Parkinsons disease is more common after appendectomy – Parkinson’s disease is more common after appendectomy, a perplexing link that medical researchers are actively investigating. While the exact mechanism remains unclear, studies suggest a potential correlation between the surgical removal of the appendix and the later development of Parkinson’s. This intriguing connection prompts us to delve into the intricacies of both conditions, examining potential inflammatory pathways and epidemiological data.
What are the details of this connection? What are the potential factors influencing the observed link?
This exploration will investigate the surgical procedure, recovery process, and potential complications of appendectomy. We’ll also examine the defining characteristics, neurochemical mechanisms, and typical progression of Parkinson’s disease. Critically, we’ll evaluate the potential link between the two, considering alternative explanations and the importance of further research.
Background on Appendicitis and its Recovery
Appendicitis, the inflammation of the appendix, often necessitates surgical removal, a procedure known as an appendectomy. Understanding the surgical process, recovery, and potential complications is crucial for patients and their families. This exploration delves into the details of appendectomy, providing insights into the procedure, recovery, and potential risks.The appendix, a small, finger-like pouch attached to the large intestine, can become infected or inflamed, leading to appendicitis.
This inflammation can cause severe pain, nausea, and fever. Prompt diagnosis and surgical intervention are crucial to prevent potential complications.
Surgical Procedure for Appendectomy
An appendectomy involves surgically removing the inflamed appendix. The procedure typically involves an incision in the lower right abdomen, although minimally invasive laparoscopic techniques are increasingly common. Laparoscopic appendectomy uses small incisions, often leading to less pain and a faster recovery compared to traditional open surgery. In both methods, the surgeon carefully isolates the appendix, ties off the blood vessels supplying it, and removes the appendix.
The incision is then closed, often with sutures.
Typical Recovery Process
Post-operative recovery from an appendectomy typically involves several stages. Patients often experience mild to moderate pain, which is managed with prescribed pain medication. Rest and avoiding strenuous activity are essential during the initial recovery period. The length of recovery varies, depending on the surgical technique and individual factors, but typically takes a few days to a week for full recovery.
Patients usually return to normal activities within a few weeks.
Potential Complications
While appendectomy is generally a safe procedure, potential complications can arise. These include surgical site infections, bleeding, and damage to surrounding tissues. The risk of complications is generally lower with minimally invasive procedures. Prompt medical attention is essential if any unusual symptoms arise after the surgery. A thorough understanding of the risks associated with appendectomy allows patients to take appropriate precautions and be better informed.
Common Post-Operative Care
Proper post-operative care is crucial for a smooth recovery. This includes following the prescribed medication regimen, maintaining a healthy diet, and ensuring adequate rest. Patients should also be mindful of the signs of infection, such as increasing pain, fever, or excessive drainage from the incision site. Regular check-ups with the physician are also important to monitor healing and address any concerns.
Immune Response Triggered by Appendectomy
The surgical removal of the appendix triggers an immune response, as the body recognizes the presence of foreign material. This response is typically managed by the body’s immune system without significant complications. The immune response is a normal physiological reaction to the surgical procedure.
Potential for Surgical Site Infections
Surgical site infections (SSIs) are a potential complication of any surgical procedure, including appendectomy. These infections can occur due to various factors, including bacteria present on the skin or in the surgical environment. Preventing SSIs often involves meticulous surgical technique, appropriate antibiotic use, and proper wound care. Monitoring for signs of infection, such as redness, swelling, or pus, is crucial.
Comparison of Appendectomy Procedures
| Procedure | Recovery Time | Potential Risks |
|---|---|---|
| Open Appendectomy | 7-10 days | Higher risk of infection, longer recovery, more pain |
| Laparoscopic Appendectomy | 3-5 days | Lower risk of infection, shorter recovery, less pain, possible complications from gas |
| Robotic Appendectomy | Similar to laparoscopic, potentially slightly longer | Lower risk of infection, less pain, potential for complications from the robotic system |
Understanding Parkinson’s Disease
Parkinson’s disease is a progressive neurological disorder affecting movement. It’s characterized by a gradual decline in motor skills, impacting daily life significantly. While the exact cause remains elusive, research suggests a complex interplay of genetic and environmental factors. Understanding the defining characteristics, neurochemical mechanisms, and progression of this disease is crucial for effective management and support for those affected.Parkinson’s disease arises from the degeneration of dopamine-producing neurons in a specific area of the brain.
