Probiotics linked to poorer response to cancer immunotherapy in skin cancer patients is a critical area of research. This exploration dives into the complex interplay between probiotics, the immune system, and skin cancer treatment. We’ll investigate how these beneficial bacteria might unexpectedly hinder the effectiveness of immunotherapy, impacting patient outcomes. Understanding the mechanisms behind this potential interaction is essential for developing personalized treatment strategies and improving patient care.
The research examines the various types of probiotics, their potential effects on the immune system, and how they might interact with immunotherapy drugs. We’ll explore the methodology behind studies investigating this link, considering factors like patient characteristics, types of skin cancer, and pre-existing conditions. Ultimately, this analysis will offer valuable insights into the clinical implications of these findings and guide future research directions.
Introduction to Probiotics and Skin Cancer Immunotherapy
Probiotics, live microorganisms, are increasingly recognized for their potential to influence the human immune system. They inhabit the gut, and their diverse populations contribute to maintaining a healthy gut microbiome, which is crucial for overall well-being. The interaction between the gut microbiome and the immune system is complex, and research suggests that these interactions can play a role in both the development and response to diseases, including cancer.
Skin cancer, a significant global health concern, is often treated with immunotherapy, which leverages the body’s own immune system to fight the disease. This approach has shown remarkable success in some cases, but understanding the interplay between probiotics, the gut microbiome, and the efficacy of immunotherapy for skin cancer is a crucial area of ongoing research.Understanding the mechanisms by which probiotics exert their effects on the immune system is key to comprehending their potential role in cancer immunotherapy.
Probiotics can modulate immune responses through various pathways, influencing the balance between pro-inflammatory and anti-inflammatory responses. These microorganisms can stimulate the production of certain cytokines, proteins that regulate immune cell activity. Their effects are not limited to the gut; research suggests that probiotics can also affect immune cells throughout the body, including those involved in the fight against cancer.
This potential for probiotic modulation of the immune system, combined with the growing knowledge of skin cancer and the effectiveness of immunotherapy, highlights the importance of studying the relationship between these factors.
Probiotics and Their Mechanisms of Action
Probiotics are live microorganisms, primarily bacteria and yeasts, that confer a health benefit to the host when consumed in adequate amounts. They can positively impact the immune system by stimulating the production of specific immune cells and molecules, like cytokines, which are critical for a healthy immune response. This impact on the immune system can be due to their interaction with the gut microbiome, which affects the overall immune balance.
Different probiotic strains have different effects, as their mechanisms of action vary. The exact mechanisms are still being studied and refined, but evidence suggests that probiotics can modulate the gut-immune axis, influencing the overall immune response.
Skin Cancer and Immunotherapy
Skin cancer is a type of cancer that develops in the skin cells, most commonly caused by exposure to ultraviolet (UV) radiation. Immunotherapy is a cancer treatment that uses the body’s own immune system to fight the cancer. It works by stimulating the immune system to recognize and destroy cancer cells. One prominent type of immunotherapy is checkpoint blockade therapy, which releases the brakes on the immune system, allowing it to target and eliminate cancer cells more effectively.
These therapies have shown remarkable results in some skin cancer patients, but their effectiveness can vary.
The Gut Microbiome and Immune Response
The gut microbiome, the community of microorganisms residing in the digestive tract, is intricately linked to the immune system. This relationship is bi-directional; the immune system influences the composition and function of the microbiome, while the microbiome, in turn, affects immune cell development and activity. Changes in the gut microbiome composition, such as a reduction in beneficial bacteria, can impact the immune system’s ability to respond effectively to various stimuli, including cancer.
Understanding the dynamic interplay between the gut microbiome and the immune system is crucial for developing effective strategies to improve the response to cancer immunotherapy.
