Obesity narrows airway leads to asthma, a complex interplay of factors impacting respiratory health. This article delves into the intricate relationship between excess weight, airway constriction, and the development of asthma. We’ll explore the anatomical changes, physiological mechanisms, and inflammatory processes that contribute to this association.
From the impact of different obesity types on airway narrowing to the effectiveness of various diagnostic methods, this discussion covers the full spectrum of this critical health issue. We will also examine management strategies, case studies, and public health implications, providing a comprehensive understanding of the problem.
Introduction to Obesity and Airway Narrowing
Obesity significantly impacts the respiratory system, leading to a complex interplay of structural and functional changes. Excess fat deposition around the airways and chest wall can restrict breathing capacity and contribute to respiratory conditions like asthma. Understanding the mechanisms behind this connection is crucial for developing effective preventative and therapeutic strategies.The accumulation of adipose tissue, particularly around the chest and upper airway, can physically compress the respiratory structures.
This compression reduces the space available for the lungs to expand and contract, impacting lung function and potentially triggering or exacerbating asthma symptoms. The consequences extend beyond mere discomfort, potentially affecting overall health and quality of life.
Obesity’s Impact on Respiratory Structures
Obesity affects various respiratory structures, leading to alterations in their function and dimensions. These changes, combined with the inflammatory response associated with excess fat, can make the airways more susceptible to constriction and inflammation, increasing the risk of asthma episodes.
Mechanisms of Airway Narrowing
Several mechanisms contribute to airway narrowing in obese individuals. Increased fat deposition around the upper airway, including the neck and upper chest, can physically compress the trachea and bronchi. This reduction in luminal space directly impacts airflow. Furthermore, the inflammatory response associated with obesity can lead to increased mucus production and airway inflammation, exacerbating the narrowing effect. Additionally, the mechanical strain on the respiratory muscles due to excess weight can reduce their efficiency, impacting the overall breathing process.
Anatomical Changes in the Respiratory Tract
Obesity induces several anatomical changes in the respiratory tract. The accumulation of fat in the chest wall can reduce the volume of the thoracic cavity, making it harder for the lungs to expand. The adipose tissue surrounding the airways can compress the tracheal and bronchial walls, leading to a reduction in the airway diameter. Furthermore, the increased weight of the upper body can put additional pressure on the diaphragm, impacting its effectiveness in driving respiration.
These combined effects contribute to reduced lung function and increased susceptibility to respiratory problems.
Types of Obesity and Their Relation to Airway Narrowing
Obesity is categorized into different types based on body mass index (BMI) and distribution of fat. Central obesity, characterized by fat accumulation around the abdomen and upper body, is strongly associated with airway narrowing. This type of obesity has a more significant impact on respiratory function compared to peripheral obesity. Furthermore, different degrees of obesity can correlate with varying degrees of airway narrowing.
Comparison of Obesity Levels and Airway Diameter
| Obesity Level (BMI) | Description | Estimated Effect on Airway Diameter |
|---|---|---|
| 18.5 – 24.9 | Healthy Weight | Normal |
| 25.0 – 29.9 | Overweight | Slight reduction |
| 30.0 – 34.9 | Obese Class I | Moderate reduction |
| 35.0 – 39.9 | Obese Class II | Significant reduction |
| 40.0+ | Obese Class III (Morbid Obesity) | Marked reduction |
This table provides a general overview. Individual responses to obesity can vary significantly.
Asthma and its Relationship to Obesity
Obesity and asthma share a complex interplay, impacting the health and well-being of millions globally. While distinct conditions, their connection is rooted in shared inflammatory pathways and physiological changes. Understanding this intricate relationship is crucial for developing effective prevention and treatment strategies.Obesity significantly increases the risk of developing asthma and exacerbates existing asthma symptoms. This is not simply a matter of correlation but a demonstrable link through various physiological mechanisms.
Obesity narrowing airways can unfortunately lead to asthma, a condition that significantly impacts breathing. While some might consider alternative procedures like fat freezing, a recent study highlights more complications than initially thought with this treatment. This study suggests a deeper look at the potential risks involved, which could further affect individuals trying to manage obesity-related respiratory issues.
Ultimately, understanding the link between obesity and asthma remains crucial for effective treatment strategies.
The interplay between these two conditions requires a nuanced understanding of their individual characteristics and their shared inflammatory responses.
