Pain relief central pain syndrome is a complex condition affecting the central nervous system, causing chronic and often debilitating pain. Understanding the underlying mechanisms, diverse symptoms, and available treatment options is crucial for effective management. This exploration delves into the intricacies of this syndrome, from its definition and diagnostic criteria to the impact on daily life and promising future research.
This comprehensive guide will provide a detailed overview of central pain syndrome (CPS), exploring its various facets, from the underlying neurological processes to the practical implications for patients. We’ll cover everything from the diagnostic process to treatment strategies, shedding light on the unique challenges associated with managing CPS effectively.
Defining Central Pain Syndrome
Central pain syndrome (CPS) is a complex neurological condition characterized by persistent and often debilitating pain that arises from damage or dysfunction within the central nervous system (CNS). Unlike peripheral neuropathic pain, which originates from damage to the nerves outside the brain and spinal cord, CPS involves the brain’s misinterpretation of sensory signals. This misinterpretation leads to heightened pain responses, even in the absence of a clear physical cause.
Understanding CPS requires a nuanced approach to its pathophysiology, types, diagnosis, and comparison to other pain conditions.
Pathophysiology of Central Pain Syndrome
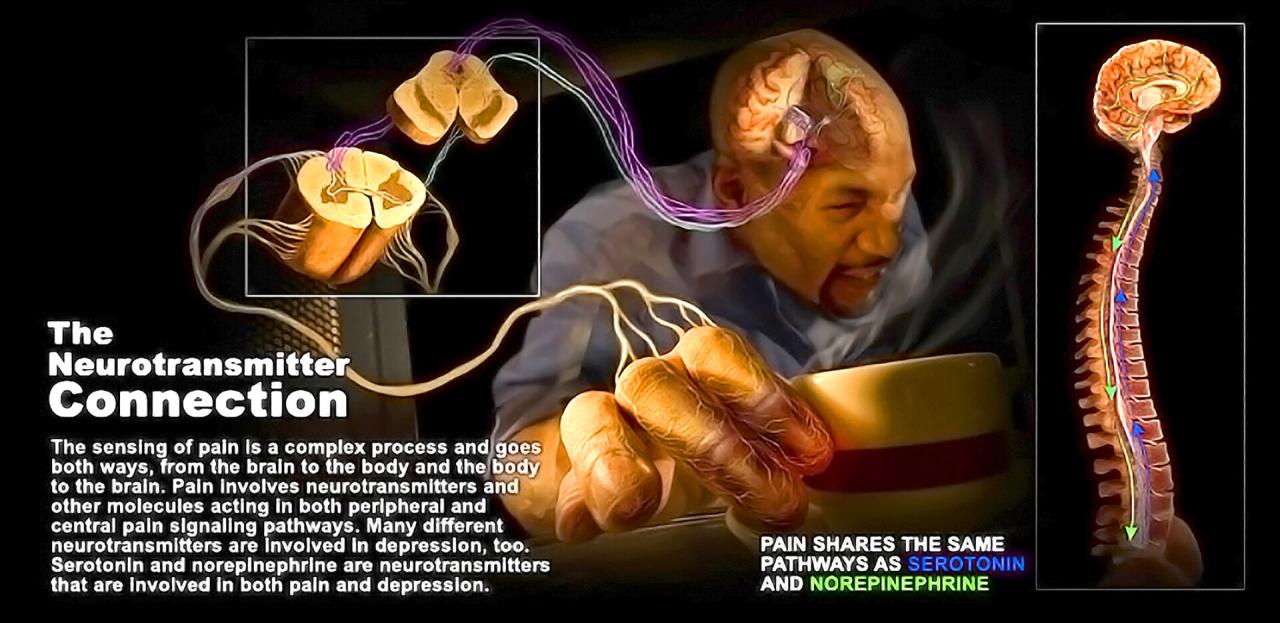
Central pain syndrome stems from a disruption in the normal processing of sensory information within the central nervous system. This disruption can manifest in various ways, including changes in the excitability of neurons in the spinal cord and brain. The exact mechanisms underlying these changes are not fully understood, but several factors are implicated, including: altered neurotransmitter levels, changes in the structure and function of synapses, and inflammatory processes within the CNS.
