People using opioids for chronic pain shouldnt stop cold turkey – People using opioids for chronic pain shouldn’t stop cold turkey. Sudden cessation can trigger severe withdrawal symptoms, impacting physical and mental well-being. Understanding the risks and exploring alternative, gradual approaches is crucial for managing chronic pain effectively and safely.
This comprehensive guide delves into the dangers of abrupt opioid cessation, outlining alternative pain management strategies, and emphasizing the importance of gradual reduction plans under medical supervision. It also highlights the vital role of healthcare professionals and patient support systems in navigating this challenging process.
Understanding the Risks of Abrupt Cessation
Stopping opioid use abruptly for chronic pain can be extremely dangerous. The body, having become accustomed to the presence of opioids, experiences significant physiological changes when these medications are suddenly withdrawn. This can lead to a cascade of potentially severe and even life-threatening withdrawal symptoms. A gradual, medically supervised tapering strategy is crucial to mitigate these risks.The body’s systems become reliant on opioids, modifying neurochemical pathways and receptor function.
These changes, while often temporary, can be profound. This reliance necessitates a cautious and controlled approach to cessation. Ignoring the potential dangers of abrupt cessation can have devastating consequences for individuals with chronic pain.
Potential Dangers of Abrupt Cessation
Opioid withdrawal is a complex process, marked by a variety of unpleasant symptoms. These symptoms arise as the body attempts to re-establish its normal balance without the presence of opioids. The most significant concern lies in the potential for severe complications if the withdrawal process is not managed appropriately.
Physiological Mechanisms of Opioid Withdrawal
Opioids exert their effects by binding to opioid receptors in the central nervous system. These receptors, primarily mu-opioid receptors, play a crucial role in pain modulation, mood regulation, and other physiological functions. When opioids are chronically used, the body adapts, increasing the expression of opioid receptors or altering the signaling pathways around them. This adjustment leads to a state of dependence.
Abrupt cessation disrupts this altered balance, causing a cascade of neurochemical reactions. The disruption of the delicate equilibrium between neurotransmitters like dopamine, norepinephrine, and serotonin, amongst others, contributes to the emergence of withdrawal symptoms.
“The body’s physiological adaptations to chronic opioid use necessitate a controlled tapering strategy to mitigate the risks of abrupt cessation.”
Examples of Severe Withdrawal Symptoms
Abrupt cessation can trigger a wide range of severe withdrawal symptoms. These symptoms can vary significantly in their intensity and duration, depending on the individual’s tolerance and the amount of opioid used. Examples include seizures, potentially life-threatening cardiovascular issues, and profound psychological distress. The unpredictability of the severity of symptoms highlights the importance of medical supervision.
Severity of Opioid Withdrawal Symptoms
| Symptom | Description | Severity Level |
|---|---|---|
| Nausea and Vomiting | Intense feelings of sickness and repeated episodes of vomiting. | Moderate to Severe |
| Muscle Aches and Pains | Widespread, intense muscle cramps and soreness. | Moderate to Severe |
| Diarrhea | Frequent and watery bowel movements. | Moderate to Severe |
| Anxiety and Irritability | Excessive worry, restlessness, and agitation. | Moderate |
| Insomnia | Inability to sleep or maintain sleep. | Moderate |
| Rhinorrhea (Runny Nose) | Excessive nasal discharge. | Mild |
| Pupil Dilation | Widening of the pupils. | Mild |
| Yawning | Frequent and excessive yawning. | Mild |
Alternative Approaches to Opioid Management
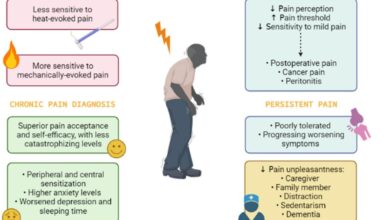
Managing chronic pain without opioids requires a multifaceted approach that considers the individual’s unique needs and preferences. Simply replacing opioids with another medication isn’t always the best strategy; often, a combination of therapies proves most effective. This approach emphasizes holistic well-being, addressing the physical, emotional, and psychological aspects of pain. Effective strategies encompass non-pharmacological interventions and explore the potential of various therapies.Chronic pain often impacts not only physical function but also mental health and overall quality of life.
A comprehensive pain management plan should therefore involve a team of healthcare professionals, including pain specialists, physical therapists, psychologists, and other relevant specialists. This collaborative effort ensures that patients receive the most appropriate and effective care.
