Pulmonary arterial hypertension prognosis offers a crucial look at the journey faced by those battling this complex disease. Understanding the factors that influence outcomes, from diagnosis to long-term survival, is essential for navigating this intricate health challenge.
This comprehensive exploration will cover everything from the initial diagnosis and available treatments to the impact on quality of life and the latest research in the field. We’ll examine the diverse types of pulmonary arterial hypertension, their underlying causes, and the crucial role of individual characteristics in shaping the prognosis for each patient.
Introduction to Pulmonary Arterial Hypertension (PAH)
Pulmonary arterial hypertension (PAH) is a progressive and often life-threatening condition characterized by increased pressure in the blood vessels of the lungs. This elevated pressure hinders the flow of blood from the heart to the lungs, making it difficult for the heart to pump efficiently. The condition gradually damages the delicate blood vessels in the lungs, reducing their ability to deliver oxygen to the body.Understanding the complexities of PAH is crucial for both patients and healthcare professionals.
It’s a condition that affects the entire cardiovascular system, impacting not only lung function but also the heart’s ability to perform its vital role. Recognizing the symptoms and potential causes is paramount for early diagnosis and appropriate treatment.
Types of Pulmonary Arterial Hypertension
PAH isn’t a single disease entity but rather a spectrum of conditions. While the exact cause isn’t always known, various factors can contribute to its development. Some types are associated with specific underlying conditions, while others occur seemingly without any identifiable cause.
Causes and Characteristics of PAH
| Disease Type | Cause | Symptoms | Impact on Cardiovascular System |
|---|---|---|---|
| Idiopathic PAH | Unknown; no identifiable underlying cause. | Early symptoms often include shortness of breath, fatigue, chest pain, and dizziness. As the disease progresses, symptoms like lightheadedness, edema, and fainting episodes may occur. | Increased pressure in the pulmonary arteries leads to right heart strain, ultimately potentially causing right-sided heart failure (cor pulmonale). |
| Heritable PAH | Genetic mutations can predispose individuals to PAH. | Symptoms are similar to idiopathic PAH, often appearing at a younger age. | Similar to idiopathic PAH, heritable PAH leads to increasing pressure in the pulmonary arteries, resulting in strain on the right ventricle. |
| PAH associated with connective tissue disorders (e.g., scleroderma, lupus) | Certain autoimmune conditions are linked to PAH. | Symptoms often overlap with the symptoms of the underlying connective tissue disorder, potentially including joint pain, skin changes, and fatigue. | The underlying condition, combined with PAH, puts significant strain on the right side of the heart. |
| PAH associated with HIV infection | HIV infection can sometimes lead to PAH. | Symptoms include shortness of breath, fatigue, and chest pain. Individuals may experience other HIV-related symptoms as well. | PAH in HIV patients further burdens the heart, compounding the cardiovascular strain. |
Symptoms of Pulmonary Arterial Hypertension, Pulmonary arterial hypertension prognosis
Recognizing the early symptoms of PAH is vital for timely intervention. Early detection allows for earlier treatment and potentially better outcomes. Common symptoms include shortness of breath, especially during exertion, fatigue, chest pain, dizziness, and swelling in the ankles and legs. In more advanced stages, symptoms may include fainting spells, lightheadedness, and palpitations.
Diagnostic Methods and Criteria: Pulmonary Arterial Hypertension Prognosis
Unveiling the complexities of pulmonary arterial hypertension (PAH) requires a precise diagnostic journey. The diagnostic process often involves a series of tests to confirm the diagnosis and determine the specific subtype and severity of the disease. Accurate identification of PAH is crucial for appropriate treatment and improved patient outcomes.
Diagnostic Procedures for PAH
The diagnostic pathway for PAH typically begins with a thorough evaluation of the patient’s medical history and a physical examination. This initial assessment helps to identify potential risk factors and symptoms that might suggest PAH. Subsequent tests are designed to gather objective data and confirm or rule out the diagnosis.
Criteria for Classifying and Staging PAH
The classification and staging of PAH are essential for guiding treatment decisions and predicting prognosis. These criteria are based on various factors, including the severity of the disease, the presence of specific symptoms, and the results of diagnostic tests.
