Obamacare helped keep rural hospitals open, offering a lifeline to communities across America. Before the Affordable Care Act, many rural hospitals faced crippling financial struggles, threatening vital healthcare access. This article explores how the ACA’s provisions impacted these facilities, examining the factors that contributed to their pre-ACA vulnerabilities and the ways in which the law potentially mitigated those risks.
We’ll also look at alternative explanations for their continued operation, alongside the crucial role Medicaid expansion played.
The analysis will delve into the specific healthcare services offered by rural hospitals, examining how the ACA might have affected demand and costs. We’ll present illustrative data visualizations to further solidify the discussion, offering a clear picture of the trends in closures before and after the ACA’s implementation, and comparing financial performance across states.
Rural Hospital Viability Before Obamacare
Rural hospitals, crucial components of healthcare access in underserved areas, faced significant financial challenges before the Affordable Care Act (ACA) was implemented. These institutions, often serving as the sole providers of medical services in their communities, were particularly vulnerable to economic downturns and shifting healthcare landscapes. Understanding their precarious situation prior to the ACA’s reforms helps contextualize the positive impact of the legislation.The economic landscape of rural hospitals before the ACA was characterized by a confluence of factors.
Limited patient volume, often stemming from lower population densities and a higher proportion of elderly and uninsured individuals, contributed to reduced revenue streams. Additionally, escalating healthcare costs, including expensive equipment and staff salaries, put further strain on already limited resources. The rising costs of medical technology, coupled with the increasing complexity of medical procedures, presented a significant hurdle for rural facilities.
Financial Health of Rural Hospitals Pre-ACA
Historical data reveals a concerning trend in the financial health of rural hospitals before the ACA. Many rural hospitals operated on thin margins, often with limited revenue to cover operating expenses. Reduced reimbursements from insurers, particularly for Medicaid and Medicare patients, frequently strained their budgets. In some cases, these factors led to substantial losses, placing these facilities at risk of closure.
Factors Contributing to Economic Challenges
Several factors contributed to the economic woes of rural hospitals prior to the ACA. The aging infrastructure of these facilities, often requiring significant capital investments for repairs and upgrades, was a significant burden. Furthermore, competition from larger, more established hospitals in urban areas, along with the increasing prevalence of managed care, further exacerbated their financial struggles. Limited access to capital and funding for expansion or modernization also hindered their ability to compete.
Examples of Rural Hospitals Facing Closure
Numerous rural hospitals faced closure or significant financial distress before the ACA. The lack of alternative healthcare options in their communities often left patients with few choices. For instance, a rural hospital in a sparsely populated region of the Midwest, offering primary care, emergency services, and obstetrics, faced mounting debt and potential closure. The loss of such a vital facility would have had a profound impact on the region’s overall health.
Types of Services Offered and Dependence on Patient Populations
Rural hospitals often provided a range of essential medical services, including emergency care, primary care, and specialized services such as obstetrics and pediatrics. Their patient populations were often reliant on these services due to a lack of alternatives. The presence of a high proportion of elderly patients, individuals with chronic conditions, and those with limited financial resources significantly influenced the hospital’s revenue streams and service offerings.
Obamacare’s impact on rural hospitals is pretty significant, and it’s something I’ve always been interested in. It seems to have played a crucial role in keeping them afloat, which is great news. However, it’s interesting to compare that to the recent Olympic figure skating scandal and the use of banned drugs. For example, this article on the Olympic figure skating scandal and banned drugs highlights the importance of fair play and ethical considerations.
Ultimately, though, the long-term effects of healthcare reform, like Obamacare, and their positive impact on rural communities are a key topic for ongoing discussion and study.
Many of these hospitals also provided specialized care, including surgical services, which were essential for the well-being of the community.
Obamacare’s impact on rural hospitals was significant, helping to keep many of them afloat. The healthcare industry is one of the fastest growing sectors, driven by innovation and evolving needs, as explored in this fascinating article about healthcare among fastest growing industries. This robust industry growth, in turn, underscores the importance of initiatives like Obamacare, which ensured crucial access to care, especially in underserved rural communities, keeping vital facilities open.
