PrEP implementation is associated with a rapid decline in new HIV infections, a significant development with profound implications for global health. This insightful exploration delves into the details of PrEP, examining its various methods of administration, the demographics it benefits, and the associated adherence challenges. We’ll also analyze the correlation between PrEP and declining HIV transmission rates, highlighting the effectiveness of PrEP in reducing new infections.
Furthermore, this analysis considers the factors influencing successful PrEP implementation, including community engagement, healthcare access, and the crucial role of education and awareness.
The impact of PrEP extends beyond immediate infection reduction. We’ll explore the challenges and considerations surrounding PrEP implementation, from logistical hurdles to ethical concerns and the need for equitable access. Real-world examples of successful PrEP programs will be showcased, providing valuable insights into best practices and lessons learned. Finally, we’ll look ahead to the future directions of PrEP research, emphasizing the need for more comprehensive data and innovative strategies to further improve PrEP access and affordability.
Understanding PrEP Implementation
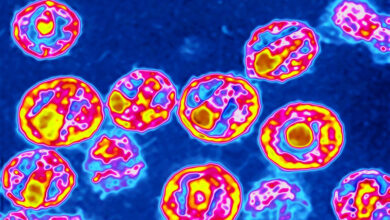
PrEP, or pre-exposure prophylaxis, is a powerful tool in the fight against HIV. It’s a strategy that aims to prevent HIV infection by taking medication before potential exposure. This approach is particularly effective for individuals at high risk of acquiring HIV, and its implementation has contributed to a significant reduction in new HIV infections. This detailed look at PrEP will cover its mechanisms, methods, demographics, and considerations for effective use.PrEP works by preventing HIV from establishing itself in the body.
It does this by blocking the virus’s ability to replicate and integrate into the cells of the immune system. Essentially, PrEP creates a barrier against HIV infection. This approach has proven to be a crucial element in the global effort to reduce HIV transmission.
PrEP Mechanism of Action
PrEP works by inhibiting the entry of HIV into cells. This crucial step prevents the virus from replicating and spreading. This action effectively stops the virus from establishing a foothold in the body.
Methods of PrEP Administration
PrEP is typically administered in the form of a daily pill containing antiretroviral medication. The most common type of PrEP is tenofovir disoproxil fumarate/emtricitabine (Truvada). This medication is taken orally, meaning it’s swallowed with water. Consistent daily intake is essential for maximum effectiveness.
Demographic Groups Benefiting from PrEP
PrEP is beneficial for individuals who are at an increased risk of contracting HIV. This includes men who have sex with men (MSM), people who inject drugs (PWID), and heterosexual individuals in communities with high HIV prevalence. Also, those who have had a history of sexually transmitted infections (STIs) or multiple partners are also prime candidates for PrEP.
PrEP Regimens and Adherence Challenges
| Regimen Type | Medication | Adherence Challenges |
|---|---|---|
| Truvada | Tenofovir disoproxil fumarate/emtricitabine | Potential side effects like nausea, headache, and fatigue can impact adherence. Also, daily pill-taking can be challenging for some. |
| Descovy | Tenofovir alafenamide | While generally well-tolerated, some individuals may experience gastrointestinal upset, impacting adherence. The need for strict adherence is essential for effectiveness. |
Consistent daily intake is crucial for the efficacy of PrEP. Adherence difficulties are a key concern in PrEP implementation, and various strategies exist to support adherence.
Potential Side Effects of PrEP
Potential side effects of PrEP, while generally mild, include nausea, headache, diarrhea, and fatigue. These side effects typically subside over time as the body adjusts to the medication. If side effects are severe or persistent, it is crucial to consult a healthcare provider.
Importance of Ongoing Monitoring for PrEP Users
Regular monitoring is essential for PrEP users. This involves routine HIV testing, including blood tests to assess kidney and liver function, as these organs can be affected by PrEP. Also, regular check-ups with a healthcare provider are critical for ongoing management. This proactive approach helps ensure the safety and effectiveness of PrEP.
The Correlation Between PrEP and HIV Infections

PrEP, or pre-exposure prophylaxis, has emerged as a powerful tool in the fight against HIV. Its successful implementation in various communities has demonstrably led to a significant reduction in new HIV infections. Understanding the factors driving this decline and the potential impact on broader transmission rates is crucial for optimizing public health strategies.PrEP’s effectiveness lies in its ability to prevent HIV transmission by blocking the virus from replicating in the body.