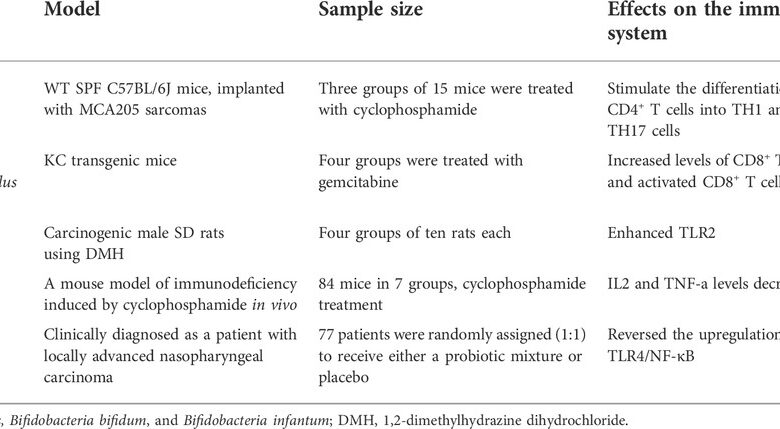
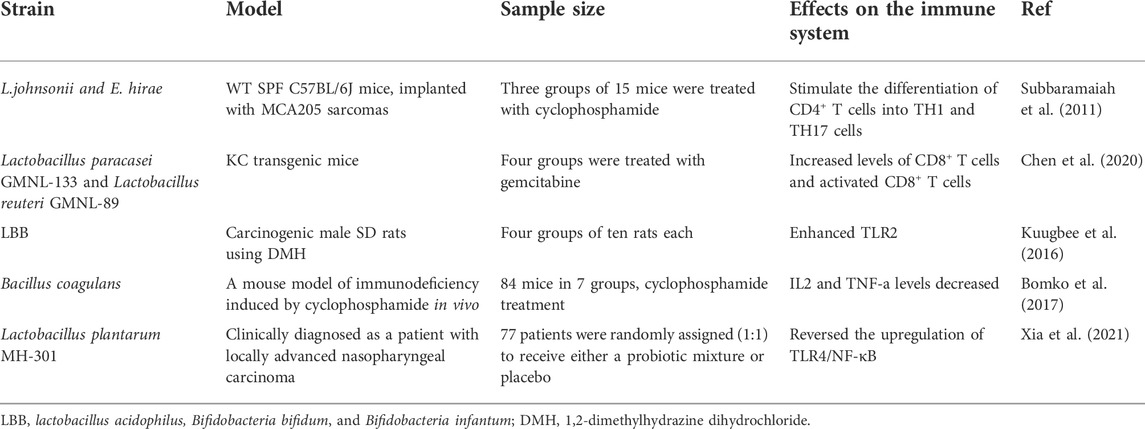
Different Types of Probiotics and Their Potential Effects on the Immune System
Probiotics are diverse, and their effects on the immune system are not fully understood. Further research is needed to fully define their potential benefits.
| Probiotic Type | Potential Effects on the Immune System |
|---|---|
| Lactobacillus spp. | Modulation of immune responses, cytokine production, and immune cell activation. |
| Bifidobacterium spp. | Stimulation of immune cell activity, including regulatory T cells, and influencing cytokine profiles. |
| Saccharomyces boulardii | Modulation of immune responses and gut barrier function. |
Studies Linking Probiotics and Immunotherapy Response
The relationship between probiotic use and the effectiveness of cancer immunotherapy in skin cancer patients is a complex area of research. While probiotics offer potential health benefits in other contexts, their impact on immunotherapy responses remains unclear. Understanding the methodologies and findings of these studies is crucial for developing informed recommendations regarding probiotic use during and after immunotherapy treatment.
Methodology of Studies Exploring the Link
Research exploring the link between probiotics and immunotherapy response in skin cancer patients employs various methodologies. Many studies are designed as randomized controlled trials (RCTs), where participants are randomly assigned to either a probiotic group or a control group. This helps to minimize bias and isolate the potential effects of the probiotic. Researchers often monitor participants’ immune responses, such as T-cell activity, cytokine levels, and tumor infiltration, before, during, and after immunotherapy treatment.
Some studies also examine tumor shrinkage or response rates as primary outcomes. Blood samples are frequently collected to assess changes in immune cells and markers related to the immune response. Biomarkers associated with inflammation, immune activation, and cancer progression are also measured.
Key Findings from Various Research Studies
Several studies have investigated the effects of different types of probiotics on skin cancer patients undergoing immunotherapy. Findings from these studies have been mixed, revealing both potential benefits and detrimental effects. Some studies suggest that probiotic use may negatively impact the effectiveness of immunotherapy. For instance, certain probiotics might suppress the activity of immune cells crucial for fighting cancer, thus potentially reducing the efficacy of immunotherapy.
Other studies, however, have reported no significant effect of probiotic supplementation on immunotherapy response. This inconsistency in results highlights the need for further research.