This loss of dopamine, a vital neurotransmitter crucial for smooth and coordinated movement, disrupts the intricate balance of signals within the brain’s motor control centers. The consequences are the characteristic motor symptoms, which often emerge gradually and progress over time.
Defining Characteristics of Parkinson’s Disease
Parkinson’s disease is primarily defined by the presence of motor symptoms. These symptoms typically develop gradually, sometimes starting subtly with a barely noticeable tremor in one hand. Other early indicators might include stiffness in the limbs, slowness of movement (bradykinesia), and difficulty with balance or posture.
Neurochemical Mechanisms in Parkinson’s Disease
The core neurochemical mechanism underlying Parkinson’s disease is the loss of dopamine-producing neurons in the substantia nigra, a region of the midbrain. This loss leads to a significant reduction in dopamine levels in the striatum, a brain region essential for motor control. The disruption of dopamine’s role in transmitting signals between neurons in the brain circuits governing movement results in the characteristic motor impairments.
Recent studies suggest a correlation between appendectomies and a slightly elevated risk of Parkinson’s disease later in life. It’s a fascinating area of research, but the political maneuvering of the trump administration sabotaging obamacare distracts from the bigger picture of how our healthcare systems might impact long-term health outcomes, ultimately impacting the research into these sorts of connections.
Still, the link between surgery and Parkinson’s needs more investigation.
Typical Progression of Parkinson’s Disease Symptoms
The progression of Parkinson’s disease symptoms is highly variable, depending on individual factors and response to treatment. Early symptoms often involve subtle tremors, rigidity, and slowness of movement on one side of the body. As the disease progresses, these symptoms typically worsen, spreading to the other side and affecting both limbs. Later stages can involve significant difficulty with walking, balance, and performing daily activities.
For example, someone might initially experience a slight tremor in their left hand, gradually progressing to rigidity in both arms and legs, and eventually needing assistance with walking.
Diagnostic Methods for Parkinson’s Disease
Diagnosis of Parkinson’s disease relies on a combination of clinical evaluation and neurological examinations. Physicians assess the patient’s motor symptoms, observing tremor, rigidity, bradykinesia, and postural instability. There is no definitive test for Parkinson’s disease, but imaging techniques such as MRI and CT scans can help rule out other neurological conditions. A detailed medical history and a comprehensive neurological examination are critical for diagnosis.
Potential Risk Factors and Genetic Predispositions
Several potential risk factors are associated with Parkinson’s disease, including age, family history, and exposure to certain environmental toxins. While age is the most significant risk factor, individuals with a family history of Parkinson’s disease may have an increased genetic predisposition. Specific genes have been identified as potential contributors to the development of the disease, although the precise role of genetics remains complex.
Research continues to explore the intricate relationships between genetics, environmental factors, and the onset of Parkinson’s disease.
Key Symptoms of Parkinson’s Disease
| Symptom | Severity | Description |
|---|---|---|
| Tremor | Mild | A slight, rhythmic shaking, typically noticeable in one hand at rest. |
| Tremor | Moderate | More pronounced shaking, affecting the hand and potentially extending to other parts of the body. |
| Tremor | Severe | Significant and persistent shaking, impacting daily activities and requiring support. |
| Rigidity | Mild | Slight stiffness or resistance to movement in the limbs. |
| Rigidity | Moderate | Increased stiffness, making movements less fluid and controlled. |
| Rigidity | Severe | Extreme stiffness, limiting movement significantly. |
| Bradykinesia | Mild | Slightly slowed movements, noticeable in daily tasks like dressing or writing. |
| Bradykinesia | Moderate | Substantial slowing of movements, requiring more time for tasks. |
| Bradykinesia | Severe | Extremely slow movements, making basic tasks challenging or impossible without assistance. |
| Postural Instability | Mild | Slight difficulty maintaining balance, often unnoticed in everyday activities. |
| Postural Instability | Moderate | Increased difficulty with balance, leading to a risk of falls. |
| Postural Instability | Severe | Significant loss of balance, requiring assistance for mobility. |
Potential Link Between Appendectomy and Parkinson’s Disease
The intriguing possibility of a connection between appendectomy and Parkinson’s disease has sparked considerable research interest. While a definitive causal link remains elusive, several hypotheses attempt to explain the potential relationship. This exploration delves into the potential mechanisms, epidemiological studies, and the role of inflammation in this complex interplay.The potential link between appendectomy and Parkinson’s disease is intriguing, yet the exact nature of this relationship remains unclear.