Geographical Distribution and Density
Prior to the ACA, rural hospitals were geographically dispersed, with a lower density in rural areas compared to urban areas. This distribution reflected the population density and the relative need for healthcare services in different regions. A map illustrating the geographic distribution would show a concentration of rural hospitals in areas with lower population density, often serving as the primary healthcare providers for a large area.
Impact of Obamacare on Rural Hospitals
The Affordable Care Act (ACA), often referred to as Obamacare, aimed to expand health insurance coverage, potentially impacting the financial stability and operations of rural hospitals. While the law’s intention was to improve access to care, its effect on rural facilities has been complex and multifaceted, presenting both challenges and opportunities. Understanding the nuances of this impact is crucial for policymakers and healthcare providers alike.The ACA introduced several provisions that could influence rural hospitals.
These provisions varied from subsidies for low-income individuals to expanded Medicaid eligibility, aiming to increase the number of insured individuals, thereby potentially increasing patient volume and revenue for these facilities. However, the specific impact of these provisions varied significantly depending on the specific context of individual rural hospitals and their local communities.
ACA Provisions Affecting Rural Hospitals
The ACA’s provisions aimed at increasing access to affordable healthcare influenced rural hospitals in several ways. Medicaid expansion, a key component, directly impacted the financial viability of rural hospitals by increasing the number of eligible patients. Subsidies for individuals purchasing health insurance through the marketplace could also bring more insured patients to these hospitals. These changes had the potential to improve revenue streams for rural hospitals, but also brought challenges related to cost management and patient demographics.
Financial Performance of Rural Hospitals Post-ACA
The financial performance of rural hospitals after the ACA’s implementation has been a subject of ongoing research and debate. Some studies have shown a mixed bag of results, with some hospitals experiencing improved financial stability while others faced challenges. The extent of improvement often depended on factors like the specific provisions of the ACA utilized in a particular region, local economic conditions, and the hospital’s ability to adapt to changes in patient demographics and needs.
Factors such as increased administrative costs and the complexities of handling a larger, potentially more diverse patient population also influenced financial outcomes.
Obamacare’s impact on rural hospitals is pretty significant, helping to keep them afloat. While we’re on the topic of things that might seem out of place, have you ever wondered if head lice actually jump? It’s a question that pops up from time to time, and you can find out the answer to that fascinating question here: do head lice jump.
Ultimately, though, the crucial point remains that the Affordable Care Act was instrumental in preventing the closure of many vital rural hospitals.
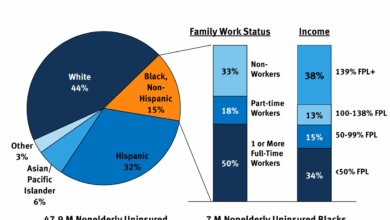
Changes in Patient Volume and Demographics
Patient volume and demographics at rural hospitals after the ACA’s implementation showed notable shifts. Increased access to insurance through the ACA and Medicaid expansion meant that rural hospitals saw an increase in insured patients. However, this increase wasn’t uniform across all facilities. The demographics of patients also changed. For example, hospitals in areas with higher proportions of low-income populations saw a larger influx of patients utilizing the ACA subsidies.
This shift necessitated adjustments in staffing, service offerings, and infrastructure for some rural hospitals.
Impact of Subsidies and Coverage Expansion
The subsidies offered through the ACA’s marketplace were intended to reduce the financial burden on individuals purchasing health insurance. This, in theory, could lead to more insured patients seeking care at rural hospitals. However, the actual impact on rural hospital finances was often nuanced. The effectiveness of these subsidies depended on the availability of healthcare providers in the area and the accessibility of care.
Increased coverage also brought about potential increases in the demand for services, which might have put pressure on existing resources and infrastructure.
Cost Reduction and Revenue Enhancement Mechanisms
To adapt to the changes brought about by the ACA, rural hospitals needed to implement strategies for cost reduction and revenue enhancement. One strategy was to explore collaborations with other rural hospitals to share resources, potentially reducing administrative costs and improving access to specialized services. Another strategy involved focusing on preventive care, potentially reducing the need for expensive emergency room visits and hospitalizations.