Diagnostic Tests and Their Roles in Diagnosing PAH
A variety of diagnostic tests are employed to evaluate patients suspected of having PAH. Each test plays a specific role in assessing different aspects of the cardiovascular system and the lungs. The following table provides a comparative overview of common diagnostic tests:
| Test | Role in Diagnosing PAH |
|---|---|
| Echocardiography | Provides a visual assessment of the heart’s structure and function. It can detect right ventricular enlargement, a common feature in PAH. It also assesses the severity of valve abnormalities, which may be present in some cases. |
| Pulmonary Function Tests (PFTs) | Evaluates lung function, particularly the ability of the lungs to transfer oxygen and carbon dioxide. Reduced lung capacity or diffusion capacity can suggest the presence of PAH, but PFTs are not typically definitive for diagnosis. |
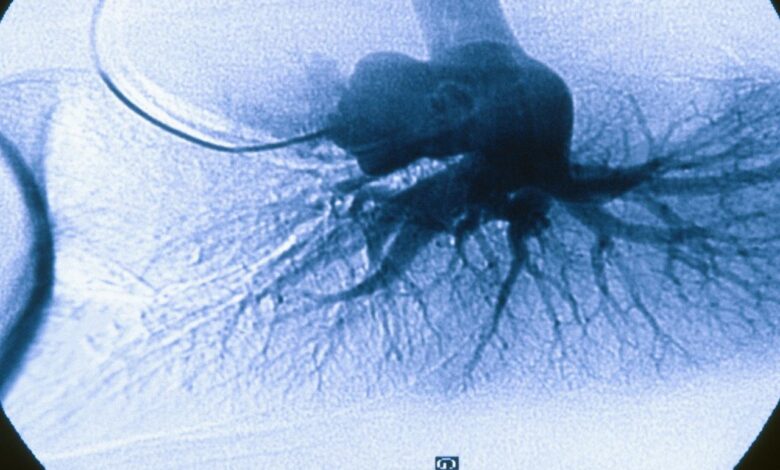
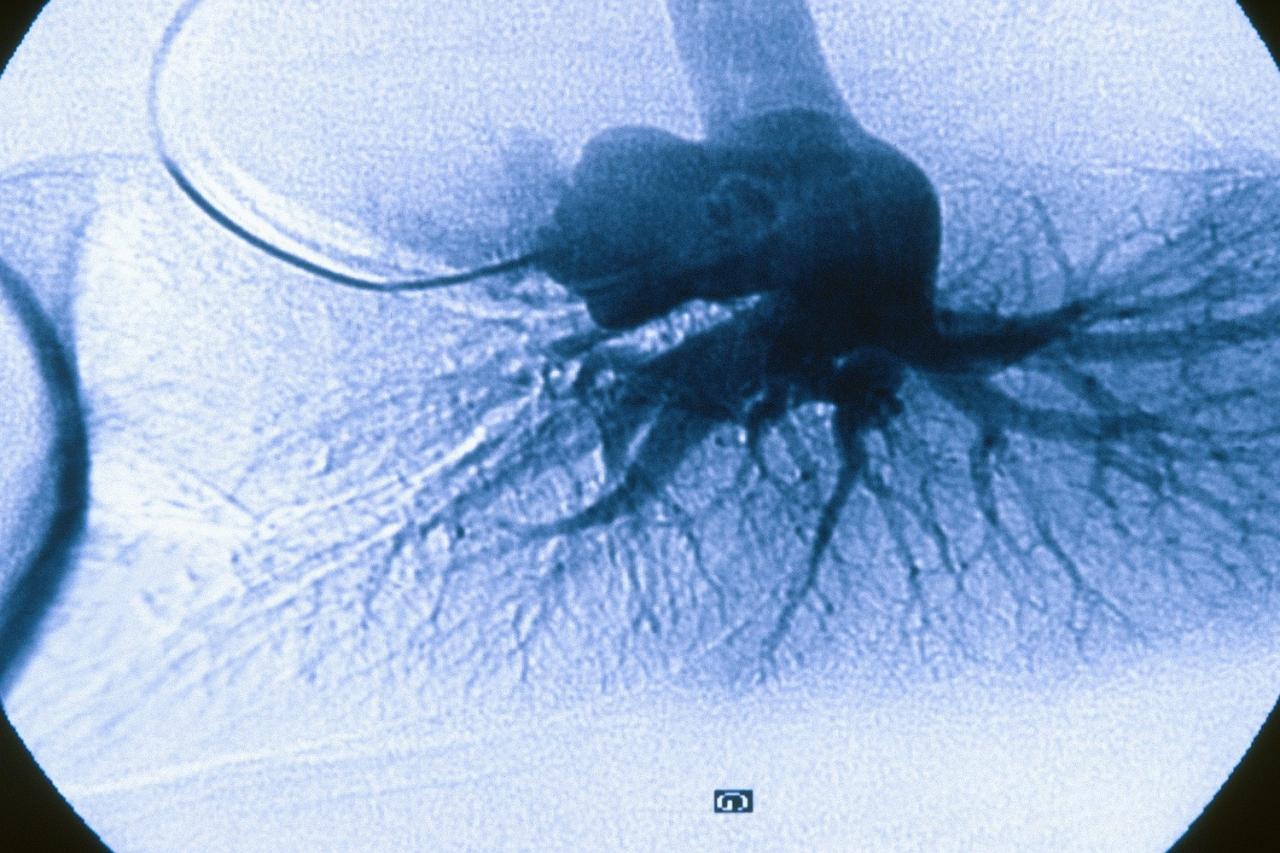
| Right Heart Catheterization | Provides the most definitive assessment of PAH. This invasive procedure involves inserting a catheter into the right side of the heart. It allows for direct measurement of pressures within the heart chambers and pulmonary arteries. This crucial test directly measures pulmonary artery pressure, a key indicator of PAH. Furthermore, it helps to differentiate PAH from other conditions with similar symptoms. |
| Blood Tests | Blood tests are conducted to assess the overall health status and rule out other conditions that might mimic PAH. For instance, tests for inflammatory markers or specific blood cell counts might provide clues. |
| Cardiac MRI | Cardiac MRI provides detailed images of the heart and great vessels. It can identify structural abnormalities, assess right ventricular function, and provide further insights into the extent of disease. |
Role of Right Heart Catheterization in Diagnosing PAH
Right heart catheterization remains a cornerstone of the diagnostic process for PAH. It provides crucial hemodynamic data, including pulmonary artery pressure, which is a key diagnostic criterion. The procedure involves inserting a catheter into a vein, typically in the groin, and guiding it through the heart to measure pressures and oxygen saturations. The information obtained during right heart catheterization is vital for determining the severity of PAH and differentiating it from other conditions.