Commonalities and Differences between Obesity and Asthma
Obesity and asthma, though distinct, share some overlapping characteristics. Both conditions are chronic, often requiring long-term management. Both can significantly impact quality of life, leading to reduced physical activity and social limitations. However, obesity is primarily characterized by excess body fat, while asthma is a chronic inflammatory disease of the airways. These differences in the fundamental nature of the conditions necessitate distinct approaches to diagnosis and treatment.
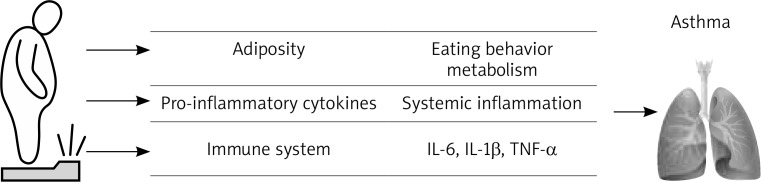
Physiological Mechanisms Linking Obesity to Asthma
Several physiological mechanisms connect obesity to asthma. Excess adipose tissue releases pro-inflammatory cytokines, substances that contribute to airway inflammation. These cytokines can trigger and exacerbate airway narrowing, a key feature of asthma. Furthermore, the increased weight and pressure on the chest can physically compress the airways, further reducing airflow. The resulting changes in lung function can manifest as increased symptoms and decreased quality of life.
Inflammatory Processes in Obese Individuals Susceptible to Asthma
Airways in obese individuals susceptible to asthma display increased inflammation. This is characterized by an elevated presence of inflammatory cells, such as mast cells and eosinophils, in the bronchial tissues. The presence of these cells releases inflammatory mediators, leading to the characteristic airway narrowing and hyperresponsiveness seen in asthma. The persistent inflammation can cause irreversible damage to the airways over time, resulting in more severe and frequent asthma attacks.
Obesity narrowing airways can lead to asthma, a condition often worsened by poor lifestyle choices. For example, overindulging during the Super Bowl, like the unhealthy pig-out described in how unhealthy pig out during super bowl , can significantly contribute to weight gain. This extra weight puts extra pressure on the respiratory system, making asthma symptoms worse and potentially triggering new episodes.
Prevalence of Asthma in Obese and Non-Obese Populations
Studies consistently demonstrate a higher prevalence of asthma in obese individuals compared to those with a healthy weight. This suggests a strong correlation between increased body mass index (BMI) and the likelihood of developing or experiencing more severe asthma. The increased risk is not limited to a particular age group but affects people across the lifespan.
Correlation between BMI and Asthma Risk
| BMI Category | Asthma Risk |
|---|---|
| Underweight (BMI < 18.5) | Lower risk |
| Normal weight (BMI 18.5-24.9) | Moderate risk |
| Overweight (BMI 25-29.9) | Increased risk |
| Obese (BMI ≥ 30) | High risk |
The table above provides a general overview. Individual experiences and responses to these conditions vary considerably. Genetic predispositions and environmental factors also play a crucial role in determining the risk of developing asthma in both obese and non-obese populations. It’s important to remember that this is not an exhaustive list and individual risk factors should be considered when assessing the potential for asthma development.
The Role of Inflammation in the Development of Asthma in Obese Individuals
Obesity significantly impacts the respiratory system, often contributing to the development and exacerbation of asthma. A key factor in this relationship is chronic inflammation, a complex process involving multiple mediators and immune cells. Understanding the specific inflammatory pathways activated in obese individuals with asthma is crucial for developing targeted therapies.Inflammation in obese individuals with asthma is characterized by a dysregulated immune response, which leads to an overactive inflammatory reaction in the airways.
This overreaction is a crucial element in the development and progression of the disease, as it contributes to airway narrowing, increased mucus production, and persistent inflammation. The interplay between adipose tissue and the immune system is central to this process, with adipose tissue acting as a significant source of inflammatory mediators.
Recent studies show that obesity significantly narrows airways, increasing the risk of asthma. This, coupled with the current political climate and the Trump administration’s efforts to dismantle the Affordable Care Act (ACA), trump administration sabotaging obamacare , could potentially lead to a surge in asthma cases, especially in vulnerable populations lacking access to affordable healthcare. It’s a concerning trend that needs serious attention and proactive solutions.