The success of these mechanisms often depended on the willingness of hospitals to embrace innovation and adapt to the changing healthcare landscape.
Alternative Explanations for Rural Hospital Stability

The Affordable Care Act (ACA), often called Obamacare, has been a significant topic in discussions about rural hospital viability. However, other factors can influence the health and sustainability of these institutions. Understanding the multifaceted role of these factors is crucial to a complete picture of rural hospital stability. Beyond the ACA’s impact, other support systems, community resources, and economic trends play a vital part in the ongoing operation of rural healthcare facilities.The stability of rural hospitals is a complex issue influenced by a multitude of interconnected factors, not solely the ACA.
Medicaid expansion, for instance, can significantly affect a hospital’s financial health, as it expands access to care for a broader population, including low-income individuals and families. The ACA’s impact on rural hospitals, while noteworthy, should be considered within the larger context of all contributing factors.
Medicaid Expansion’s Role in Rural Hospital Viability
Medicaid expansion, a key component of the ACA, can be a significant source of revenue for rural hospitals. By increasing access to healthcare for low-income individuals, it reduces the financial burden on hospitals that would otherwise care for uninsured patients. This influx of funding can help rural hospitals offset some of the challenges associated with lower patient volumes and limited access to specialized services.
Hospitals in states that expanded Medicaid have demonstrated improved financial stability compared to those in states that did not.
Comparison of ACA Strategies with Other Rural Healthcare Support Programs
Different strategies for supporting rural healthcare exist beyond the ACA. For instance, federal funding programs and grants specifically targeted at rural hospitals can provide essential financial assistance. State-level initiatives, like the creation of rural healthcare funds or the development of community health centers, can also provide valuable resources. A comprehensive evaluation of rural healthcare support should consider these different approaches, comparing their respective strengths and weaknesses in terms of effectiveness, accessibility, and sustainability.
Examples of Rural Hospitals Remaining Open Despite Challenges
Several rural hospitals have demonstrated resilience despite facing challenges not directly related to the ACA. Factors such as the development of innovative financial models, diversification of services, and strategic partnerships with other healthcare providers have contributed to their continued operation. Examples include hospitals that successfully implemented telehealth programs, expanded their outreach services, or developed strong community partnerships to reduce isolation and improve access to care.
A case study analysis of these hospitals could reveal successful strategies that can be replicated elsewhere.
Factors Beyond the ACA Contributing to Rural Hospital Operations
Beyond the ACA’s impact, various factors contribute to the continued operation of rural hospitals. These include community-based initiatives to improve healthcare access, increased investment in telehealth services, and proactive efforts by local governments to support healthcare infrastructure. Rural hospitals that have successfully navigated challenges frequently demonstrate adaptability, innovation, and community engagement. These examples demonstrate the multifaceted nature of rural healthcare support.
Potential Confounding Variables Influencing ACA-Rural Hospital Relationship
Several confounding variables can affect the relationship between the ACA and rural hospital survival. Economic trends in rural areas, changes in the demographics of the patient population, and the availability of alternative healthcare services can all influence a hospital’s financial health. Factors such as the prevalence of chronic diseases and the changing needs of the rural population need to be taken into consideration when evaluating the ACA’s impact on rural hospitals.
The interaction of these variables can either amplify or mitigate the ACA’s effect on hospital viability.
Specific Services Provided by Rural Hospitals

Rural hospitals play a crucial role in providing essential healthcare services to communities often lacking access to larger medical centers. Their services are vital for maintaining public health, particularly in areas with limited transportation options and fewer specialists. Understanding the types of services offered and their potential impact on sustainability is essential for developing effective support strategies.The Affordable Care Act (ACA) introduced significant changes to the healthcare landscape, potentially influencing both the demand for and cost of services provided by rural hospitals.
This analysis explores the specific services offered, the impact of the ACA, and how these factors interact to shape the financial viability of rural healthcare facilities.