These alterations lead to the amplification of pain signals, creating a heightened sensitivity to stimuli that would not normally be perceived as painful. The resulting pain is often described as burning, shooting, or stabbing, and can be localized or widespread. The intensity of the pain can fluctuate, and may be triggered by seemingly innocuous stimuli, unlike peripheral neuropathic pain.
Types of Central Pain Syndrome
While not rigidly categorized, CPS can be associated with specific underlying conditions. These include stroke, multiple sclerosis, traumatic brain injury, and spinal cord injury. Each condition can contribute to a unique presentation of CPS, though the core pathophysiological mechanisms remain consistent. The specific symptoms and characteristics can vary depending on the location and extent of the CNS damage.
For example, someone experiencing CPS following a stroke might exhibit pain in the face or arm, while someone with spinal cord injury might experience widespread pain throughout the body.
Diagnostic Criteria for Central Pain Syndrome
Diagnosing CPS relies on a combination of clinical evaluation and exclusionary criteria. Physicians must rule out other potential causes of chronic pain, including peripheral nerve damage, musculoskeletal disorders, and psychiatric conditions. Key diagnostic criteria include: the patient’s history, neurological examination, and often, imaging studies. The history should emphasize the onset, location, and characteristics of the pain, as well as any associated neurological symptoms.
The neurological examination should assess for signs of central nervous system dysfunction. Imaging studies may help identify underlying conditions, such as lesions or structural abnormalities.
Comparison of Central Pain Syndrome and Peripheral Neuropathic Pain
| Feature | Central Pain Syndrome | Peripheral Neuropathic Pain |
|---|---|---|
| Location of injury | Central nervous system (brain, spinal cord) | Peripheral nervous system (nerves outside the brain and spinal cord) |
| Symptoms | Often described as burning, shooting, or stabbing; can be widespread; often triggered by non-painful stimuli; frequently fluctuating intensity. | Often described as tingling, numbness, or sharp, shooting pain; typically follows a specific nerve distribution; often associated with a clear injury or condition. |
| Treatment | Treatment strategies often focus on modulating central nervous system activity, including medication for pain relief, antidepressants, and anticonvulsants. Physical therapy and psychological support may also play a crucial role. | Treatment strategies often focus on managing the underlying cause of the peripheral nerve damage, including medications to reduce inflammation and nerve pain, and physical therapy. |
Symptoms and Manifestations
Central Pain Syndrome (CPS) presents a complex tapestry of symptoms, often defying easy categorization. The variability in individual experiences makes diagnosis challenging, requiring careful consideration of each patient’s unique constellation of sensations. Understanding the diverse range of symptoms is crucial for both accurate diagnosis and effective management strategies.The hallmark of CPS is the experience of chronic, often debilitating pain that extends beyond the usual expected response to a stimulus.
This pain can manifest in various ways, impacting physical function, emotional well-being, and overall quality of life. The intensity and character of the pain can fluctuate significantly, and this variability adds another layer of complexity to the condition.
Common Symptoms
The symptoms of CPS can be quite widespread, often extending beyond the area of initial injury or trauma. Patients frequently report sensations that are not easily explained by conventional pain mechanisms. These include, but are not limited to, deep, aching pain, burning sensations, and sharp, shooting pains.
Central pain syndrome can be a real challenge, making everyday life tough. While exploring potential pain relief strategies, it’s interesting to consider how certain nutrients might influence the aging process. For instance, could this version of vitamin B3 actually slow aging? could this version of vitamin b 3 slow aging is an intriguing area of research.
Ultimately, more research is needed to fully understand how this could impact pain relief in central pain syndrome.