A key aspect of this procedure is that it allows for direct measurement of pulmonary artery pressures. This crucial information enables accurate diagnosis and facilitates the selection of appropriate therapies. Furthermore, it can help assess the response to treatment. This detailed approach is essential for creating a personalized treatment plan tailored to each patient’s unique needs.
Factors Influencing Prognosis
Predicting the course of pulmonary arterial hypertension (PAH) is crucial for personalized treatment strategies and patient management. Understanding the factors that influence prognosis allows clinicians to tailor interventions to maximize patient outcomes and improve quality of life. The severity of PAH, specific subtypes, associated comorbidities, and individual patient responses to treatment all play significant roles in determining the long-term outlook for PAH patients.The prognosis for individuals with PAH is highly variable, ranging from a relatively benign course to a rapidly progressive and fatal condition.
This variability underscores the importance of considering multiple factors when assessing the potential trajectory of a particular patient’s disease.
Severity of PAH
The severity of PAH directly impacts prognosis. PAH is typically classified into five groups based on hemodynamic parameters, reflecting the degree of pressure in the pulmonary arteries. Patients with more severe PAH, as reflected by higher pulmonary artery pressures and lower cardiac output, tend to have a poorer prognosis compared to those with milder disease. The functional class of the patient, which reflects the degree of physical limitations, is also closely correlated with the severity of the disease and its impact on the prognosis.
For example, patients with severe PAH may experience significant limitations in daily activities and have a lower quality of life compared to those with less severe disease.