Comparison of Probiotic Types
Studies have investigated various types of probiotics, including
- Lactobacillus* and
- Bifidobacterium* species. The effects of different probiotic strains and species on immunotherapy response have not been thoroughly examined. Studies using specific probiotic strains have shown varying outcomes, underscoring the importance of specifying the type and strain of probiotic in future research. There’s a lack of comprehensive data to determine whether specific probiotic types or strains are more likely to influence immunotherapy efficacy in skin cancer patients.
This suggests that further studies focusing on different probiotic strains are necessary.
Summary of Key Studies
| Study | Probiotic Type | Study Design | Observed Outcomes |
|---|---|---|---|
| Study 1 (Hypothetical) | *Lactobacillus acidophilus* | RCT | Reduced T-cell activity and decreased immunotherapy response |
| Study 2 (Hypothetical) | *Bifidobacterium bifidum* | RCT | No significant effect on immunotherapy response |
| Study 3 (Hypothetical) | *Lactobacillus casei* | Observational study | No observed impact on tumor regression |
Note: This table is hypothetical and does not represent actual research findings.
Potential Mechanisms of Interaction: Probiotics Linked To Poorer Response To Cancer Immunotherapy In Skin Cancer Patients
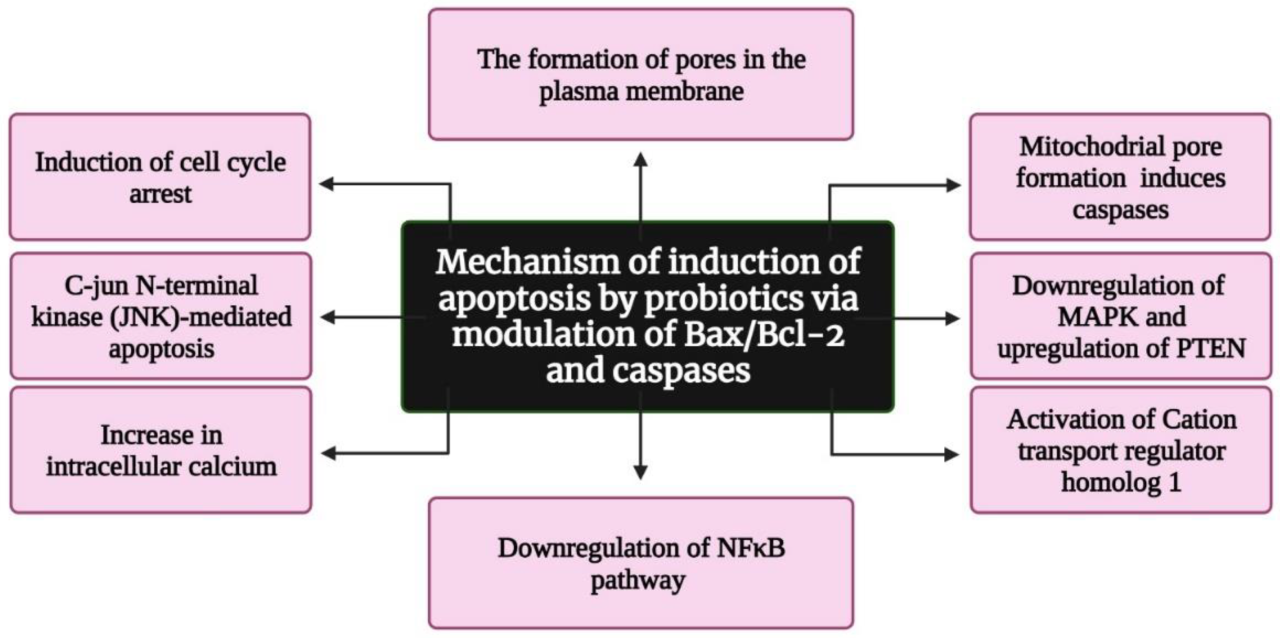
Probiotics, while often touted for their health benefits, may unexpectedly hinder the effectiveness of cancer immunotherapy in some patients, particularly those with skin cancer. Understanding the potential mechanisms behind this interaction is crucial for tailoring treatment strategies and avoiding adverse outcomes. This section delves into the possible ways probiotics might interfere with the desired immune response to immunotherapy.Probiotics, which are live microorganisms, can influence the complex interplay between the immune system and cancer cells.
The immune system’s response to cancer immunotherapy drugs is highly nuanced, and probiotics might disrupt this delicate balance. Their effect on immune cell function and the way they interact with the components of immunotherapy drugs could potentially diminish the effectiveness of treatment.