Uncommon Symptoms
While the common symptoms are fairly well-documented, uncommon manifestations of CPS are less frequently discussed. Some patients experience hypersensitivity to light touch, temperature fluctuations, or even sounds. These heightened responses can significantly impact daily activities and social interactions.
Variability in Symptom Presentation
A key characteristic of CPS is the significant variability in symptom presentation across individuals. One person might experience primarily burning pain in a specific limb, while another might report a constellation of shooting pains throughout the body. This variability underscores the importance of a personalized approach to diagnosis and treatment.
Pain Qualities
The quality of pain experienced by those with CPS can range from dull aches to sharp, stabbing sensations. The table below provides a glimpse into the different types of pain commonly reported.
| Pain Quality | Description | Frequency in CPS |
|---|---|---|
| Burning | A persistent, intense, and often localized sensation of heat, similar to a continuous flame. This can range from a mild warmth to an excruciatingly painful feeling. | High |
| Shooting | A sudden, intense, and often brief pain that travels along a nerve pathway. This can feel like an electric shock or a piercing sensation. | Moderate |
| Stabbing | A sharp, localized, and often sudden pain that feels like a pointed object penetrating the skin or tissue. It can be intense and brief, or more persistent. | Moderate |
| Aching | A deep, dull, and often persistent pain that feels diffuse and spread throughout a region or area. | High |
Psychosocial Impacts of Chronic Pain
Chronic pain, a hallmark of CPS, can have significant psychosocial impacts. Patients may experience feelings of isolation, anxiety, and depression due to the persistent discomfort and limitations on daily activities. Difficulties in social interactions and maintaining relationships are common. This can lead to decreased participation in work or social activities.
Sleep Disturbances
The pain and associated symptoms can frequently disrupt sleep patterns. Difficulty falling asleep, staying asleep, or experiencing restless sleep are common complaints. This sleep disruption can exacerbate pain and contribute to feelings of fatigue and exhaustion.
Cognitive Impairments
CPS can also impact cognitive function. Patients may experience difficulties with concentration, memory, and problem-solving. This is often attributed to the chronic stress and pain associated with the condition. For example, a patient might struggle to focus on tasks at work or have difficulty remembering appointments. This cognitive impairment can impact various aspects of daily life.
Diagnosis and Assessment
Pinpointing central pain syndrome (CPS) can be a challenging journey, often requiring a multi-faceted approach. A thorough understanding of the patient’s medical history, combined with meticulous neurological examinations, imaging studies, and psychological assessments, is crucial for accurate diagnosis. This process aims to identify the underlying neurological dysfunction contributing to the patient’s pain experience and its impact on their overall well-being.Accurate diagnosis of CPS hinges on recognizing the complex interplay between neurological factors, psychological distress, and the patient’s unique experience.
This necessitates a holistic approach that integrates various diagnostic tools and procedures. The process is not just about identifying the pain; it’s about understanding the complete picture of the individual’s condition.
Dealing with central pain syndrome can be tough, but boosting your immune system might help. Taking steps to avoid the flu, like the ones outlined in the viral nurse things you can do to avoid flu , could indirectly improve your overall well-being and potentially lessen pain symptoms. Ultimately, consistent self-care plays a significant role in managing central pain syndrome.
Neurological Examinations
Neurological examinations play a pivotal role in the diagnostic process. These examinations assess reflexes, sensation, motor function, coordination, and balance. Variations from normal findings can suggest the presence of neurological dysfunction, potentially linking to the central pain experience. A comprehensive neurological examination is essential for gathering objective data about the patient’s neurological status.
Imaging Studies
Imaging studies, particularly MRI (magnetic resonance imaging) and PET (positron emission tomography), are valuable tools for evaluating the brain and spinal cord. MRI can provide detailed anatomical images, revealing structural abnormalities or changes in the central nervous system that might correlate with CPS. PET scans, on the other hand, can assess metabolic activity within the brain, potentially highlighting areas of abnormal function.
The information obtained from these imaging techniques can support the diagnosis and guide treatment strategies.