By making it harder for the virus to establish itself, PrEP acts as a significant barrier to infection, particularly when taken consistently. This, in turn, has a profound effect on the overall prevalence of HIV in affected populations. The key to understanding this correlation lies in analyzing the specific factors contributing to the decline in new infections.
Key Factors Contributing to the Decline in New HIV Infections
Consistent use of PrEP is a crucial factor in reducing transmission rates. When individuals at risk consistently take PrEP, the risk of contracting HIV is dramatically reduced. Other factors include targeted outreach and education programs, particularly in communities most affected by HIV. These programs empower individuals with the knowledge and tools to make informed decisions about their health and reduce their risk of exposure.
Studies show that implementing pre-exposure prophylaxis (PrEP) is strongly linked to a dramatic drop in new HIV infections. It’s a testament to the power of preventative measures, and a stark contrast to stories like Randy Travis’s long journey back to health, Randy Travis’s long road back. While his personal struggle highlights the challenges of health recovery, PrEP’s effectiveness underscores the importance of proactive strategies in curbing the spread of HIV.
Potential Impact of PrEP on Overall HIV Transmission Rates
PrEP has the potential to significantly alter the trajectory of HIV transmission. By reducing the number of people who become infected, the overall transmission rate decreases. This reduction in transmission can lead to a decline in the number of people living with HIV, consequently impacting the burden of the disease on healthcare systems and communities. The impact is particularly pronounced in populations with high HIV prevalence and exposure risk.
Effectiveness of PrEP in Reducing New HIV Infections
Numerous studies have demonstrated the effectiveness of PrEP in reducing new HIV infections. These studies have focused on different populations, such as men who have sex with men (MSM), transgender individuals, and people who inject drugs. These groups often experience higher rates of HIV infection due to increased risk factors. Studies consistently show that consistent PrEP use substantially reduces the risk of acquiring HIV.
Data on PrEP Implementation and Reduced HIV Transmission
| Population Group | PrEP Implementation Status | Impact on New HIV Infections |
|---|---|---|
| MSM | Widely implemented in many regions | Significant reduction in new infections in areas with robust PrEP programs |
| People who inject drugs | Implementation varying by region | Positive results observed in areas with strong PrEP access and linkage to care |
| Transgender women | Implementation varying by region | Positive results seen in some areas, emphasizing the importance of tailored interventions |
Epidemiological Trends in Areas with and without PrEP Programs
Epidemiological data clearly show a correlation between the implementation of PrEP programs and a decrease in HIV infection rates. Areas with well-established PrEP programs demonstrate a marked decline in new HIV infections compared to areas without such programs. This difference highlights the substantial public health impact of PrEP.
“Consistent PrEP use can effectively reduce the risk of HIV acquisition by over 90%.”
Factors Influencing PrEP Implementation Success: Prep Implementation Is Associated With A Rapid Decline In New Hiv Infections
PrEP, or pre-exposure prophylaxis, has proven remarkably effective in reducing HIV infections. However, successful implementation hinges on a multitude of factors beyond simply providing the medication. These factors require careful consideration and strategic implementation to maximize the impact of PrEP programs and ensure widespread access and uptake. Effective PrEP programs need to go beyond simply distributing medication.Different implementation strategies, community engagement, healthcare accessibility, and addressing stigma all play critical roles in achieving substantial reductions in HIV transmission.
Understanding these complexities is essential to create and maintain successful PrEP programs.
Comparing PrEP Implementation Strategies
Various strategies exist for implementing PrEP, each with its own strengths and weaknesses. Some focus on targeted outreach to specific populations at higher risk, while others emphasize broader community engagement. Strategies that include mobile clinics or home-based delivery can reach populations who might otherwise face barriers to accessing healthcare. The most effective approach often involves a combination of strategies tailored to the specific context.
Studies show that pre-exposure prophylaxis (PrEP) implementation is strongly linked to a significant drop in new HIV infections. Just like you wouldn’t rely on a little bit of weed to save your life during a heart attack ( weed wont save your life during heart attack ), medical interventions like PrEP are crucial for preventing infections and maintaining health.
Ultimately, responsible health practices, including PrEP, are key to tackling the spread of HIV.
The Role of Community Engagement
Community engagement is paramount to successful PrEP implementation. It fosters trust, encourages participation, and ensures that programs are culturally sensitive and address the unique needs of the communities they serve. Engaging community leaders, health workers, and individuals from the target population is crucial to understand and address local challenges and concerns. This process empowers communities to become active participants in their own health.