Types of Healthcare Services Offered, Obamacare helped keep rural hospitals open
Rural hospitals typically provide a broad range of services, often acting as the primary healthcare providers for their communities. These facilities are often the only source of comprehensive care for many miles around, providing a vital link to the larger healthcare system.
| Service Type | Description | Potential Impact on Financial Sustainability |
|---|---|---|
| Emergency Services | Providing immediate care for critical illnesses and injuries. | High volume, often high cost, and crucial for community health. |
| Primary Care | Routine checkups, preventive care, and management of chronic conditions. | Crucial for maintaining patient health and reducing hospital readmissions. |
| Surgical Services | Performing surgeries for a range of conditions, including routine and complex procedures. | Significant financial impact, dependent on case volume and complexity. |
| Obstetrics and Gynecology | Providing prenatal care, childbirth services, and women’s health services. | Essential for maternal health and can be a significant revenue source. |
| Diagnostic Imaging | Offering X-rays, CT scans, and other imaging services. | Essential for diagnosis and treatment, can be expensive to maintain. |
| Laboratory Services | Performing tests and analyses to support diagnosis and treatment. | Essential support service, impacts patient outcomes. |
Impact of the ACA on Service Demand
The ACA’s expansion of health insurance coverage significantly impacted the demand for healthcare services, particularly in rural areas. Increased access to insurance led to a higher number of insured individuals seeking care, which could have positively affected the demand for primary care services. However, the effect on specialized services like cardiology or oncology might have been less pronounced, as these are often associated with higher out-of-pocket expenses.
Influence of the ACA on Service Costs
The ACA’s emphasis on preventative care and chronic disease management could lead to increased costs for certain services. For example, the increased need for screenings and management of chronic conditions could have led to higher costs associated with primary care services. Additionally, the shift towards value-based care, encouraging preventative care and population health management, could have placed additional financial burdens on rural hospitals, potentially needing to invest in new technologies or personnel.
Impact on Supply Chain and Specialized Equipment
The ACA’s provisions, while intending to improve access to care, might have affected the supply chain and access to specialized equipment for rural hospitals. For instance, the increased demand for certain medications or medical devices could have led to increased costs or supply chain challenges. Rural hospitals might face difficulties in obtaining specialized equipment or maintaining inventory levels.
Medicaid Expansion and Rural Hospitals: Obamacare Helped Keep Rural Hospitals Open
Rural hospitals often face unique challenges, including limited patient populations and high operating costs. Medicaid expansion, when implemented effectively, can play a crucial role in stabilizing these facilities. By increasing the number of insured patients, Medicaid expansion can bolster revenue streams and help rural hospitals maintain financial viability.Medicaid expansion is directly correlated with the survival of rural hospitals because it increases the number of insured patients.
This influx of patients, many of whom might not otherwise have access to care, provides a crucial revenue source. The increased volume of patients can offset some of the high operating costs associated with rural hospital operations, ultimately improving their financial stability.
Impact of Medicaid Expansion on Rural Hospitals
Medicaid expansion has demonstrated varying impacts on rural hospitals across different states. In states that expanded Medicaid, a noticeable trend of improved financial stability has been observed in many rural hospitals. This improvement is often linked to the increased patient volume and the associated revenue generated from the expanded insured population.
Examples of States with Medicaid Expansion and their Impact
Several states have expanded Medicaid, and the impacts on rural hospitals have been observed in various ways. For instance, states that expanded Medicaid often saw an immediate increase in the number of patients seeking care at rural hospitals. This influx of patients contributed to increased revenue and helped mitigate some of the financial pressures these hospitals faced.
States Without Medicaid Expansion and their Impact on Rural Hospitals
Conversely, in states that have not expanded Medicaid, rural hospitals often struggle to maintain financial stability. Without the increased patient volume that Medicaid expansion can provide, these hospitals may experience decreased revenue, potentially leading to reduced services or even closure in some cases.
Benefits of Medicaid Expansion for Rural Hospitals
Medicaid expansion offers several potential benefits for rural hospitals. Increased patient volume and revenue can directly contribute to improved financial stability. Furthermore, Medicaid expansion can help these hospitals provide necessary services to a broader segment of the community, thereby maintaining the provision of essential healthcare services in rural areas.