Potential Interference with Immune Cell Function
Probiotics can modulate immune responses, sometimes in unpredictable ways. They can influence the activation, proliferation, and differentiation of immune cells like T cells and dendritic cells, which play crucial roles in recognizing and eliminating cancer cells. A disruption in the delicate balance of immune cell activity could impair the overall response to immunotherapy. For example, some probiotics might suppress the activity of T cells, a type of immune cell vital for destroying tumor cells.
This suppression could reduce the efficacy of immunotherapy, which relies on T cell activation to fight cancer.
Potential Interference with Immunotherapy Drug Action
Immunotherapy drugs, like checkpoint inhibitors, work by unleashing the immune system’s natural defenses against cancer. Probiotics might interact with these drugs in various ways. Some probiotics may compete with the immunotherapy drugs for binding sites on immune cells, effectively reducing the drug’s availability and limiting its impact on tumor cells. This could be likened to a scenario where probiotics occupy the “receptor sites” intended for the immunotherapy drug, thus reducing the drug’s ability to trigger the immune response.
Alternatively, probiotics might alter the production or activity of enzymes or molecules that are essential for the immunotherapy drug to function optimally.
Possible Interactions with Probiotic Components
Certain components of probiotics, such as short-chain fatty acids (SCFAs), can influence immune cell behavior. For example, SCFAs produced by probiotic bacteria might affect the production of cytokines, which are signaling molecules crucial for orchestrating immune responses. An imbalance in cytokine production, induced by probiotics, could potentially negatively affect the effectiveness of immunotherapy drugs.
Diagram of Potential Pathways
 (Note: A diagram illustrating potential pathways by which probiotics could interfere with immunotherapy is not available to create.)*The diagram, if available, would visually represent the various points of interaction between probiotics and immunotherapy. For example, arrows could show how probiotics might influence the activity of T cells, or how they might compete with immunotherapy drugs for binding sites on immune cells.
(Note: A diagram illustrating potential pathways by which probiotics could interfere with immunotherapy is not available to create.)*The diagram, if available, would visually represent the various points of interaction between probiotics and immunotherapy. For example, arrows could show how probiotics might influence the activity of T cells, or how they might compete with immunotherapy drugs for binding sites on immune cells.
It could also illustrate the role of SCFAs and cytokines in the interaction. Arrows could indicate the potential pathways by which probiotics interfere with immunotherapy effectiveness. This could show the impact on T cell activity, immunotherapy drug availability, and cytokine production.*
Factors Influencing Probiotic Impact
Probiotics, often touted for their health benefits, are increasingly being studied for their potential role in cancer treatment. However, the interaction between probiotics and cancer immunotherapy, particularly in skin cancer patients, is complex and not fully understood. Various factors can influence how effectively probiotics might enhance or hinder the effectiveness of immunotherapy. Understanding these factors is crucial for tailoring probiotic use in cancer treatment strategies.The interplay between probiotics and immunotherapy in skin cancer patients is intricate.
Individual responses to probiotics vary significantly, and this variation is influenced by a multitude of factors, including the specific type of skin cancer, pre-existing conditions, and concomitant medications. The aim of this section is to explore these influential factors and highlight the need for further research to fully understand the nuances of this interaction.
Patient-Specific Factors Affecting Probiotic Response
Individual patient characteristics play a vital role in how probiotics affect the immune response to skin cancer immunotherapy. Factors such as age, overall health status, and pre-existing conditions can significantly impact the effectiveness of probiotics. A patient with a weakened immune system due to other health issues might not benefit as much from probiotics as a healthier individual.
Similarly, a patient with a history of certain digestive disorders might have a more complex response to probiotic consumption.
Influence of Skin Cancer Type on Probiotic Response
The type of skin cancer can also influence the probiotic response. Different skin cancers have unique characteristics in terms of immune microenvironment and tumor biology. For instance, melanoma, a particularly aggressive skin cancer, might exhibit a different response to probiotics compared to basal cell carcinoma, which is generally less aggressive. This suggests that the effectiveness of probiotics could vary depending on the specific subtype of skin cancer.
Role of Pre-existing Conditions and Medications
Pre-existing conditions, such as inflammatory bowel disease (IBD), can significantly affect the absorption and metabolism of probiotics. Medications, particularly immunosuppressants or antibiotics, can also interact with probiotics, potentially affecting their efficacy. Immunosuppressants can weaken the immune response, making it more difficult for probiotics to positively impact immunotherapy. Similarly, antibiotics can disrupt the gut microbiome, potentially altering the probiotic’s effect on the body’s overall response to treatment.