Healthcare Access and Affordability
Ensuring equitable healthcare access and affordability is essential for PrEP uptake. Financial barriers can significantly hinder access to medication, regardless of the overall availability. Integrating PrEP into existing healthcare systems and developing innovative financing mechanisms are crucial. Programs should consider options such as subsidies, insurance coverage, and sliding-scale fees to make PrEP accessible to a wider range of individuals.
Impact of Stigma and Social Norms
Stigma and social norms surrounding HIV and PrEP can significantly impact PrEP adherence. Negative attitudes and beliefs can discourage individuals from seeking PrEP, or even from disclosing their use of the medication. Addressing stigma requires targeted education campaigns and community-led initiatives that foster acceptance and understanding. Open dialogue and promoting positive messaging is key to overcoming these obstacles.
Importance of Education and Awareness Campaigns
Education and awareness campaigns play a crucial role in promoting PrEP understanding and uptake. These campaigns should not only explain how PrEP works but also address common misconceptions and concerns. Clear, accessible information, delivered through various channels, is vital for fostering informed decision-making. These campaigns should be culturally appropriate and address the specific needs of the target audience.
Essential Components of a Comprehensive PrEP Implementation Strategy
| Component | Description |
|---|---|
| Community Engagement | Active involvement of community leaders, health workers, and individuals from the target population in program design, implementation, and evaluation. |
| Targeted Outreach | Focus on populations at higher risk of HIV infection through mobile clinics, outreach events, and tailored interventions. |
| Healthcare Access | Integration of PrEP into existing healthcare systems, ensuring affordable and accessible services, and potentially subsidies. |
| Stigma Reduction | Addressing stigma and social norms through education campaigns, community dialogues, and culturally sensitive programs. |
| Comprehensive Education | Providing accurate and accessible information about PrEP, its benefits, and potential side effects, including culturally tailored messaging. |
| Monitoring and Evaluation | Regularly tracking PrEP uptake, adherence, and impact on HIV transmission rates, using data to inform program adjustments. |
Challenges and Considerations in PrEP Implementation
PrEP, or pre-exposure prophylaxis, has proven a powerful tool in preventing HIV transmission. However, widespread and effective implementation faces significant hurdles. Understanding these challenges is crucial for tailoring programs to maximize impact and ensure equitable access for all at risk. Successfully addressing these issues is paramount to realizing the full potential of PrEP in controlling the HIV epidemic.Implementing PrEP programs effectively requires a multifaceted approach that considers various factors.
From logistical hurdles to ensuring equitable access, ethical considerations, and long-term sustainability, each element demands careful attention. The complexities involved in scaling up PrEP programs are not trivial, and demand strategic planning and resource allocation.
Barriers to PrEP Implementation in Various Settings
Various factors impede PrEP access in different communities. These range from social stigma and lack of awareness about PrEP to financial constraints and inadequate healthcare infrastructure. Addressing these barriers requires tailored interventions that consider the specific context of each community. For instance, in resource-limited settings, community-based approaches and simplified adherence strategies might be more effective than traditional clinic-based models.
Logistical Challenges Associated with PrEP Programs
PrEP programs face logistical challenges in procurement, storage, and distribution of PrEP medication. Ensuring appropriate storage conditions for the medication, and efficient delivery mechanisms, particularly in remote areas, is vital. Maintaining a steady supply chain and addressing potential shortages are critical for the long-term sustainability of the program. Moreover, ensuring sufficient healthcare provider training and capacity to properly counsel and monitor patients on PrEP use is crucial for effective implementation.
Ensuring Equitable Access to PrEP
Equitable access to PrEP is essential for its effectiveness in reducing HIV infections. Disparities in access based on socioeconomic status, geographic location, or other factors can significantly limit the program’s impact. Strategies to mitigate these disparities include community outreach programs targeting marginalized populations, mobile clinics in underserved areas, and culturally sensitive PrEP education. This requires understanding and addressing the specific barriers faced by different communities.
Studies show that pre-exposure prophylaxis (PrEP) implementation is strongly linked to a significant drop in new HIV infections. Navigating the challenges of a career with a condition like multiple sclerosis, as explored in this insightful article on difficulties of your job with multiple sclerosis , highlights the often-unseen hurdles we face in maintaining health and well-being. Ultimately, initiatives like PrEP are crucial in preventing the spread of HIV and protecting public health.