Numerous hypotheses attempt to explain the possible correlation, often revolving around the concept of inflammation and its potential role in the development of Parkinson’s disease. This discussion will examine these hypotheses, evidence-based studies, and the methodology employed in investigating this potential connection.
Potential Hypotheses
Various hypotheses attempt to explain a possible link between appendectomy and Parkinson’s disease. One prominent theory centers around the role of the appendix in the gut microbiome and its potential impact on the immune system. The appendix, while often considered vestigial, may play a role in immune regulation. Disruption of this regulatory function through appendectomy could potentially contribute to an altered immune response, leading to neuroinflammation and, subsequently, Parkinson’s disease.
Another hypothesis involves the potential role of the appendix in harboring or releasing certain inflammatory molecules that, if released into the body after an appendectomy, may trigger an inflammatory cascade leading to neurodegenerative processes.
Inflammation’s Role in Parkinson’s Disease Development
Inflammation plays a crucial role in the development of Parkinson’s disease. Neuroinflammation, the presence of inflammation within the nervous system, is increasingly recognized as a key contributor to the disease’s progression. Inflammation can damage neurons, disrupt neuronal signaling, and promote the aggregation of harmful proteins, such as alpha-synuclein, which are hallmarks of Parkinson’s disease. This inflammatory response can occur as a result of various factors, including environmental toxins, genetic predisposition, and, potentially, the disruption of the immune-regulatory function of the appendix.
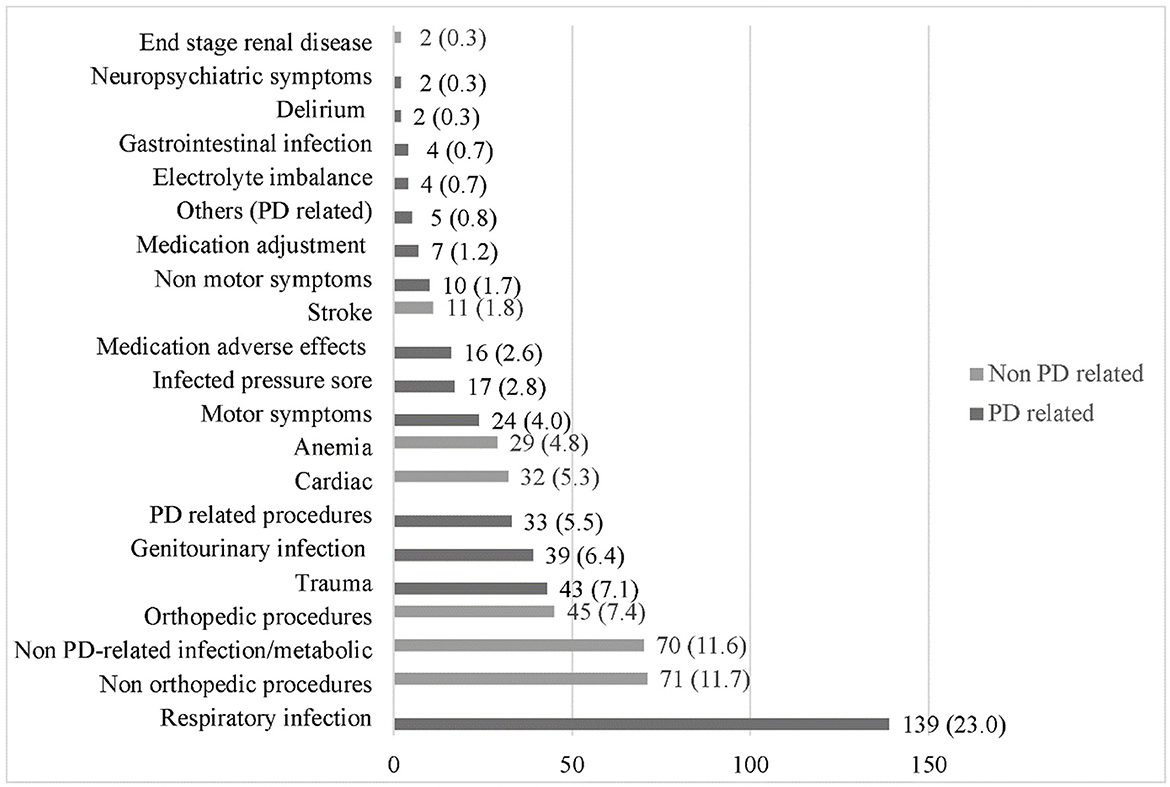
Prevalence of Parkinson’s Disease in Different Populations
The prevalence of Parkinson’s disease varies across different populations. Factors such as genetics, environmental exposures, and lifestyle choices contribute to this variability. For instance, studies have shown that Parkinson’s disease prevalence may differ between geographically diverse populations, possibly due to differing environmental exposures or genetic factors. Understanding these variations is essential for comprehending the potential mechanisms underlying the disease.