The prognosis for pulmonary arterial hypertension (PAH) can be challenging, often impacting quality of life significantly. While the outlook varies greatly depending on the individual and stage of the disease, advancements in treatment are offering hope. Interestingly, researchers are also exploring how generic opioids, a key aspect of the ongoing opioid crisis, might be leveraged to manage pain associated with PAH.
To learn more about the innovative approaches to combating the opioid crisis with generic opioids, check out this article: generic opioids battle opioid epidemic. Ultimately, PAH treatment requires a multifaceted approach that considers the patient’s unique needs and the ever-evolving landscape of medical research.
PAH Subtypes
Different PAH subtypes exhibit distinct prognostic implications. While idiopathic PAH (iPAH) is the most common type, other subtypes such as heritable PAH (hPAH), PAH associated with connective tissue disorders (e.g., scleroderma), and PAH associated with other conditions (e.g., HIV) may have varying degrees of severity and progression. The underlying mechanisms and genetic factors influencing each subtype can significantly impact the disease trajectory and treatment response, leading to varying outcomes.
For instance, hPAH may show a more aggressive course in some individuals than iPAH.
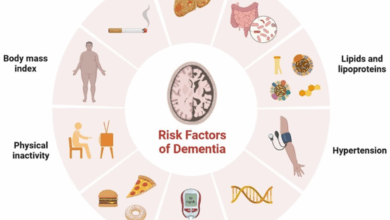
Comorbidities
The presence of comorbidities significantly influences PAH prognosis. Conditions such as chronic obstructive pulmonary disease (COPD), coronary artery disease, and other cardiovascular issues can exacerbate the underlying pathophysiology of PAH and reduce the effectiveness of treatment. The presence of other co-morbidities can complicate treatment and contribute to adverse outcomes. Patients with concurrent conditions may experience a more rapid decline in their functional status and overall health.
Pulmonary arterial hypertension (PAH) prognosis can be tricky, varying greatly depending on the individual and treatment response. Factors like the severity of the condition and how well a patient adheres to their medication plan play a significant role. It’s also important to consider the impact of co-occurring conditions, such as those affecting mental health, like depression and anxiety, which can be common in patients with conditions like idiopathic pulmonary fibrosis (IPF).
For more information on the connection between depression, anxiety, and IPF, check out this helpful resource: depression anxiety and ipf. Ultimately, a holistic approach to PAH management, including mental well-being, is key to improving prognosis.
For example, a patient with both PAH and COPD might have a worse prognosis compared to one with PAH alone due to the additive effects on their respiratory and cardiovascular systems.
Correlation Between PAH Characteristics and Prognosis
| PAH Characteristic | Impact on Prognosis |
|---|---|
| Severity (e.g., functional class) | Higher severity generally associated with poorer prognosis. |
| Subtype (e.g., iPAH, hPAH) | Some subtypes (e.g., hPAH) may have more aggressive courses than others. |
| Comorbidities (e.g., COPD, CAD) | Presence of comorbidities often worsens prognosis due to additive effects on health. |
| Treatment Response | Adequate treatment response and adherence to medication regimen is crucial for a favorable prognosis. |
| Age | Age is a factor. Older age can be associated with poorer prognosis in some studies. |
| Right Ventricular Dysfunction | Progression of right ventricular dysfunction is often a marker of poor prognosis. |
Treatment Options and Their Impact on Prognosis
Pulmonary arterial hypertension (PAH) is a progressive and life-threatening condition, necessitating a multifaceted approach to treatment. Effective management hinges on a tailored treatment plan that addresses the underlying pathophysiology and individual patient needs. The prognosis for PAH patients has significantly improved with the advent of targeted therapies, but understanding the nuances of each treatment option is crucial for optimizing outcomes.The success of PAH treatment is not solely determined by the individual therapy, but rather by a combination of factors, including the patient’s response, adherence to the treatment plan, and timely intervention for any adverse effects.
The goal is not just to prolong life but to improve the quality of life for PAH patients, allowing them to participate in activities and maintain their independence for as long as possible.
Available Treatment Options
Various pharmacological and procedural therapies are employed to manage PAH. These include medications aimed at relaxing blood vessels, reducing inflammation, and enhancing the heart’s function. Surgical interventions are also considered in specific situations. A thorough understanding of each treatment option is essential for appropriate patient selection and optimal management.