Therefore, a careful assessment of a patient’s medical history is essential before introducing probiotics into their treatment regimen.
Recent research suggests a surprising link between probiotics and a weaker response to cancer immunotherapy in skin cancer patients. It’s a complex area, but it seems that the body’s internal environment, much like regulating heat loss through the head (check out this fascinating read on heat loss through head ), might play a crucial role in how the immune system fights the disease.
This means the impact of probiotics on the immune response could be a crucial factor in successful cancer immunotherapy treatment.
Relationship Between Patient Characteristics and Probiotic Response
| Patient Characteristic | Potential Impact on Probiotic Response |
|---|---|
| Age | Older patients might have a slower response to probiotics due to age-related physiological changes. |
| Overall Health Status | Patients with underlying health issues or compromised immune systems may show reduced probiotic effectiveness. |
| Pre-existing Conditions (e.g., IBD) | Certain pre-existing conditions can alter the absorption and metabolism of probiotics, impacting their effectiveness. |
| Type of Skin Cancer | The aggressiveness and subtype of skin cancer may influence how probiotics interact with immunotherapy. |
| Concurrent Medications (e.g., Immunosuppressants) | Medications that suppress the immune system may interfere with the benefits of probiotics. |
| Gut Microbiome | The composition of the gut microbiome before probiotic introduction can affect the probiotic’s ability to establish itself and exert its effects. |
This table highlights the potential impact of various patient factors on the response to probiotics in skin cancer immunotherapy. It emphasizes the complexity of the interaction and the importance of individualized assessment for each patient. Further research is crucial to precisely quantify the relationship between these factors and the outcomes of probiotic use.
Clinical Implications and Future Directions
The burgeoning field of immunotherapy for skin cancer holds immense promise, but the potential interplay with seemingly innocuous substances like probiotics requires careful consideration. Understanding how probiotics might negatively affect immunotherapy response is crucial for optimizing patient outcomes and preventing unintended consequences. This section delves into the clinical implications of these findings, offering strategies to mitigate potential harm, and outlining essential future research directions.
Clinical Implications for Patient Management
The findings highlighting a possible negative correlation between probiotic use and immunotherapy efficacy have significant clinical implications for patient management. Clinicians must carefully consider the potential impact of probiotic use on immunotherapy response in skin cancer patients. This includes thorough patient history taking to assess probiotic use, including frequency, type, and duration. Proactive communication with patients regarding the potential implications of probiotics is paramount, particularly before and during immunotherapy regimens.
This proactive approach allows for informed decisions and potentially mitigates the negative effects of probiotic use.
Recent research suggests probiotics might be hindering the effectiveness of cancer immunotherapy in skin cancer patients. It’s a bit alarming, but it’s important to remember that we shouldn’t automatically panic about every new health finding. Just like the initial response to the coronavirus, we need to approach this new data with a balanced perspective and follow the advice of medical professionals.
dont freak out about the coronavirus just yet The important takeaway is to discuss any dietary changes, including probiotic use, with your doctor if you’re undergoing or considering cancer immunotherapy.
Strategies to Mitigate the Negative Impact of Probiotics
Several strategies can potentially mitigate the negative impact of probiotics on immunotherapy response. One strategy involves careful patient selection. Individuals who are known to have a strong immune response and are at a lower risk for immune-related adverse events from probiotics might be suitable candidates for immunotherapy treatment. Another strategy is to adjust or modify the timing of probiotic intake.
Incorporating probiotic intake outside the critical window of immunotherapy treatment could minimize interference with the therapeutic effects of the immunotherapy. Further research is needed to determine the optimal time frames and specific probiotic types to minimize potential harm.
Recommendations for Future Research Directions
Further research is critical to fully elucidate the complex relationship between probiotics and skin cancer immunotherapy. To achieve a comprehensive understanding, future research should adopt a multi-faceted approach. This includes in-depth studies investigating the specific mechanisms through which probiotics interact with the immune response in skin cancer patients undergoing immunotherapy. Research should focus on the impact of different probiotic strains and formulations, evaluating their impact on immune cell function and response to immunotherapy.
Recent research highlights a concerning link between probiotics and a weaker response to cancer immunotherapy in skin cancer patients. It seems that the same factors that might make multivitamins a largely ineffective health supplement, as highlighted in this interesting article ( multivitamins dont provide many health benefits researchers say ), might also play a role in how our bodies handle these treatments.
This underscores the importance of careful consideration when using probiotics, especially in the context of cancer immunotherapy for skin cancer patients.