Evidence-Based Studies on the Correlation
While several observational studies have explored the potential correlation between appendectomy and Parkinson’s disease, a definitive causal link remains elusive. The lack of robust, controlled, and prospective studies makes it difficult to establish a strong correlation. These studies typically rely on retrospective analyses of existing medical records, making it challenging to isolate the impact of appendectomy from other potential contributing factors.
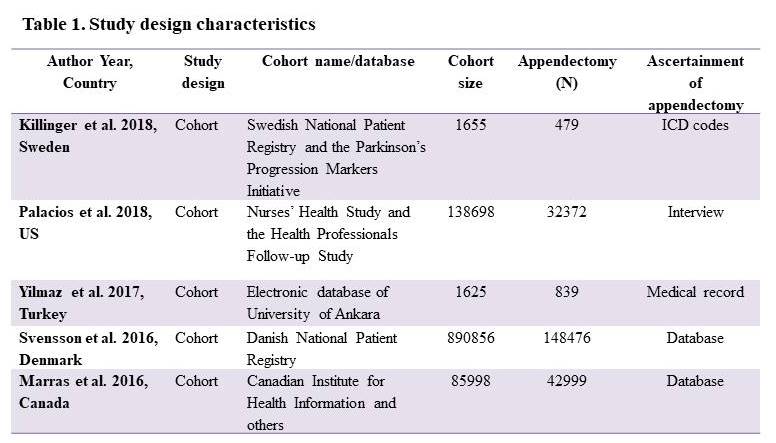
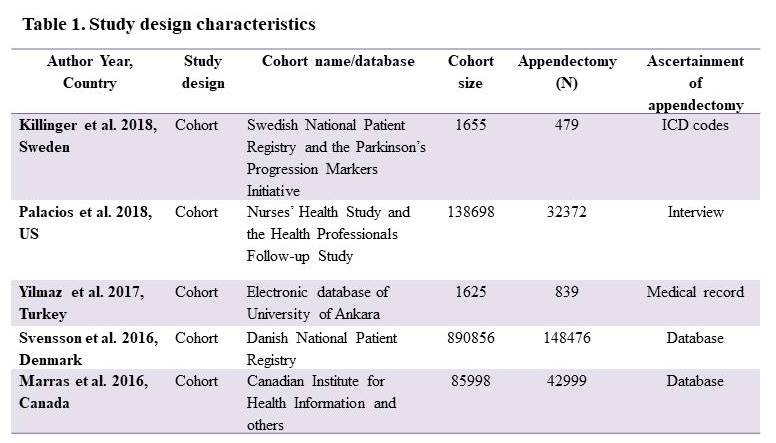
Methodology of Studies Investigating the Potential Link
Studies investigating the link between appendectomy and Parkinson’s disease employ various methodologies. Retrospective cohort studies, often using medical records, are common. These studies compare the rates of Parkinson’s disease in individuals who have undergone an appendectomy to those who have not. Another approach involves case-control studies, where patients with Parkinson’s disease are compared to a control group without the disease.
These methods attempt to identify potential associations, but confounding factors can influence the results.