Non-Pharmacological Pain Management Techniques
Non-pharmacological methods play a vital role in managing chronic pain without relying on opioids. These techniques often offer long-term benefits and reduce the risk of side effects associated with medication. They include a wide range of approaches, targeting different aspects of the pain experience.
Physical Therapy
Physical therapy interventions are crucial for restoring function and improving mobility. These therapies often involve targeted exercises, manual therapy techniques, and education on proper body mechanics. By strengthening supporting muscles, improving flexibility, and enhancing posture, physical therapy can effectively reduce pain and improve overall physical function. Examples include specific exercises for back pain, strengthening programs for joint pain, and gait training for musculoskeletal disorders.
Cognitive Behavioral Therapy (CBT), People using opioids for chronic pain shouldnt stop cold turkey
Cognitive behavioral therapy (CBT) addresses the psychological aspects of chronic pain. CBT helps patients identify and modify negative thought patterns and behaviors that contribute to pain perception and experience. CBT can be particularly beneficial in reducing pain catastrophizing, increasing coping mechanisms, and improving overall emotional well-being. For example, patients can learn to reframe negative thoughts about their pain, develop relaxation techniques, and manage stress more effectively.
Alternative Medicine Approaches
Alternative medicine approaches, such as acupuncture, massage therapy, and mindfulness-based practices, have shown promise in managing chronic pain. Acupuncture involves inserting thin needles into specific points on the body, believed to stimulate energy flow and reduce pain signals. Massage therapy provides relief through soft tissue manipulation, improving circulation and reducing muscle tension. Mindfulness-based practices, such as meditation and yoga, can help patients focus on the present moment, reducing stress and improving overall well-being.
The efficacy of these approaches often varies from person to person.
Comparison of Non-Opioid Pain Management Options
Different non-opioid pain management techniques offer various benefits and potential risks. Careful consideration of individual needs and preferences is essential in selecting the most appropriate approach. Factors like the type of pain, its severity, and the patient’s overall health status should be considered. The table below provides a concise overview of several non-opioid pain management options.
| Intervention Type | Benefits | Risks | Examples of Specific Interventions |
|---|---|---|---|
| Physical Therapy | Improved mobility, reduced pain, enhanced function | Potential for muscle soreness, discomfort during sessions, limited effectiveness for some conditions | Exercises for back pain, strengthening programs for arthritis, gait training |
| Cognitive Behavioral Therapy (CBT) | Improved coping mechanisms, reduced pain catastrophizing, enhanced emotional well-being | Requires commitment to therapy sessions, potential for emotional distress during sessions, not suitable for everyone | Identifying and modifying negative thoughts, relaxation techniques, stress management |
| Acupuncture | Potential pain relief, reduced inflammation | Risk of bruising, infection at the insertion site, potential allergic reaction to needles | Inserting needles into specific points, stimulating energy flow |
| Massage Therapy | Muscle relaxation, improved circulation, reduced tension | Potential for discomfort, skin irritation, exacerbation of underlying conditions | Soft tissue manipulation, applying pressure and stretching |
| Mindfulness-Based Practices | Stress reduction, improved focus, emotional regulation | Requires consistent practice, potential for initial discomfort, may not be effective for everyone | Meditation, yoga, deep breathing exercises |
Gradual Reduction Strategies
Successfully managing opioid cessation for chronic pain requires a cautious and structured approach. A sudden halt in opioid use can trigger severe withdrawal symptoms, impacting a patient’s well-being and potentially leading to relapse. A gradual reduction strategy, overseen by a healthcare professional, offers a safer alternative, minimizing discomfort and improving long-term outcomes.
Tapering schedules are meticulously designed to gradually decrease opioid dosage over time. This controlled reduction allows the body to adapt, minimizing the intensity of withdrawal symptoms. The schedule itself is tailored to the individual patient’s specific needs, taking into account factors such as the duration and dosage of prior opioid use, overall health status, and potential co-occurring conditions.
Importance of Medical Supervision
Medical supervision is crucial during opioid tapering. Healthcare providers monitor patients closely for any signs of withdrawal, adjust the tapering schedule as needed, and offer supportive care to manage discomfort. They can also address any underlying mental health or physical health concerns that might exacerbate the withdrawal process.
It’s crucial to understand that abruptly stopping opioid use for chronic pain isn’t a healthy approach. Just like a new mom navigating breastfeeding while juggling work and ACA benefits, a gradual approach is key. Finding the right support system and medical guidance is essential, especially when considering the complexities of aca working moms breastfeeding alongside other significant life changes.