Inflammatory Mediators in Obesity-Related Asthma
The inflammatory response in obesity-related asthma involves a complex interplay of inflammatory mediators. These mediators include cytokines, chemokines, and lipid mediators, each contributing to the overall inflammatory cascade. Cytokines, such as TNF-α, IL-1β, and IL-6, are key players in initiating and sustaining the inflammatory response. Chemokines, such as CCL2 and CCL5, recruit immune cells to the site of inflammation.
Lipid mediators, including leukotrienes and prostaglandins, further amplify the inflammatory response and contribute to bronchoconstriction.
Interaction Between Adipose Tissue and the Immune System
Adipose tissue, commonly known as fat tissue, is not merely a storage depot for energy. It is an active endocrine organ that secretes a variety of adipokines, including leptin, adiponectin, and resistin. These adipokines can influence the immune system and contribute to the development of inflammation in the respiratory system. Leptin, for instance, can promote the production of pro-inflammatory cytokines, whereas adiponectin may have anti-inflammatory effects.
The balance between these adipokines is crucial in determining the overall inflammatory state of the body, and this balance is often disrupted in obesity. Dysregulation of adipokines may play a critical role in the development of asthma in obese individuals.
Immune Cells Involved in Airway Inflammation
Immune cells, such as mast cells, eosinophils, neutrophils, and T cells, play a critical role in the inflammatory response in the airways. Mast cells release histamine and other mediators, contributing to bronchoconstriction. Eosinophils are associated with allergic inflammation and are often elevated in asthma. Neutrophils are involved in the acute inflammatory response, and their presence in the airways can be indicative of severe inflammation.
T helper cells, particularly Th2 cells, are important in allergic responses and are often implicated in the development of asthma.
Alterations in Immune Response in Obese Individuals
Obesity alters the immune response in the respiratory system by shifting the balance toward a pro-inflammatory state. This alteration can lead to increased airway reactivity and susceptibility to asthma attacks. The increased presence of inflammatory mediators, the dysregulation of immune cells, and the interaction of adipose tissue with the immune system contribute to the overall inflammatory state. Obese individuals tend to have an exaggerated inflammatory response in the airways, which is a significant factor in the development and progression of asthma.
Key Inflammatory Markers in Obese Individuals with Asthma, Obesity narrows airway leads to asthma
| Inflammatory Marker | Description | Significance in Obesity-Related Asthma |
|---|---|---|
| TNF-α | Tumor Necrosis Factor-alpha | A potent pro-inflammatory cytokine, elevated levels are associated with increased airway inflammation and hyperresponsiveness. |
| IL-1β | Interleukin-1 beta | A pro-inflammatory cytokine, implicated in the initiation and perpetuation of the inflammatory response in the airways. |
| IL-6 | Interleukin-6 | A pro-inflammatory cytokine, implicated in the development of airway inflammation and remodeling. |
| CCL2 | Chemokine (C-C motif) ligand 2 | A chemokine that recruits immune cells, including macrophages and T cells, to the site of inflammation. |
| CCL5 | Chemokine (C-C motif) ligand 5 | A chemokine that attracts inflammatory cells to the airways, contributing to the recruitment of eosinophils and other immune cells. |
| Leptin | Adipokine | Elevated levels often associated with increased inflammation and airway hyperresponsiveness. |
| Adiponectin | Adipokine | Decreased levels may contribute to an inflammatory environment. |
Diagnostic Methods for Identifying Asthma in Obese Patients
Pinpointing asthma in obese individuals presents a unique challenge. Standard diagnostic approaches often fall short, leading to delayed or misdiagnosis. This can significantly impact treatment and patient outcomes. Understanding the nuances of these diagnostic methods is crucial for providing optimal care to this growing population.
Challenges in Standard Asthma Diagnosis for Obese Patients
Traditional asthma diagnostics often rely on symptoms and pulmonary function tests (PFTs). However, these methods can be less reliable in obese patients due to several factors. Obese individuals frequently exhibit overlapping symptoms with other conditions, making symptom-based diagnosis less accurate. Furthermore, the presence of excess adipose tissue can affect lung mechanics and the interpretation of PFT results.
This can lead to misdiagnosis, underdiagnosis, or overdiagnosis, impacting the patient’s treatment plan.