Ethical Considerations Related to PrEP Implementation
Ethical considerations surrounding PrEP implementation include informed consent, confidentiality, and potential unintended consequences. Ensuring individuals fully understand the benefits and risks of PrEP before initiating treatment is paramount. Robust confidentiality measures are needed to protect patient privacy. Potential unintended consequences, such as changes in sexual behavior, require careful monitoring and evaluation.
Long-Term Sustainability of PrEP Programs
Long-term sustainability of PrEP programs hinges on securing adequate funding, building strong partnerships, and integrating PrEP into routine healthcare services. Ongoing funding commitments are essential for the continued provision of PrEP. Collaboration with community organizations and healthcare providers is critical for sustaining program engagement and adherence. Integrating PrEP into existing healthcare structures, like routine HIV testing, facilitates broader uptake.
Potential Obstacles and Strategies to Overcome Them in PrEP Programs
| Potential Obstacles | Strategies to Overcome |
|---|---|
| Lack of awareness and knowledge about PrEP | Targeted community outreach, educational campaigns, and partnerships with community health workers |
| Financial constraints | Exploring funding opportunities, developing cost-effective models, and advocating for government funding |
| Social stigma and discrimination | Addressing social stigma through community dialogues, promoting acceptance, and ensuring confidentiality |
| Inadequate healthcare infrastructure | Strengthening healthcare systems, training healthcare providers, and implementing mobile or community-based models |
| Supply chain challenges | Improving procurement systems, implementing robust storage strategies, and establishing backup plans |
Illustrative Examples of Successful PrEP Programs
PrEP, or pre-exposure prophylaxis, has shown remarkable promise in curbing the spread of HIV. Successful implementation of PrEP programs hinges on a multifaceted approach, tailored to the specific needs and context of the target communities. These initiatives often go beyond simply providing medication; they incorporate comprehensive strategies for education, access, and ongoing support. This section will delve into case studies of successful PrEP programs, highlighting the key strategies and impacts they’ve had.Successful PrEP programs aren’t one-size-fits-all.
Their effectiveness relies heavily on tailoring the program to the specific needs of the community, considering factors like social determinants of health, cultural norms, and existing healthcare infrastructure. Understanding the nuanced elements that contribute to success is crucial for replicating these positive outcomes in other contexts.
Successful PrEP Implementation Strategies
PrEP programs that have effectively reduced HIV transmission often employ a combination of strategies. These strategies frequently include community engagement initiatives, tailored education campaigns, and robust access points for medication. These initiatives have demonstrated significant impacts in reducing HIV infections in specific populations.
Community Engagement and Outreach
Effective PrEP programs prioritize community engagement to build trust and address concerns. This often involves partnering with community organizations, healthcare providers, and local leaders to ensure the program aligns with local needs and values. This approach builds trust and facilitates open communication about PrEP.
Accessible and Convenient Access Points
Providing convenient access to PrEP is essential. This includes expanding the availability of PrEP through community health centers, mobile clinics, and partnerships with existing healthcare providers. Making PrEP accessible outside of traditional healthcare settings is crucial for reaching vulnerable populations. These programs often employ strategies to minimize barriers, such as transportation challenges or clinic hours.
Tailored Education and Counseling
Comprehensive education and counseling are critical components of successful PrEP programs. These programs educate individuals about PrEP, its benefits, potential side effects, and adherence strategies. Counseling focuses on individual needs and risk assessments, helping participants understand the program and make informed decisions. These programs are designed to address potential barriers to adherence and support ongoing engagement.
Impact on Specific Communities
The impact of successful PrEP programs on reducing HIV infections in specific communities can be substantial. Programs often target high-risk groups such as men who have sex with men, transgender individuals, and people who inject drugs. The reduction in HIV transmission is not merely statistical but impacts the health and well-being of these communities.
Case Studies and Positive Outcomes
Several regions have reported impressive success stories. For example, a program in the San Francisco Bay Area demonstrated a significant decrease in new HIV infections among men who have sex with men following the implementation of a comprehensive PrEP program. Similar results have been seen in other parts of the United States and globally. These programs show that when designed and implemented effectively, PrEP can dramatically reduce HIV transmission.
Key Lessons Learned from Successful Programs
Analyzing successful PrEP programs reveals key lessons for future initiatives. These include the importance of community engagement, culturally appropriate outreach, and sustained efforts to ensure long-term access to PrEP. These programs highlight the critical role of ongoing monitoring and evaluation to adapt and improve the program as needed.