Navigating the prognosis of pulmonary arterial hypertension (PAH) can feel daunting, but staying motivated is key. Finding new ways to maintain a healthy lifestyle is crucial, and that’s where activities like starting to run during the pandemic come in. Learning how to stay motivated and avoid injuries while getting back into running can be incredibly beneficial, as detailed in this great resource: begin running during the pandemic how to stay motivated avoid injury.
Ultimately, maintaining a positive outlook and focusing on manageable goals, like a consistent running routine, is a powerful tool for managing the long-term outlook of PAH.
Medications for PAH
A range of medications are used to treat PAH, each with a specific mechanism of action. These medications are categorized based on their effects on the pulmonary vasculature and the underlying pathophysiological mechanisms.
- Phosphodiesterase-5 (PDE5) Inhibitors: These medications, such as sildenafil and tadalafil, work by relaxing the pulmonary blood vessels. They are often the first-line treatment for PAH, and their efficacy in improving exercise capacity and reducing pulmonary vascular resistance has been well-documented. However, potential side effects include headache, flushing, and visual disturbances.
- Endothelin Receptor Antagonists (ERAs): These drugs, such as bosentan and ambrisentan, block the action of endothelin, a potent vasoconstrictor. Their effectiveness in reducing pulmonary hypertension and improving survival has been demonstrated in clinical trials. Potential side effects include liver enzyme abnormalities, peripheral edema, and headaches.
- Prostanoids: These naturally occurring substances, like epoprostenol and treprostinil, are vasodilators that improve pulmonary blood flow. They are often reserved for more severe cases or when other treatments are ineffective. Prostanoids are usually administered intravenously or subcutaneously, leading to a higher frequency of administration. Side effects can include flushing, headache, and gastrointestinal issues.
- Guanylate Cyclase Stimulators: These medications, such as riociguat, promote vasodilation by increasing cyclic GMP levels. They have proven effective in lowering pulmonary artery pressure and improving exercise tolerance. Potential side effects include hypotension, dizziness, and headaches.
Procedural Therapies
In certain cases, procedural interventions may be necessary to improve PAH prognosis. These procedures aim to directly address the affected pulmonary vessels.
- Pulmonary Endarterectomy: This surgical procedure removes obstructions in the pulmonary arteries. It’s particularly effective for patients with inoperable thromboembolic disease and can significantly improve symptoms and exercise capacity. However, it carries surgical risks, including bleeding and infection. Post-operative care and rehabilitation are critical.
- Lung Transplantation: This is a complex procedure used in advanced cases when other therapies have failed. It offers the potential for a significant improvement in quality of life and survival. However, the procedure carries considerable risks, including organ rejection and the need for lifelong immunosuppression.
Combination Therapies
The use of combination therapies, combining different medications, can often lead to synergistic effects, improving treatment outcomes and reducing the risk of side effects.
Comparative Analysis
A comparative analysis of treatment modalities requires considering the efficacy and potential side effects of each approach. Factors such as the severity of PAH, the patient’s overall health, and individual response to therapy need to be evaluated. A detailed discussion with the physician is crucial for choosing the optimal treatment strategy. For example, in some patients, the combination of a PDE5 inhibitor with an ERA may yield better results than using either drug alone.
A doctor can determine the best approach based on the individual patient’s needs.
Long-Term Outcomes and Survival
Pulmonary arterial hypertension (PAH) is a progressive and often devastating disease, impacting the quality of life and ultimately, the lifespan of those affected. Understanding the long-term trajectory of this condition is crucial for patients, families, and healthcare providers alike. This section delves into the typical outcomes, the factors influencing survival, and the vital role of patient adherence and regular follow-ups in managing the disease.The long-term prognosis for PAH patients is unfortunately often challenging.
While advancements in treatment have significantly improved outcomes compared to previous decades, the disease’s relentless nature necessitates ongoing vigilance and proactive management. A key aspect of this management lies in understanding the factors that influence survival rates and how to effectively mitigate their impact.
Typical Long-Term Outcomes
PAH typically progresses over time, leading to a decline in lung function and ultimately, reduced ability to perform daily activities. This progression can manifest in various ways, including increasing shortness of breath, fatigue, and potentially, heart failure. The severity of these symptoms varies greatly among individuals, making accurate prediction of long-term outcomes difficult for any individual patient.