Pulmonary Function Tests (PFTs) and Their Applications
Pulmonary function tests (PFTs) are vital in assessing lung function. They measure various parameters like forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and peak expiratory flow rate (PEFR). These tests help evaluate airflow obstruction and airway responsiveness. In obese patients, however, the presence of excess body mass can artificially alter PFT results. For example, higher lung volumes and increased airway resistance can mask true airflow limitations.
Therefore, clinicians need to adjust interpretation strategies and consider alternative approaches to evaluate the patient’s actual lung function. PFTs are valuable, but clinicians need to be mindful of the potential biases introduced by obesity.
Comparison of Different Diagnostic Approaches
Several diagnostic approaches can be used to assess asthma in obese individuals. Spirometry, a common PFT, measures lung volumes and airflow rates. Methacholine challenge testing evaluates airway responsiveness. Exhaled nitric oxide (eNO) measurement assesses airway inflammation. The selection of the appropriate diagnostic approach depends on the patient’s specific clinical presentation and the severity of suspected asthma.
It is essential to consider the potential limitations of each method and combine multiple approaches for a more comprehensive assessment.
Summary Table of Diagnostic Procedures for Asthma in Obese Patients
| Diagnostic Procedure | Description | Potential Limitations in Obese Patients | Additional Considerations |
|---|---|---|---|
| Spirometry | Measures lung volumes and airflow rates. | Increased lung volumes and airway resistance can mask true airflow limitations. | Use predicted values adjusted for body size. |
| Methacholine Challenge Test | Evaluates airway responsiveness to a bronchoconstrictor. | Potential for altered airway reactivity due to obesity-related inflammation. | Consider the impact of obesity on bronchoconstriction. |
| Exhaled Nitric Oxide (eNO) Measurement | Assesses airway inflammation. | Potential for altered eNO levels due to obesity-related factors. | Correlation with other diagnostic methods is important. |
| Symptom Assessment | Evaluation of patient’s respiratory symptoms. | Symptoms may overlap with other conditions, making diagnosis less definitive. | Detailed symptom history is critical. |
Management Strategies and Treatments: Obesity Narrows Airway Leads To Asthma
Managing asthma in obese individuals requires a multifaceted approach that considers both the underlying obesity and the asthma itself. Effective strategies encompass medication, lifestyle modifications, and preventative measures. The goal is to not only control asthma symptoms but also to address the contributing factors of obesity, thereby improving overall health and quality of life.
Current Approaches to Managing Asthma in Obese Patients
Current approaches to managing asthma in obese patients prioritize a combination of pharmacological treatments and lifestyle interventions. This holistic strategy aims to reduce airway inflammation, improve lung function, and ultimately enhance the patient’s overall health and well-being. A crucial aspect of this approach is tailoring the management plan to the individual’s specific needs and circumstances, recognizing that each patient’s response to treatment can vary.
Treatment Options for Obese Individuals with Asthma
Various treatment options are available for obese individuals with asthma. These options range from inhaled corticosteroids to long-term control medications, each with its own mechanism of action and potential side effects. The choice of treatment depends on the severity of asthma, the individual’s response to previous therapies, and the presence of any other medical conditions.
Lifestyle Modifications in Managing Asthma in Obese Individuals
Lifestyle modifications play a vital role in managing asthma in obese individuals. These modifications focus on weight management, improved diet, increased physical activity, and stress reduction. Weight loss, even modest amounts, can significantly improve lung function and reduce asthma symptoms. A balanced diet rich in fruits, vegetables, and whole grains can contribute to better overall health, and regular physical activity strengthens the cardiovascular system and improves lung capacity.
Managing stress through relaxation techniques, such as meditation or yoga, can also be beneficial.
Preventive Measures to Mitigate the Impact of Obesity on Asthma Development
Preventive measures for mitigating the impact of obesity on asthma development focus on addressing the root causes of both conditions. Promoting healthy lifestyle choices from an early age is crucial. This includes encouraging a balanced diet, regular physical activity, and stress management techniques. Encouraging weight management through a combination of dietary changes, exercise, and behavior modification can effectively reduce the risk of developing asthma in obese individuals.
Regular checkups and early intervention for obesity can significantly lower the risk of asthma complications.