Table: Key Characteristics of Successful PrEP Programs, Prep implementation is associated with a rapid decline in new hiv infections
| Region | Target Population | Key Strategies | Impact |
|---|---|---|---|
| San Francisco Bay Area (USA) | Men who have sex with men | Community-based outreach, streamlined access, tailored education | Significant decrease in new HIV infections |
| [Specific Region 2] | [Specific Population 2] | [Specific Strategies 2] | [Specific Impact 2] |
| [Specific Region 3] | [Specific Population 3] | [Specific Strategies 3] | [Specific Impact 3] |
Future Directions for PrEP Research

Pre-exposure prophylaxis (PrEP) has proven to be a powerful tool in the fight against HIV, significantly reducing new infections. However, ongoing research is crucial to maximize its impact and ensure its optimal use. This exploration focuses on critical areas for future investigation, aiming to refine PrEP implementation and broaden its reach to vulnerable populations.The future of PrEP research hinges on addressing several key areas, including a deeper understanding of PrEP’s effectiveness across diverse populations, the long-term effects of PrEP use, and strategies for improving access and affordability.
Innovative approaches and comprehensive data collection are essential to ensure that PrEP continues to be an effective and accessible intervention.
Critical Areas for Future PrEP Research
Future research should focus on expanding our understanding of PrEP’s impact on diverse populations. Existing studies have primarily focused on specific demographics, such as cisgender men who have sex with men (MSM). There’s a critical need for comprehensive data on PrEP effectiveness among women, transgender individuals, people of color, and those in marginalized communities. This includes examining the impact of social determinants of health, such as socioeconomic status and access to healthcare, on PrEP adherence and outcomes.
Research should also explore how PrEP interacts with other health conditions and medications.
Long-Term Effects of PrEP Use
Long-term follow-up studies are essential to fully understand the potential long-term effects of PrEP. While short-term safety profiles are well-established, the long-term implications of daily PrEP use on overall health need further investigation. This research should examine potential interactions with other medications, potential hormonal changes, and the impact on kidney function, bone health, and other systems. Data collection on these aspects will help to inform long-term recommendations for PrEP use.
Improving PrEP Access and Affordability
Increasing PrEP access and affordability is crucial to maximizing its impact. Strategies should include exploring innovative financing mechanisms, such as government subsidies and insurance coverage. Collaboration between healthcare providers, policymakers, and community organizations is essential to address logistical challenges, such as ensuring equitable distribution and removing barriers to access. Educational initiatives can also play a significant role in promoting PrEP awareness and addressing potential concerns.
Innovative Strategies for Enhanced PrEP Implementation
Innovative strategies are necessary to further enhance PrEP implementation. These strategies should include developing tailored interventions for specific populations, incorporating PrEP into existing healthcare settings, and exploring new technologies, such as point-of-care testing and mobile health platforms, to improve access and adherence. For example, mobile health applications can provide reminders and support for medication adherence, while point-of-care testing can expedite diagnosis and treatment.
Potential Future Directions of PrEP Research (Summary Table)
| Area of Research | Specific Focus | Expected Outcomes |
|---|---|---|
| PrEP Effectiveness Across Diverse Populations | Comprehensive data collection on diverse groups, including women, transgender individuals, people of color, and marginalized communities. | Improved understanding of PrEP’s effectiveness across a wider spectrum of individuals, potentially revealing disparities and tailoring interventions. |
| Long-Term PrEP Effects | Longitudinal studies examining potential long-term health implications of daily PrEP use. | Improved understanding of the long-term safety and efficacy of PrEP, enabling more informed recommendations and strategies. |
| Access and Affordability | Exploring innovative financing mechanisms, insurance coverage, and improving logistical challenges. | Increased access to PrEP, promoting equity in HIV prevention efforts. |
| Innovative Strategies | Developing tailored interventions, incorporating PrEP into existing healthcare settings, exploring new technologies. | Enhanced PrEP implementation through efficient and accessible models, potentially improving adherence and outcomes. |
Conclusion
In conclusion, the evidence overwhelmingly supports the vital role of PrEP in combating the HIV epidemic. From understanding the fundamentals of PrEP to evaluating its effectiveness and acknowledging the challenges in implementation, this discussion underscores the importance of proactive measures to reduce HIV transmission and ultimately achieve a future free from the scourge of this disease. The ongoing research and implementation of PrEP programs will undoubtedly continue to shape global health strategies for years to come.