A slow, managed withdrawal, overseen by a healthcare professional, is far safer and more effective for managing chronic pain and preventing serious health issues.
Tapering Schedules and Examples
Various tapering schedules are used, and the choice depends on individual patient circumstances. A key aspect of any tapering schedule is the gradual decrease in dosage, which avoids the abrupt cessation of opioid use. The reduction rate and duration of the tapering process are crucial factors to consider.
| Schedule Type | Daily Reduction Rate | Duration | Monitoring Procedures |
|---|---|---|---|
| Slow Taper | 0.5-2.5mg per day reduction in oral morphine equivalents (or equivalent of other opioids) | 4-8 weeks | Daily assessments of vital signs, pain levels, and withdrawal symptoms. Regular follow-up appointments to adjust the schedule as needed. |
| Moderate Taper | 2.5-5mg per day reduction in oral morphine equivalents (or equivalent of other opioids) | 6-12 weeks | Daily assessments of vital signs, pain levels, and withdrawal symptoms. Regular follow-up appointments to adjust the schedule as needed, including medication adjustments for discomfort. |
| Fast Taper | 5-10mg per day reduction in oral morphine equivalents (or equivalent of other opioids) | 8-16 weeks | Daily assessments of vital signs, pain levels, and withdrawal symptoms. Close monitoring for signs of discomfort or complications. Potential for increased frequency of follow-up appointments. |
Note: These are example schedules, and specific details will vary depending on the individual patient’s needs. The exact daily reduction rate and duration should be determined by a healthcare provider.
Patient Monitoring During Tapering
Throughout the tapering process, diligent patient monitoring is essential. Healthcare providers closely track vital signs, assess pain levels, and monitor for withdrawal symptoms. Regular communication between the patient and provider is critical for adjusting the tapering schedule and addressing any emerging concerns. This proactive approach helps to ensure a safe and effective transition off opioids.
The Role of Healthcare Professionals
Navigating the complexities of opioid use disorder requires a collaborative approach, with healthcare professionals playing a pivotal role in guiding patients toward safe and effective pain management strategies. The journey of transitioning off opioids is often fraught with emotional and physical challenges, making the support and expertise of dedicated healthcare providers essential. A compassionate and comprehensive approach is critical to ensure successful outcomes for patients experiencing chronic pain.Healthcare professionals are not merely prescribers of medications; they are essential guides and advocates for their patients.
Their role extends beyond dispensing prescriptions to encompass thorough assessments, personalized treatment plans, and ongoing support throughout the transition process. Open communication, a cornerstone of effective care, empowers patients to actively participate in their recovery journey.
Open Communication and Shared Decision-Making
Open and honest communication between patients and healthcare providers is paramount in opioid management. Patients should feel comfortable discussing their pain experiences, concerns, and expectations regarding treatment options. This dialogue fosters a shared understanding of the patient’s individual needs and preferences, allowing for the development of personalized treatment plans. Healthcare providers should actively listen to patients, address their questions, and provide clear and concise information about the risks and benefits of different strategies.
A collaborative approach, where both parties actively participate in decision-making, is key to successful outcomes.
Comprehensive Pain Assessments and Individualized Treatment Plans
Comprehensive pain assessments are crucial for effective opioid management. These assessments should consider not only the physical symptoms but also the emotional, psychological, and social factors contributing to a patient’s pain experience. This holistic approach allows healthcare professionals to develop individualized treatment plans that address the unique needs of each patient. The treatment plan should include strategies beyond medication, such as physical therapy, counseling, and alternative pain management techniques.
It’s crucial to understand that people using opioids for chronic pain shouldn’t abruptly stop the medication. A gradual reduction, under medical supervision, is vital. In fact, exploring complementary therapies like massage can significantly boost the effectiveness of managing chronic pain alongside medication. For example, massage can boost effectiveness of workouts , and this same principle can apply to pain management.
This gentle approach helps to avoid potentially dangerous withdrawal symptoms and allows for a smoother transition to alternative pain relief methods, ensuring a healthier path forward for those struggling with chronic pain.
Tailoring interventions to the specific circumstances of each patient optimizes the chances of a successful transition.
It’s crucial to understand that abruptly stopping opioid use for chronic pain can be incredibly dangerous. Think about how your body adjusts to long-term medication. Just like prediabetes can develop into type 2 diabetes if not managed properly, gradual adjustments to medication regimens are key for avoiding severe withdrawal symptoms. A slow and monitored tapering process is essential for both physical and mental well-being, and avoiding potentially life-threatening consequences.