Table of Treatment Options for Obese Asthma Patients
| Treatment Option | Mechanism of Action | Potential Side Effects |
|---|---|---|
| Inhaled Corticosteroids | Reduce airway inflammation by suppressing the immune response. | Oral thrush, hoarseness, or dysphonia, in some cases, decreased bone density. |
| Long-Acting Beta-2 Agonists | Relax the airways by stimulating beta-2 receptors. | Tremors, palpitations, or nervousness, in some cases. |
| Leukotriene Modifiers | Reduce airway inflammation by inhibiting the action of leukotrienes. | Headache, nausea, or abdominal pain, in some cases. |
| Combination Inhalers | Combine the effects of inhaled corticosteroids and long-acting beta-2 agonists for better control. | Similar to those of individual components. |
| Oral Corticosteroids | Powerful anti-inflammatory agents, used for severe exacerbations. | Increased risk of osteoporosis, cataracts, or other side effects with prolonged use. |
Illustrative Case Studies
Obesity significantly impacts airway function, often exacerbating pre-existing asthma or triggering its development. Understanding the diverse presentations of this interplay is crucial for effective diagnosis and management. The following case studies highlight the variability in how obesity and asthma manifest, from mild to severe cases, and demonstrate the importance of personalized treatment approaches.
Case Study 1: Progressive Asthma in an Obese Adolescent
A 16-year-old female, previously diagnosed with mild asthma, presented with worsening symptoms. Her BMI was 35 kg/m². She experienced increasing breathlessness, particularly at night, and wheezing episodes triggered by exertion. Spirometry revealed reduced lung function, consistent with moderate persistent asthma. This case illustrates how obesity can progressively worsen pre-existing asthma, potentially leading to more frequent and severe exacerbations.
The challenge lay in differentiating between the effects of obesity and the progression of asthma, necessitating careful monitoring and adjustments to the treatment plan. The patient responded well to a combination of weight management strategies, including a balanced diet and increased physical activity, alongside an optimized asthma medication regimen.
Case Study 2: Asthma Masking as Obesity-Related Dyspnea
A 40-year-old male, obese with a BMI of 42 kg/m², presented with shortness of breath, a common complaint in obese individuals. He reported difficulty breathing, especially during exertion. Initial assessments focused on potential cardiovascular issues. However, detailed pulmonary function tests revealed airflow limitation consistent with mild asthma. The patient’s initial presentation mimicked other potential causes of dyspnea, highlighting the importance of comprehensive evaluation.
Respiratory assessments were crucial in identifying the underlying asthma. This case demonstrates how asthma symptoms can be masked by obesity-related respiratory issues, potentially leading to delayed or incorrect diagnosis.
Case Study 3: Successful Treatment Response in a Patient with Severe Asthma and Obesity
A 28-year-old female with a BMI of 40 kg/m² and a history of severe persistent asthma experienced frequent exacerbations requiring hospitalizations. She had limited response to standard asthma medications. The introduction of a multi-faceted treatment approach incorporating weight loss strategies (with a registered dietitian), inhaled corticosteroids, long-acting beta-agonists, and a bronchodilator significantly improved her lung function. The patient’s symptoms were controlled, and hospitalizations were drastically reduced.
This case showcases the positive impact of a comprehensive treatment plan combining weight management and asthma medication on the patient’s health and quality of life. The improved lung function is clearly linked to the combined treatment approach.
Summary Table of Case Studies
| Case Study | Patient Characteristics | Presentation | Challenges | Treatment | Outcome |
|---|---|---|---|---|---|
| 1 | 16-year-old female, BMI 35 kg/m², mild asthma | Progressive asthma symptoms | Differentiating obesity and asthma progression | Weight management, optimized asthma medication | Improved lung function, controlled symptoms |
| 2 | 40-year-old male, BMI 42 kg/m², dyspnea | Asthma masked by obesity | Delayed or incorrect diagnosis | Comprehensive respiratory assessment, asthma medications | Accurate diagnosis, symptom control |
| 3 | 28-year-old female, BMI 40 kg/m², severe asthma | Frequent exacerbations, limited response to standard medication | Severe uncontrolled asthma | Multi-faceted approach: weight loss, optimized asthma medications | Reduced exacerbations, improved lung function, improved quality of life |
Prevention and Public Health Implications
Obesity-related asthma poses a significant public health challenge, demanding proactive preventative measures and comprehensive community interventions. Effective strategies are crucial for mitigating the escalating burden of both conditions, impacting individuals and straining healthcare systems. Addressing the underlying factors that contribute to obesity and asthma is paramount in achieving long-term health improvements.