Factors Influencing Survival Rates
Several factors contribute to the variation in survival rates among PAH patients. These include the severity of the disease at diagnosis, the presence of co-morbidities (other health conditions), and the patient’s response to treatment. A key indicator of long-term outcome is the initial right ventricular dysfunction, as this often correlates with a faster disease progression. Age at diagnosis also plays a significant role.
Importance of Adherence to Treatment Plans
Adherence to prescribed treatment plans is paramount in influencing long-term prognosis for PAH patients. Consistent medication intake, as well as adhering to lifestyle recommendations (such as avoiding strenuous activity when advised) and following a healthy diet, can significantly improve outcomes. A patient’s understanding of the disease and their active participation in their care plan are essential components of this.
Role of Regular Follow-up Appointments
Regular follow-up appointments with healthcare providers are crucial for managing PAH and predicting prognosis. These appointments allow for monitoring of the disease’s progression, adjustments to treatment regimens, and early detection of potential complications. The frequency of these visits is often tailored to the individual patient’s needs and disease severity. Early intervention for worsening symptoms is vital.
Summary of Factors Affecting Long-Term Survival in PAH
| Factor | Impact on Survival |
|---|---|
| Disease Severity at Diagnosis | Higher severity at diagnosis often correlates with a shorter life expectancy. |
| Presence of Co-morbidities | Co-morbidities can negatively impact the patient’s overall health and reduce survival time. |
| Response to Treatment | Effective treatment response is crucial for prolonging life and improving quality of life. |
| Right Ventricular Dysfunction | Early and severe right ventricular dysfunction often indicates a faster disease progression. |
| Patient Adherence | Consistent adherence to treatment plans and lifestyle modifications is vital for better outcomes. |
| Regular Follow-up Appointments | Regular check-ups enable early detection of complications and adjustments to treatment, thus improving prognosis. |
Impact on Quality of Life
Living with pulmonary arterial hypertension (PAH) significantly impacts a patient’s overall quality of life. The progressive nature of the disease, coupled with the debilitating symptoms, creates numerous challenges that extend beyond the physical limitations. Patients experience a multifaceted decline in their ability to perform daily activities, impacting their emotional well-being and social interactions.Understanding the multifaceted effects of PAH on quality of life is crucial for developing effective support strategies and treatment plans.
This involves acknowledging the physical, psychological, and social dimensions of the patient experience. Recognizing these aspects enables healthcare professionals and caregivers to tailor interventions that address the holistic needs of PAH patients.
Physical Impact on Daily Activities
The progressive nature of PAH leads to a gradual decline in physical capacity. Symptoms such as shortness of breath, fatigue, and chest pain limit patients’ ability to perform routine tasks. Even simple activities like climbing stairs or walking short distances become strenuous or impossible. This restriction impacts their independence and social participation. Reduced physical activity often leads to muscle weakness and decreased overall fitness, further exacerbating the challenges.
This significantly impacts their ability to maintain employment, engage in hobbies, and participate in social activities.
Psychological and Emotional Effects
PAH can take a substantial toll on a patient’s psychological and emotional well-being. The fear of worsening symptoms, the uncertainty about the future, and the burden of chronic illness can lead to anxiety, depression, and feelings of isolation. The constant struggle to manage symptoms and adapt to limitations can create a sense of helplessness and frustration. Furthermore, the social stigma associated with chronic illness and the need for frequent medical appointments can lead to feelings of social isolation.
These emotional and psychological burdens are often overlooked but significantly impact the patient’s quality of life.
Social Impact
The limitations imposed by PAH can also impact social interactions and relationships. Patients may find it challenging to participate in social activities, maintain friendships, or pursue hobbies. The need for frequent medical appointments and the unpredictable nature of the disease can make it difficult to maintain a stable social life. It is vital to acknowledge the impact of PAH on social life, enabling healthcare providers to offer support and resources that facilitate social interaction and connection.