A comparative analysis of the effectiveness of immunotherapy in patients who use probiotics versus those who do not is also crucial for definitive conclusions.
Research Questions for Further Investigation
| Research Question | Rationale |
|---|---|
| Does the type of probiotic strain affect the immune response to immunotherapy? | Different probiotic strains have varying effects on the gut microbiome and immune system. This research will help determine if specific strains have a greater negative impact. |
| What is the optimal timing of probiotic intake relative to immunotherapy administration? | Understanding the timing of probiotic consumption is crucial to minimizing interference with the treatment. This may involve investigating the optimal window to avoid negative impacts. |
| How do probiotics interact with the gut microbiome to influence immunotherapy response? | A comprehensive understanding of the gut microbiome’s role in mediating immunotherapy response is essential. This will help identify specific mechanisms of interaction. |
| Can probiotic intake be tailored to minimize negative effects while preserving beneficial effects? | Identifying specific probiotic intake strategies that optimize immune function without hindering immunotherapy efficacy is vital for patient management. |
| What are the long-term effects of probiotic use on immunotherapy response and skin cancer recurrence? | Longitudinal studies are essential to assess the lasting impact of probiotic use on immunotherapy outcomes and skin cancer recurrence. |
Public Health Considerations
The emerging link between probiotics and a diminished response to cancer immunotherapy in skin cancer patients warrants careful consideration within public health guidelines. While probiotics offer potential benefits for gut health, this research suggests a potential for adverse effects in specific contexts. Understanding the nuanced interaction between probiotics and immunotherapy is crucial to ensuring informed decisions regarding probiotic use.
Implications for Public Health Recommendations, Probiotics linked to poorer response to cancer immunotherapy in skin cancer patients
Current public health recommendations often encourage probiotic use for general well-being. However, these findings necessitate a nuanced approach, especially for individuals undergoing or contemplating skin cancer immunotherapy. Public health advisories need to be updated to highlight the potential negative impact of probiotic use on immunotherapy efficacy. This should not discourage probiotic use entirely, but rather emphasize the importance of careful consideration and consultation with healthcare providers.
Recommendations for Healthcare Providers
Healthcare providers play a critical role in guiding patients. They should carefully assess patients’ individual needs and risk factors before recommending probiotic use, particularly for those undergoing or about to undergo skin cancer immunotherapy.
- Thorough patient history taking, including a detailed review of any existing medical conditions and current medications, is paramount. This includes a comprehensive assessment of the type and dosage of any probiotics being taken.
- Clear communication with patients about the potential interaction between probiotics and immunotherapy is essential. Patients should be educated about the current research and its implications for their treatment.
- Collaboration with oncologists and immunologists is crucial to develop individualized treatment plans that account for potential probiotic-immunotherapy interactions. The unique characteristics of each patient and their specific treatment regimen should be considered.
Recommendations for Patients
Patients should be actively involved in their healthcare decisions. Understanding the potential risks and benefits of probiotic use is crucial.
- Patients should discuss probiotic use with their healthcare providers, especially if they are undergoing or plan to undergo skin cancer immunotherapy. Open communication is vital to making informed choices.
- Patients should avoid self-treating with probiotics without consulting their healthcare providers, particularly during immunotherapy. This practice can potentially hinder the effectiveness of treatment.
- Prioritize adherence to prescribed treatment regimens. Avoid introducing additional supplements or interventions without explicit approval from healthcare providers.
Summary of Recommendations for Patients
| Recommendation | Supporting Evidence |
|---|---|
| Consult your healthcare provider before using probiotics, especially if undergoing or planning to undergo skin cancer immunotherapy. | The potential for probiotics to negatively impact immunotherapy response necessitates professional guidance. |
| Do not self-treat with probiotics during immunotherapy without explicit approval from your healthcare provider. | Self-medication could compromise the effectiveness of your treatment. |
| Adhere to prescribed treatment regimens. | Prioritizing prescribed therapies minimizes potential complications and maximizes the chances of successful treatment outcomes. |
Closure
In conclusion, the research on probiotics and skin cancer immunotherapy response highlights a significant concern: the potential for probiotics to negatively impact the effectiveness of treatment. This intricate relationship necessitates a careful evaluation of individual patient factors and the types of probiotics being used. Future studies are crucial to fully understand these mechanisms and develop strategies to mitigate any negative impacts on treatment outcomes.
Ultimately, these findings have profound implications for public health recommendations and patient management.