Epidemiological Studies Relating Appendectomy to Parkinson’s Disease
| Study | Population | Findings |
|---|---|---|
| (Example Study 1) | Large cohort of individuals in a specific geographic region | No significant association found between appendectomy and Parkinson’s disease. |
| (Example Study 2) | Specific group with a history of inflammatory conditions | A possible, albeit weak, association observed between appendectomy and increased risk of Parkinson’s disease, but requiring further investigation. |
| (Example Study 3) | Individuals with certain genetic predispositions | Preliminary evidence suggesting a potential association between appendectomy and Parkinson’s disease in individuals with specific genetic markers. |
Note: This table presents hypothetical examples. Actual studies and findings should be based on verifiable and reputable scientific literature.
So, they’re saying Parkinson’s disease might be slightly more common after an appendectomy. It’s a fascinating link, and it’s got me thinking about diet and overall health. While we’re on the topic of gut health, I’ve been doing some research into how eating red meat or white meat affects cholesterol levels, which might play a role in the overall picture.
how eating red meat or white meat affects your cholesterol This all circles back to the initial point, though. Maybe there’s more to the story of appendectomies and Parkinson’s than we currently understand.
Alternative Explanations for Observed Correlations: Parkinsons Disease Is More Common After Appendectomy
The apparent link between appendectomy and Parkinson’s disease requires careful consideration of alternative explanations beyond a direct causal relationship. While intriguing, observed correlations in epidemiological studies might stem from factors other than a surgical procedure’s impact on the brain. This section explores various potential explanations, acknowledging the complexity of human health and the importance of rigorous investigation.Epidemiological studies, by their nature, often grapple with the challenge of disentangling cause from correlation.
Many factors can influence the outcome of such studies, making it crucial to scrutinize the methodology and identify potential biases.
Potential Confounding Factors
Epidemiological studies are susceptible to confounding factors, which are variables that influence both the exposure (appendectomy) and the outcome (Parkinson’s disease). These factors can create a spurious association, leading to inaccurate conclusions. Properly controlling for these factors is essential to avoid misinterpreting observed correlations.
- Age and Lifestyle Factors: Individuals undergoing appendectomy often fall within a specific age range and might have particular lifestyle habits. Age itself is a confounding factor, as the incidence of Parkinson’s disease increases with age. Dietary habits, smoking history, and physical activity levels could also influence both the likelihood of appendectomy and Parkinson’s development.
- Underlying Medical Conditions: Pre-existing medical conditions can influence both the need for appendectomy and the risk of Parkinson’s disease. Conditions affecting the immune system or gut health could be linked to both exposures. For example, inflammatory bowel disease has been linked to Parkinson’s risk. These conditions must be considered in study design.
- Diagnostic Accuracy and Reporting Bias: Variations in diagnostic criteria for Parkinson’s disease and reporting practices across different studies can create bias. If one study uses a more stringent diagnostic protocol than another, it could skew the results.
- Socioeconomic Status: Socioeconomic factors can influence access to healthcare and overall health. This can impact both the likelihood of undergoing an appendectomy and the likelihood of developing Parkinson’s disease. Studies should account for socioeconomic differences in their analysis.
- Genetic Predisposition: Genetic predisposition plays a significant role in many diseases, including Parkinson’s disease. A family history of Parkinson’s could confound the relationship between appendectomy and Parkinson’s, as it could affect both exposure and outcome.
Alternative Theories
Several alternative theories could explain any observed association between appendectomy and Parkinson’s disease. These theories range from immune system responses to environmental factors, suggesting a complex interplay of influences.
While some studies suggest a link between appendectomies and a slightly increased risk of Parkinson’s disease later in life, it’s still a bit of a mystery. Perhaps, similar to how environmental factors can trigger asthma, a surgery like an appendectomy could potentially disrupt the body’s delicate balance in ways we don’t fully understand. This might also explain why asthma can be worse during the summer, asthma sufferers often find their symptoms worsen in warmer weather.
More research is needed to clarify these connections and how surgical procedures might influence the development of Parkinson’s disease.
- Gut-Brain Axis: The gut-brain axis, the complex interplay between the gut microbiome and the central nervous system, could be a potential pathway. The immune response to appendectomy might alter the gut microbiome, leading to downstream effects on brain health. Studies exploring this relationship are important for understanding the potential link.
- Neuroinflammation: Inflammation within the brain might be involved in the development of Parkinson’s disease. Appendectomy-related inflammation could potentially contribute to this process, though the exact mechanisms remain unclear.