Patient History and Symptom Evaluation
Thorough evaluation of the patient’s medical history and symptom description is fundamental. The patient’s account of pain location, intensity, quality, and duration, along with any associated symptoms, provides valuable insights into the nature and possible origin of the pain. Factors like previous injuries, illnesses, and medications should also be carefully considered. This detailed history contributes significantly to a comprehensive understanding of the individual’s experience and aids in differentiating CPS from other pain conditions.
Psychological Assessments, Pain relief central pain syndrome
Psychological assessments are critical for understanding the emotional and cognitive impact of CPS. These assessments can evaluate factors like anxiety, depression, and coping mechanisms. This helps to understand how the pain affects the patient’s overall well-being and can inform the development of comprehensive treatment plans. Psychological assessments might involve questionnaires, interviews, and other standardized measures to provide valuable data on the patient’s mental health.
Imaging Techniques for Assessing Central Pain
Different imaging techniques provide varied insights into the neurological underpinnings of CPS. These techniques can help in identifying areas of dysfunction or abnormalities that might not be apparent during a physical examination.
| Imaging Technique | Description | Usefulness in CPS diagnosis |
|---|---|---|
| MRI | Magnetic Resonance Imaging uses powerful magnetic fields and radio waves to create detailed images of the body’s internal structures. | MRI can reveal structural abnormalities in the brain and spinal cord, such as lesions, atrophy, or inflammation, which may be associated with CPS. |
| PET | Positron Emission Tomography measures metabolic activity in tissues and organs by detecting the emission of positrons from radioactive tracers. | PET scans can highlight areas of abnormal brain activity, which might correlate with pain processing in CPS. This can help distinguish it from other conditions with similar symptoms. |
Treatment Approaches
Central Pain Syndrome (CPS) requires a multifaceted approach, as no single treatment works for everyone. Effective management often involves a combination of pharmacological interventions and non-pharmacological therapies tailored to the individual’s specific needs and symptoms. This section delves into the various treatment options available, highlighting their potential benefits and limitations.Pharmacological treatments aim to modulate the abnormal pain signals within the central nervous system.
These interventions can significantly impact symptom severity, but their effectiveness varies depending on the individual and the specific type of CPS.
Pharmacological Treatments
Analgesics, including opioids and non-opioids, are often used to manage the pain associated with CPS. Opioids, while potentially effective, carry significant risks of addiction and side effects, and their long-term use is often not recommended. Non-opioid analgesics, such as NSAIDs and acetaminophen, can provide some pain relief but may not be sufficient for severe CPS.Antidepressants, particularly tricyclic antidepressants (TCAs) and selective serotonin and norepinephrine reuptake inhibitors (SNRIs), are frequently prescribed for CPS.
These medications can help regulate the neurotransmitters involved in pain processing, leading to a reduction in pain intensity and associated symptoms. However, the effectiveness of antidepressants in CPS can vary, and some individuals may experience significant side effects.
| Medication | Potential Side Effects |
|---|---|
| Gabapentin | Drowsiness, dizziness, swelling, weight gain, and gastrointestinal problems. Rarely, more serious side effects like allergic reactions or suicidal thoughts can occur. |
| Pregabalin | Drowsiness, dizziness, swelling, and weight gain. Gastrointestinal issues, including nausea and vomiting, are also possible. Rare cases of allergic reactions or suicidal thoughts have been reported. |
| Amitriptyline | Drowsiness, dry mouth, constipation, blurred vision, and difficulty urinating. Orthostatic hypotension (a sudden drop in blood pressure upon standing) is also a possible side effect. |
| Venlafaxine | Nausea, vomiting, diarrhea, insomnia, dizziness, and sexual dysfunction. Increased blood pressure and heart rate are also possible. |
Non-Pharmacological Therapies
Non-pharmacological approaches play a crucial role in the comprehensive management of CPS. These therapies can complement pharmacological interventions and address the psychological and physical aspects of the condition.Physical therapy is often essential for improving mobility, strength, and flexibility. Physical therapists can develop customized exercise programs and strategies to enhance functional capacity and reduce pain. Cognitive behavioral therapy (CBT) can help individuals cope with the emotional and psychological distress associated with chronic pain.