Strategies to Improve Quality of Life
Improving the quality of life for PAH patients necessitates a multi-faceted approach. This includes not only medical treatment but also psychological support, social engagement, and practical assistance. Providing access to support groups, counseling, and educational resources can help patients cope with the emotional and psychological aspects of the disease. Furthermore, encouraging physical activity tailored to the patient’s capabilities can help maintain strength and stamina.
Practical support, such as assistance with daily tasks, can significantly reduce the burden of the disease and improve overall well-being. Moreover, fostering a supportive environment within the healthcare system and the patient’s social circle is essential.
Impact on Quality of Life – Table Summary
| Aspect of Quality of Life | Impact of PAH |
|---|---|
| Physical Function | Reduced exercise tolerance, fatigue, shortness of breath, difficulty with daily activities. |
| Psychological Well-being | Anxiety, depression, fear of progression, social isolation. |
| Social Functioning | Difficulty participating in social activities, reduced social interaction, potential for isolation. |
| Emotional State | Helplessness, frustration, loss of independence. |
| Financial Burden | Potential for increased healthcare costs, lost income due to reduced work capacity. |
Research and Future Directions

Pulmonary arterial hypertension (PAH) remains a challenging disease, despite advancements in treatment. Ongoing research is crucial to refine diagnostic tools, uncover novel therapeutic targets, and ultimately improve long-term outcomes for patients. This section explores current research efforts, potential future therapies, and the vital role of clinical trials in shaping the future of PAH management.
Ongoing Research Efforts
Researchers are actively investigating the intricate molecular mechanisms underlying PAH pathogenesis. This includes studies focusing on the cellular and genetic factors that contribute to the development and progression of the disease. Understanding these fundamental processes is essential for developing more effective treatments and preventative strategies. For example, research into the role of specific gene mutations in PAH subtypes has led to a better understanding of disease heterogeneity, potentially enabling more personalized treatment approaches.
Potential of New Therapeutic Approaches
Emerging therapeutic strategies hold significant promise for improving PAH prognosis. These include novel therapies targeting specific signaling pathways implicated in vascular remodeling and inflammation within the pulmonary vasculature. Research is also exploring the use of targeted therapies that specifically inhibit the growth and proliferation of vascular smooth muscle cells, a key factor in PAH-induced pulmonary hypertension. One example of a promising approach is the development of drugs that block the action of specific enzymes or receptors known to play a critical role in PAH progression.
Importance of Clinical Trials
Clinical trials are essential for evaluating the efficacy and safety of new PAH treatments. These trials rigorously assess the impact of new drugs and therapeutic strategies on various clinical outcomes, including survival, symptom improvement, and quality of life. The results of well-designed clinical trials provide crucial data for regulatory agencies to approve new treatments, ultimately benefiting patients. For example, a successful clinical trial demonstrating the efficacy of a novel drug in reducing pulmonary vascular resistance could significantly impact the prognosis for PAH patients.
Current Knowledge Gaps in PAH Prognosis
Despite significant progress, several knowledge gaps persist in our understanding of PAH prognosis. One area requiring further investigation is the identification of biomarkers that can accurately predict disease progression and response to treatment. Another critical gap lies in developing more effective strategies for preventing disease progression, particularly in early-stage PAH. Finally, there is a need to understand the diverse responses of patients to existing and emerging therapies.
This will facilitate the development of more personalized treatment approaches.
Potential Avenues for Future Research
Future research should focus on developing non-invasive diagnostic tools for early detection and monitoring of PAH. This includes exploring new blood-based biomarkers that could detect PAH in its early stages, potentially enabling earlier intervention and improved outcomes. Another important area for research is the development of novel therapies targeting specific cellular pathways in the lung that drive disease progression.
This includes exploring innovative combinations of existing and new treatments. Further investigation into the role of the immune system in PAH pathogenesis may reveal new therapeutic targets. Ultimately, research should prioritize the development of personalized treatment approaches tailored to individual patient characteristics and disease progression.
Epilogue
In conclusion, pulmonary arterial hypertension prognosis is a multifaceted concept, influenced by a complex interplay of factors. From the initial diagnosis and treatment choices to the long-term outlook and impact on quality of life, a personalized approach is paramount. Ongoing research holds promise for further advancements in treatment and improved outcomes for individuals affected by this challenging condition.