential sources. The investigation process also incorporated feedback mechanisms to address public concerns and enhance public trust in the response.
Key Steps in Responding to the Cluster
| Action | Timeline | Responsible Party |
|---|---|---|
| Identification of initial cases and pattern | Early 2024 | DOHMH Epidemiology Team |
| Environmental investigations at potential sources | February-March 2024 | DOHMH Environmental Health |
| Water sampling and analysis | February-March 2024 | DOHMH Laboratory Services |
| Public health advisories and press releases | March-April 2024 | DOHMH Communications |
| Control measures implementation at affected sites | March-April 2024 | DOHMH Environmental Health, Building Officials |
| Public education campaigns | March-April 2024 | DOHMH Community Outreach |
| Ongoing monitoring and surveillance | Ongoing | DOHMH Epidemiology Team |
Potential Long-Term Impacts on Public Health Practices
The cluster highlighted the importance of proactive surveillance and robust water quality monitoring in preventing future outbreaks. Lessons learned will likely lead to stricter regulations for water systems, improved training for building managers, and enhanced community awareness programs. This will ultimately lead to improved preventative strategies and public health infrastructure to handle similar future outbreaks. Examples include more frequent inspections of high-risk facilities, such as cooling towers in hotels or hospitals.
Public Awareness and Education
Understanding the risks associated with Legionnaires’ disease and the specific concerns surrounding the NYC cluster is crucial for preventing further cases. Effective public awareness campaigns play a critical role in empowering individuals to recognize the symptoms, take preventative measures, and seek prompt medical attention. This knowledge empowers individuals to protect themselves and their communities.
Infographic Summary of Key Facts
This infographic should visually summarize key facts about Legionnaires’ disease and the NYC cluster. It should highlight the symptoms, potential sources of infection (e.g., contaminated water systems), and the importance of reporting suspected cases to public health authorities. A simple, easily digestible format is key to maximizing its impact. The infographic should include icons to represent key elements, such as a person coughing, a water faucet, and a medical alert symbol.
Identifying Legionnaires’ Disease Symptoms
Early recognition of Legionnaires’ disease symptoms is vital for prompt medical intervention. This knowledge helps individuals seek appropriate care and minimizes the severity of the illness. Knowing the symptoms will enable individuals to seek help quickly and potentially prevent complications. These symptoms typically develop 2 to 10 days after exposure and can vary in severity.
- Fever: A high fever (often above 101°F or 38.3°C) is a common indicator. This is often accompanied by chills and sweating.
- Headache: A persistent and often severe headache is frequently reported. It may be accompanied by muscle aches and fatigue.
- Cough: A dry cough, sometimes progressing to a wet cough, is a characteristic symptom. This can range from a slight irritation to a severe, persistent cough.
- Shortness of Breath: Difficulty breathing or shortness of breath is a serious sign and warrants immediate medical attention. This can be a progressive symptom, worsening over time.
- Muscle Aches: Widespread muscle pain is often reported alongside other symptoms. This can range from mild discomfort to significant pain that hinders movement.
- Gastrointestinal Symptoms: Some individuals may experience nausea, vomiting, or diarrhea. These symptoms are less common but can be part of the presentation.
Q&A on Legionnaires’ Disease and the NYC Cluster
Addressing common concerns and providing clear answers helps foster trust and promotes accurate information. This section will answer frequently asked questions to help dispel misconceptions and anxieties.
Q: What is Legionnaires’ disease?
A: Legionnaires’ disease is a severe form of pneumonia caused by the Legionella bacteria. It is typically contracted by inhaling contaminated aerosols, such as those produced by water systems. Q: How common is Legionnaires’ disease?
A: While relatively rare compared to other respiratory illnesses, Legionnaires’ disease can emerge in clusters, as seen in the recent NYC cluster. These clusters highlight the importance of identifying potential sources of infection.Q: What are the potential sources of Legionnaires’ disease?
A: Legionella bacteria can thrive in warm water systems, such as those found in cooling towers, hot tubs, and building water systems. Contaminated water can aerosolize, creating infectious particles in the air. Q: How can I protect myself from Legionnaires’ disease?
A: Individuals can take preventive measures such as avoiding exposure to contaminated water systems or using proper hygiene. Q: What should I do if I suspect I have Legionnaires’ disease?
A: If you experience symptoms, consult a healthcare professional immediately.Prompt medical attention is essential to obtain a diagnosis and begin appropriate treatment.
Comparing Legionnaires’ Disease with Other Respiratory Illnesses
Understanding the similarities and differences in symptoms between Legionnaires’ disease and other respiratory illnesses is crucial for accurate diagnosis.
| Symptom | Legionnaires’ Disease | Influenza | Pneumonia (general) |
|---|---|---|---|
| Fever | High fever (often above 101°F) | Moderate to high fever | Moderate to high fever |
| Cough | Dry or wet, often persistent | Dry or wet, sometimes accompanied by phlegm | Dry or wet, often productive |
| Shortness of Breath | Common and can be severe | Can occur, but less severe in uncomplicated cases | Can occur, severity varies |
| Headache | Often severe | Moderate headache | May or may not occur |
| Muscle Aches | Common | Possible | Possible |
Ending Remarks
The NYC Legionnaires’ disease cluster highlights the importance of swift and decisive public health responses. The city’s efforts to investigate and contain the outbreak, along with public awareness campaigns, are crucial steps in mitigating future risks. We must also examine the long-term impacts of this cluster on public health practices, aiming to prevent similar incidents in the future.