CBT equips patients with coping mechanisms to manage their pain and improve their overall well-being. Alternative therapies, such as acupuncture, massage therapy, and mindfulness-based practices, are sometimes used to alleviate pain and promote relaxation. While evidence supporting the effectiveness of some alternative therapies is limited, they can be beneficial adjuncts to other treatment modalities.
Multidisciplinary Approach
Managing CPS requires a multidisciplinary team approach. A team comprising physicians, pain specialists, physical therapists, psychologists, and other healthcare professionals can provide a comprehensive and coordinated plan of care. This collaborative effort ensures that all aspects of the condition are addressed and that the patient receives the most appropriate and effective interventions. The team can tailor the treatment plan based on the patient’s specific needs and symptoms, allowing for more personalized care.
Impact on Daily Life

Living with central pain syndrome (CPS) significantly impacts daily life, often creating challenges in various aspects of an individual’s routine and well-being. The chronic and often unpredictable nature of pain, coupled with associated symptoms, can profoundly affect work, relationships, and leisure activities. This section delves into the multifaceted ways CPS influences daily life, illustrating the impact on sleep, emotional regulation, and concentration.The pervasive nature of CPS can hinder an individual’s ability to perform everyday tasks and engage in activities they once enjoyed.
This impact extends beyond the immediate physical discomfort, encompassing the emotional and psychological consequences of living with a chronic condition. The ensuing frustration, fatigue, and isolation can contribute to a diminished quality of life.
Impact on Daily Activities
The persistent pain and accompanying symptoms associated with CPS can disrupt nearly every aspect of daily life. Simple tasks that most people take for granted, such as walking, dressing, or even engaging in light household chores, can become significant hurdles. This often leads to limitations in activities, which can severely restrict opportunities for social interaction and personal growth.For instance, an individual with CPS might find it challenging to maintain a job due to fluctuating pain levels and the inability to concentrate.
Relationships can also be strained as the individual struggles to participate in social events or fulfill their usual responsibilities. Leisure activities, like hobbies or sports, become difficult or even impossible to pursue due to the constant pain and fatigue.
Dealing with central pain syndrome can be tough, especially for kids. It’s a complex condition, but understanding how parents can help anxious children confront their fears might offer valuable insights. Learning strategies from resources like how parents can help anxious kids face their fears could translate into helpful techniques for managing the pain and anxiety associated with central pain syndrome.
Ultimately, finding the right approach to pain relief is key.
Impact on Social Interactions
Social interactions are frequently affected by CPS. The unpredictability of pain episodes and the potential for flare-ups can make it difficult to maintain social commitments. Individuals may avoid social gatherings or activities, fearing that they will be unable to cope with the pain or discomfort. This isolation can have a negative impact on mental health, leading to feelings of loneliness and depression.Moreover, the emotional toll of CPS can also affect social interactions.
The chronic pain and fatigue can lead to irritability, frustration, and a decreased ability to regulate emotions. This can strain relationships with family members and friends. Difficulties in expressing emotions and communicating needs can further exacerbate social isolation.
Impact on Work and Leisure
The impact of CPS on work can be substantial. Fluctuations in pain levels, fatigue, and difficulty concentrating can make it challenging to maintain productivity and focus. Many individuals with CPS find it difficult to hold down a job, leading to financial strain and further emotional distress. Similarly, leisure activities are often affected. The pain and fatigue can make it difficult to engage in hobbies, sports, or other enjoyable activities.