Preventative Measures to Mitigate Obesity-Related Asthma Risk
Strategies to prevent obesity and its associated asthma risk are multifaceted, focusing on lifestyle modifications and environmental factors. These measures aim to promote healthy habits from early childhood and throughout life.
- Promoting Healthy Diets: Early childhood nutrition plays a vital role in establishing healthy eating patterns. Parents and caregivers can implement strategies that encourage consumption of fruits, vegetables, and whole grains while limiting processed foods, sugary drinks, and unhealthy fats. School-based nutrition programs and community gardens can be valuable resources to promote healthier food choices within communities. For instance, implementing a “fruits and vegetables for all” program in schools could drastically improve dietary habits among children.
- Encouraging Physical Activity: Promoting regular physical activity is essential for weight management and respiratory health. This includes incorporating physical activity into daily routines, such as taking the stairs instead of the elevator, walking or cycling to school or work, and participating in organized sports or recreational activities. Creating accessible parks and playgrounds in communities can facilitate outdoor activities for children and adults alike.
Community-based fitness programs can also play a significant role in encouraging physical activity.
- Addressing Environmental Factors: Exposure to air pollutants, allergens, and other environmental factors can exacerbate asthma symptoms and contribute to weight gain. Public health initiatives should focus on reducing exposure to these environmental hazards. This may involve implementing stricter regulations on air pollution, promoting the use of public transportation, and encouraging the use of environmentally friendly products.
Public Health Implications of the Correlation
The link between obesity and asthma has substantial public health implications. Increased rates of obesity directly correlate with higher incidences of asthma, leading to increased healthcare costs, reduced productivity, and diminished quality of life for affected individuals. The societal impact is substantial, demanding comprehensive public health strategies.
- Increased Healthcare Costs: The management of obesity-related asthma requires substantial healthcare resources. Increased hospitalizations, emergency room visits, and long-term medication costs strain healthcare systems, potentially impacting access to other vital healthcare services.
- Reduced Productivity: Asthma exacerbations can lead to missed work or school days, resulting in reduced productivity and economic losses for individuals and communities.
- Diminished Quality of Life: Asthma can significantly impact daily activities and overall well-being, leading to reduced quality of life for affected individuals.
Community-Level Interventions
Community-based interventions are essential to effectively address the complex issue of obesity-related asthma. These interventions aim to promote healthy lifestyles and provide access to resources within communities.
- Community-Based Education Programs: Educational programs aimed at promoting healthy lifestyles, including nutrition and physical activity, can be implemented in community centers, schools, and workplaces. These programs can provide practical information and support to individuals and families in adopting healthier habits.
- Partnerships with Local Businesses: Collaborating with local businesses can provide access to healthy food options and promote physical activity within communities. For example, restaurants could offer healthier menu choices, and workplaces could implement wellness programs.
- Policy Changes: Policies that support healthy lifestyles, such as zoning regulations that promote access to parks and green spaces, and policies that limit the availability of unhealthy foods in schools, can create supportive environments for individuals to adopt healthier behaviors.
Importance of Early Detection and Management Strategies
Early detection and management of obesity and asthma are critical for preventing severe health complications and improving long-term outcomes. Effective strategies for early identification and intervention can significantly impact individuals’ health trajectories.
- Early Diagnosis: Prompt diagnosis and intervention are essential for preventing the progression of asthma and associated complications. Regular check-ups and screenings can aid in early identification of both obesity and asthma, facilitating timely interventions.
- Personalized Treatment Plans: Personalized treatment plans, tailored to the specific needs of each individual, are crucial for effective management. This includes addressing underlying factors, such as nutrition, physical activity, and environmental triggers.
Effectiveness of Prevention Strategies
| Prevention Strategy | Effectiveness | Potential Challenges |
|---|---|---|
| Promoting healthy diets | High; can lead to sustained weight management and improved respiratory health | Requires sustained effort and cultural shifts |
| Encouraging physical activity | High; can lead to weight management and improved respiratory function | Requires infrastructure support and community engagement |
| Addressing environmental factors | Moderate; can reduce exposure to triggers but may not address underlying causes | Requires policy changes and community awareness |
End of Discussion

In conclusion, the link between obesity and asthma is undeniable, and understanding this connection is crucial for improved prevention and treatment strategies. Addressing the inflammatory responses, lifestyle factors, and early detection methods associated with this condition are vital steps towards better managing and mitigating its impact on public health.