Ongoing Support and Counseling
The transition off opioids often necessitates ongoing support and counseling. Patients may experience withdrawal symptoms, emotional distress, and challenges in adapting to new pain management strategies. Counseling can help patients cope with these difficulties, develop healthy coping mechanisms, and build resilience. This ongoing support provides a safety net during a potentially challenging period. It is essential to recognize that patients may require different levels of support and to adapt the approach accordingly.
Comprehensive Pain Management Plan: A Step-by-Step Guide
| Assessment | Treatment Plan | Monitoring | Follow-up |
|---|---|---|---|
| Thorough evaluation of pain history, physical examination, psychological and social factors, medication history. | Development of a personalized treatment plan including medication tapering schedule, non-pharmacological interventions (e.g., physical therapy, exercise, mindfulness), and counseling. | Regular monitoring of pain levels, potential withdrawal symptoms, and adherence to the treatment plan. | Scheduled follow-up appointments to adjust the treatment plan as needed, address any concerns, and provide ongoing support. |
| Identification of potential co-occurring conditions (e.g., anxiety, depression) | Referral to mental health specialists as needed to address any co-occurring conditions and to provide emotional support. | Regular monitoring of mood and psychological well-being. | Ongoing communication with mental health specialists to ensure coordinated care. |
| Assessment of patient’s support system and social environment. | Incorporation of support systems into the treatment plan, such as family members or support groups. | Monitoring of patient’s social support network and identifying any potential challenges. | Referral to social workers or community resources as needed. |
Patient Education and Support Systems

Empowering patients with knowledge and resources is crucial for successful opioid tapering and long-term pain management. A comprehensive approach that goes beyond simply prescribing medication must include education, support, and access to various resources. This involves not only understanding the risks of abrupt cessation but also the benefits of different pain management strategies and the importance of ongoing support.A strong patient education program fosters informed decision-making and promotes adherence to the tapering plan.
It also equips patients with coping mechanisms to navigate the challenges of withdrawal symptoms and emotional distress. This empowers them to actively participate in their recovery journey.
Importance of Educating Patients
Patients need a thorough understanding of the potential benefits and drawbacks of different pain management approaches. This includes not just opioids but also non-pharmacological options such as physical therapy, cognitive behavioral therapy, and alternative therapies. Providing clear, accessible information helps patients make informed choices about their treatment.
Providing Resources and Support Systems
The tapering process can be emotionally and physically challenging. Offering resources and support systems during this period is essential. This includes access to healthcare professionals, support groups, and mental health services. Comprehensive support systems address the whole person, not just the physical symptoms of withdrawal.
Designing Educational Materials
Educational materials should be tailored to the specific needs and literacy levels of the patients. Clear and concise language, along with visuals like charts and diagrams, can significantly improve comprehension. Consider using various formats like pamphlets, videos, or online resources. For example, a video demonstrating relaxation techniques alongside written instructions can reinforce learning and provide actionable steps.
Role of Support Groups and Family Involvement
Support groups provide a safe space for patients to share experiences, gain encouragement, and learn coping strategies from others facing similar challenges. Family involvement is also crucial. Educating family members about the tapering process and its challenges helps them provide effective support and understanding. A supportive family environment can significantly reduce stress and anxiety during the transition.
Family members can be a vital part of the patient’s recovery team.
Examples of Support Resources
- Pain Management Clinics: These clinics often offer comprehensive care, including pain management education, therapy options, and support groups.
- Support Groups (e.g., Narcotics Anonymous): These groups offer peer support and guidance from individuals who have experienced similar struggles.
- Mental Health Professionals: Counselors and therapists can provide emotional support and coping strategies to address the psychological aspects of withdrawal and recovery.
- Online Forums and Communities: Online platforms dedicated to chronic pain or opioid use disorder can offer a supportive environment for connecting with others.
- Patient Advocacy Organizations: These organizations often provide educational materials, support networks, and advocacy for patients’ rights and needs.
Conclusive Thoughts: People Using Opioids For Chronic Pain Shouldnt Stop Cold Turkey

Ultimately, managing chronic pain with opioids requires a careful, phased approach. Abrupt cessation is risky and often ineffective. By understanding the potential dangers, exploring non-opioid options, and embracing gradual reduction strategies under medical guidance, individuals can navigate opioid cessation safely and effectively. This holistic approach prioritizes patient well-being and ensures a path toward improved pain management.