Effect on Daily Functioning
This table illustrates the effect of CPS on sleep patterns, emotional regulation, and concentration.
| Area Affected | Impact of CPS |
|---|---|
| Sleep | CPS can disrupt sleep patterns due to pain, fatigue, and discomfort. This can lead to insomnia, restless sleep, and daytime fatigue, further impacting daily activities. |
| Emotional Regulation | CPS can cause significant emotional distress, including anxiety, depression, irritability, and frustration. These emotional challenges can further complicate social interactions and daily life. |
| Concentration | Chronic pain and associated symptoms can make it difficult to concentrate and focus on tasks. This can impact work performance, academic success, and overall cognitive function. |
Visual Representation of Challenges
Imagine a series of interconnected gears, each representing a facet of daily life (work, relationships, leisure). Each gear is affected by a central, malfunctioning gear representing CPS. As the central gear malfunctions, the interconnected gears slow down, become misaligned, and eventually grind to a halt. This visual metaphor demonstrates how CPS can disrupt multiple aspects of daily life, impacting work, relationships, and personal well-being.
Research and Future Directions
Unraveling the complexities of central pain syndrome (CPS) requires a multi-faceted approach, encompassing both fundamental research into the underlying mechanisms and targeted clinical trials to refine treatment strategies. Current research efforts are focused on identifying specific biomarkers and pathways involved in CPS, which will pave the way for more accurate diagnostic tools and personalized treatments. Furthermore, ongoing studies are exploring the effectiveness of novel therapeutic interventions, offering hope for improved pain management and quality of life for those affected by CPS.
Current Research Efforts
Research into CPS is actively exploring the neural pathways and brain regions involved in the development and maintenance of chronic pain. Scientists are investigating the role of neurotransmitters, such as glutamate and substance P, in modulating pain signals within the central nervous system. These studies aim to shed light on the specific mechanisms that contribute to the persistent and often debilitating nature of CPS.
Researchers are also examining the impact of genetic factors and environmental triggers on the development of CPS. This multifaceted approach promises to enhance our understanding of the condition and potentially lead to targeted interventions.
Areas for Further Research
Improving diagnostic tools for CPS remains a crucial area of research. Currently, diagnosing CPS often relies on a combination of clinical assessment and exclusion of other conditions. Further research is needed to develop objective and reliable diagnostic markers, such as specific imaging techniques or blood tests. Developing more precise diagnostic tools will enable earlier and more accurate identification of CPS, leading to timely interventions and potentially better outcomes.
Furthermore, a deeper understanding of the heterogeneity of CPS presentations is critical. Individual variations in symptom profiles and underlying mechanisms could be responsible for the diverse responses to existing therapies. Research focusing on identifying subgroups within CPS based on specific characteristics may reveal unique treatment targets and enhance treatment efficacy.
Promising New Therapies
Several promising new therapies are being investigated for pain relief in CPS. These include non-invasive brain stimulation techniques, such as transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS). These methods aim to modulate neural activity in pain-processing regions of the brain, potentially reducing pain intensity and improving functional outcomes. Furthermore, novel pharmacological approaches targeting specific neurotransmitter systems are being explored.
Research is investigating drugs that can modulate the activity of pain pathways within the brain, potentially offering new avenues for pain management.
Ongoing Clinical Trials
Several clinical trials are underway to evaluate the efficacy and safety of various treatment approaches for CPS. These trials often involve small patient populations, and the results are often preliminary. However, these studies offer valuable insights into the potential benefits and limitations of different therapies. For example, one trial might be investigating the effectiveness of a new type of medication in managing specific CPS symptoms.
Another trial could be assessing the impact of a specific type of brain stimulation on pain intensity and functional capacity in CPS patients. Detailed data from these trials will help researchers understand the best course of treatment for individual patients with CPS.
Last Word: Pain Relief Central Pain Syndrome
In conclusion, central pain syndrome presents a significant challenge in terms of pain management, requiring a multidisciplinary approach that addresses both the physical and psychological aspects of the condition. While significant progress has been made in understanding and treating CPS, further research and development of innovative therapies are crucial for improving the lives of those affected. Ultimately, a compassionate and individualized approach to care is paramount in ensuring the best possible outcomes for individuals living with this challenging syndrome.