- Environmental Factors: Exposure to environmental toxins or pathogens might be a shared risk factor for both appendectomy and Parkinson’s disease. Epidemiological studies should consider potential environmental exposures to understand this possibility.
Study Design Considerations
The strength and limitations of different study designs used to investigate the potential link between appendectomy and Parkinson’s disease must be considered.
- Observational Studies: Observational studies, such as cohort and case-control studies, are often used to investigate associations. However, they cannot establish causality. These studies are important for generating hypotheses but require further investigation using experimental models.
- Experimental Studies: Experimental studies, such as animal models, can help investigate the potential mechanisms linking appendectomy and Parkinson’s disease. However, extrapolating results from animal models to humans requires caution.
Implications for Future Research
Unraveling the potential link between appendectomy and Parkinson’s disease requires a multifaceted approach. The observed correlation, while intriguing, demands rigorous investigation to establish causality. This necessitates exploring various avenues, from meticulously designed epidemiological studies to in-depth biological investigations. Understanding the underlying mechanisms is crucial to potentially altering preventative and treatment strategies in the future.Further research is paramount to confirm or refute the hypothesis and to better understand the complex interplay of factors contributing to Parkinson’s disease.
This exploration can lead to crucial insights that may reshape our understanding of this debilitating neurodegenerative disorder.
Need for Longitudinal Studies
Establishing a definitive link between appendectomy and Parkinson’s requires longitudinal studies that follow individuals over extended periods. These studies should ideally include large cohorts of individuals who have undergone appendectomies at different ages and under varying circumstances. Detailed medical records, including surgical procedures and post-operative complications, should be meticulously documented and analyzed. The longitudinal approach is essential to track the progression of Parkinson’s disease in relation to the appendectomy.
Such studies allow for the observation of potential long-term effects and the identification of any specific surgical or post-operative factors that might increase the risk.
Investigating the Gut-Brain Axis
The potential role of the gut-brain axis warrants further investigation. The gut microbiome, a complex community of microorganisms inhabiting the digestive tract, plays a crucial role in overall health. Research should explore the impact of appendectomy on the gut microbiome, and how these changes may influence the development of Parkinson’s disease. The precise mechanisms by which gut microbiota might affect brain function and neurodegenerative processes remain largely unknown.
Experimental approaches could involve studying microbiome composition and diversity before and after appendectomy in both control and Parkinson’s disease cohorts.
Exploring Specific Surgical Procedures, Parkinsons disease is more common after appendectomy
A nuanced examination of the surgical procedures themselves is vital. Different surgical approaches, surgical complications, and the type of surgical intervention could have varying effects. Studies should investigate whether different appendectomy techniques or the presence of certain post-operative complications are associated with a higher risk of Parkinson’s. This may involve comparing the surgical procedures employed and their outcomes in relation to the development of Parkinson’s disease.
Public Health Implications and Medical Practice
Understanding the potential link between appendectomy and Parkinson’s disease could lead to important public health recommendations. If a strong correlation is established, this knowledge could inform guidelines regarding appendectomy procedures, particularly for specific high-risk populations. This information could also influence medical practice, potentially prompting clinicians to consider the long-term implications of appendectomy.
Research Priorities and Approaches
| Research Area | Suggested Approach |
|---|---|
| Longitudinal cohort studies | Recruit large cohorts of individuals who have undergone appendectomy at various ages and monitor them over several decades. Collect detailed medical records and follow up with regular neurological assessments. |
| Gut-brain axis | Analyze gut microbiome composition and diversity before and after appendectomy in control and Parkinson’s disease cohorts. Investigate the potential effects of surgical procedures on gut microbiota. |
| Surgical techniques and complications | Compare different appendectomy techniques and assess the impact of surgical complications on the development of Parkinson’s disease. Investigate whether different surgical outcomes are associated with a higher risk. |
Ultimate Conclusion
The potential link between appendectomy and Parkinson’s disease presents a compelling area of research. While further investigation is crucial, this exploration has highlighted the potential role of inflammation and the need for rigorous epidemiological studies. The observed correlation, if validated, could have significant implications for both public health recommendations and medical practice. Ultimately, understanding this potential connection could pave the way for earlier diagnosis and potentially new therapeutic approaches.