Drawbacks of Medicaid Expansion for Rural Hospitals
However, Medicaid expansion is not without its potential drawbacks. Increased administrative burdens and complexities related to billing and reimbursements can be significant challenges. Furthermore, the reimbursement rates for Medicaid services may be lower than those for private insurance, potentially impacting the hospitals’ profitability.
Financial Implications of Medicaid Expansion on Rural Hospital Operating Costs
The financial implications of Medicaid expansion on rural hospital operating costs are complex. While the increased patient volume can reduce operating costs per patient, the lower reimbursement rates for Medicaid services may partially offset this benefit. In some cases, the overall financial impact may be neutral, while in others, hospitals might see a net reduction in operating costs due to increased patient volume.
Illustrative Data Visualization
The Affordable Care Act (ACA) significantly impacted rural hospitals, and visualizing these trends provides crucial insights into its effects. Understanding the changes in closures, financial performance, patient volume, and the correlation with Medicaid expansion is essential to evaluate the ACA’s overall impact on rural healthcare. These visualizations can help stakeholders understand the complexities of rural healthcare and the potential benefits and challenges associated with the ACA.
Trends in Rural Hospital Closures Before and After the ACA
A line graph would effectively illustrate the trends in rural hospital closures before and after the ACA. The x-axis would represent the years, and the y-axis would display the number of hospital closures. The graph would show a clear comparison of the closure rates in the years leading up to the ACA’s implementation and the years following it.
This visualization would visually highlight any potential decrease in closure rates after the ACA’s implementation, demonstrating the Act’s possible role in stabilizing rural hospitals.
Financial Performance Comparison of Rural Hospitals
A bar chart could effectively compare the financial performance of rural hospitals in ACA-compliant and non-compliant states. The x-axis would represent the states, categorized as ACA-compliant or non-compliant. The y-axis would represent key financial metrics, such as net income, operating margins, or debt levels. The chart would clearly show the difference in financial health between the two groups of states, potentially demonstrating the impact of ACA provisions on rural hospital profitability.
The data would ideally be aggregated over a period of time, to provide a clearer understanding of long-term trends.
Change in Patient Volume at Rural Hospitals
A line graph, similar to the one used to illustrate closure trends, would be appropriate to show the change in patient volume at rural hospitals after the implementation of the ACA. The x-axis would represent time, and the y-axis would display the total patient volume. A clear trendline could show if the patient volume increased, decreased, or remained stable after the ACA’s enactment.
This visualization would help understand the ACA’s impact on access to care in rural communities.
Correlation Between Medicaid Expansion and Rural Hospital Financial Stability
A scatter plot would be a useful visualization to illustrate the correlation between Medicaid expansion and the financial stability of rural hospitals. The x-axis would represent the level of Medicaid expansion in each state (e.g., percentage of eligible residents enrolled in Medicaid). The y-axis would display a key financial metric like net income, operating margin, or debt levels for rural hospitals in each state.
This plot would visually display any correlation between increased Medicaid enrollment and improved financial health in rural hospitals.
Impact of the ACA on Access to Specific Healthcare Services
A series of bar charts or stacked bar charts could effectively show the impact of the ACA on access to specific healthcare services in rural areas. Each chart would represent a different service, such as primary care, specialist care, or mental health services. The x-axis would represent the years, and the y-axis would display the percentage of rural residents having access to each service.
The charts could highlight whether access to services increased or decreased in rural areas after the implementation of the ACA. This would help evaluate the ACA’s role in improving access to crucial healthcare services in rural areas.
Epilogue
In conclusion, while other factors likely played a role, the Affordable Care Act undeniably played a significant part in the survival of numerous rural hospitals. The ACA’s impact on patient volume, demographics, and the financial stability of these facilities is undeniable, particularly when considering the correlation with Medicaid expansion. This analysis underscores the importance of the ACA in maintaining access to healthcare in underserved rural communities.
While further research is always valuable, the evidence presented suggests a strong connection between the ACA and the ongoing operation of these vital facilities.