Qa whats new in research for alzheimers diagnostics treatments – QA: What’s new in research for Alzheimer’s diagnostics and treatments? This exploration dives deep into the groundbreaking advancements in understanding, diagnosing, and treating this devastating disease. We’ll examine recent breakthroughs in biomarker discovery, novel imaging techniques, and innovative treatment strategies, while also addressing the significant challenges and ethical considerations that accompany these advancements. Prepare to be amazed by the progress and inspired by the potential for a brighter future for those affected by Alzheimer’s.
From understanding the progression of Alzheimer’s, to the limitations of current diagnostic tools, and the evolution of treatment approaches, this comprehensive overview provides a clear picture of the current landscape. We’ll analyze emerging research, explore promising new drugs and therapies, and discuss the potential societal and economic impact of these developments. We’ll look at specific examples of diagnostic tools and treatment approaches, examining their mechanisms of action and potential applications.
Finally, we’ll consider the future directions of research and the challenges that lie ahead.
Introduction to Alzheimer’s Diagnostics and Treatments
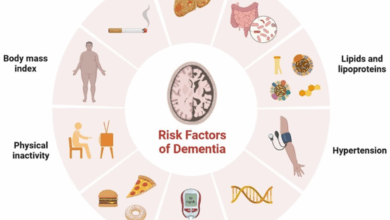
Alzheimer’s disease is a progressive neurodegenerative disorder that gradually erodes cognitive function, impacting memory, thinking, and behavior. The disease typically begins with subtle memory problems and progresses to severe impairment in daily functioning. This gradual decline significantly impacts individuals and their families, creating substantial challenges for both personal and societal well-being.The current understanding of Alzheimer’s emphasizes the accumulation of abnormal protein aggregates (amyloid plaques and tau tangles) in the brain, leading to neuronal damage and loss.
This process contributes to the characteristic symptoms observed in patients. While the precise mechanisms remain a subject of active research, the accumulating evidence highlights the critical role of these protein abnormalities in the disease’s progression.
Current Landscape of Alzheimer’s Diagnostics
Accurate and early diagnosis of Alzheimer’s disease remains a significant challenge. While several methods exist, they often exhibit limitations in terms of sensitivity, specificity, and invasiveness. Early detection is crucial for timely intervention and management strategies, yet existing tools are not always sufficient to meet this need.
- Neuropsychological testing assesses cognitive function. These tests evaluate memory, language, problem-solving, and other cognitive domains. However, these assessments may not always be sensitive enough to detect subtle cognitive changes in the very early stages of the disease.
- Neuroimaging techniques, like MRI and PET scans, provide structural and functional insights into the brain. Amyloid PET scans can detect amyloid plaques, while structural MRI can reveal brain atrophy. Despite advancements, these techniques are not always conclusive and can sometimes exhibit false positives or negatives.
- Cerebrospinal fluid (CSF) analysis can detect biomarkers like amyloid and tau proteins. Elevated levels of certain proteins in CSF can be indicative of Alzheimer’s disease, but these tests are invasive and not always readily available.
Evolution of Treatment Approaches
Treatment for Alzheimer’s disease has evolved from primarily addressing the symptoms to exploring potential disease-modifying therapies. Early interventions focused on managing symptoms like memory loss, behavioral changes, and mood disturbances. However, recent research has yielded promising leads in therapies that aim to slow or halt the progression of the disease itself.
- Symptomatic therapies, such as cholinesterase inhibitors and memantine, aim to improve cognitive function and manage symptoms. These drugs can provide some relief from cognitive decline but do not alter the underlying disease process.
- Disease-modifying therapies are currently under development and testing. These therapies target the pathological mechanisms driving Alzheimer’s, including amyloid plaque reduction and tau tangle formation. Results from clinical trials are being closely monitored to evaluate their efficacy and safety.
Comparison of Diagnostic Methods
The table below summarizes the strengths and weaknesses of different diagnostic methods for Alzheimer’s disease.
Recent breakthroughs in Alzheimer’s research are incredibly exciting, focusing on new diagnostic tools and potential treatments. While the world watches closely for what happens after the omicron wave passes, it’s important to remember that these advancements in Alzheimer’s care are ongoing and will continue to shape our future understanding and management of this debilitating disease. The future of Alzheimer’s research is promising, and we’ll continue to see important developments in the coming years.
what happens after the omicron wave passes is a fascinating topic in itself, but it’s not directly related to the advancements in Alzheimer’s diagnostics and treatments.
| Diagnostic Method | Strengths | Weaknesses |
|---|---|---|
| Neuropsychological Testing | Relatively non-invasive, readily available | Limited sensitivity in early stages, subjective interpretation |
| Neuroimaging (MRI/PET) | Provides structural and functional information, detects amyloid plaques | Can be expensive, may not always provide definitive diagnosis |
| CSF Analysis | Can detect biomarkers like amyloid and tau | Invasive procedure, not always readily available, false positives/negatives |
Recent Research Advancements in Diagnostics
Unveiling the secrets of Alzheimer’s disease hinges on accurate and early diagnosis. Recent research has yielded exciting breakthroughs in identifying biomarkers, imaging techniques, and genetic markers, offering a glimpse into the complex processes driving this devastating condition. These advancements hold the promise of earlier detection and personalized treatment strategies.
Biomarker Discovery for Early Detection
Early detection is crucial for effective Alzheimer’s intervention. Recent research has focused intensely on identifying reliable biomarkers, measurable indicators of the disease’s presence and progression. These biomarkers can be found in various biological samples, including cerebrospinal fluid (CSF), blood, and even saliva. The discovery of specific proteins, peptides, and other molecules associated with Alzheimer’s pathology is revolutionizing the field.
Amyloid-beta and tau protein levels are prime examples of biomarkers under scrutiny, their abnormal accumulation serving as key indicators of disease progression. Moreover, studies are exploring the potential of novel biomarkers, potentially offering even earlier and more accurate detection than current methods.
Novel Imaging Techniques for Brain Visualization
Advanced imaging techniques are providing invaluable insights into the structural and functional changes in the brains of individuals with Alzheimer’s. Positron emission tomography (PET) scans, coupled with specific tracers, are revealing the accumulation of amyloid-beta plaques and tau tangles in the brain. These scans offer a detailed view of the disease’s spread and progression, aiding in diagnosis and monitoring treatment efficacy.
Magnetic resonance imaging (MRI) techniques, with their enhanced resolution and sensitivity, are increasingly important in identifying subtle structural changes indicative of Alzheimer’s, including atrophy in specific brain regions. Diffusion tensor imaging (DTI), another MRI variant, can provide information about the integrity of white matter tracts in the brain, further enriching our understanding of the disease’s impact on brain connectivity.
Genetic and Proteomic Approaches for Improved Diagnostics
Genetic predispositions play a significant role in Alzheimer’s development. Researchers are exploring the intricate relationship between specific genes and the disease, seeking to identify genetic markers associated with an increased risk or progression rate. Genome-wide association studies (GWAS) are unraveling the genetic landscape of Alzheimer’s, pinpointing potential genetic variations linked to the disease. Proteomics, the study of proteins, is also being utilized to identify protein abnormalities associated with Alzheimer’s, adding another layer of complexity to our understanding of the disease’s mechanisms.
This approach, by analyzing the full complement of proteins in biological samples, promises to uncover new diagnostic markers and insights into disease pathogenesis.
Recent research on Alzheimer’s diagnostics and treatments is fascinating. While exploring new avenues for early detection and effective therapies, I’ve also been drawn to the potential of meditation techniques for managing other health challenges, like binge eating disorder. This approach, as detailed in meditation for binge eating disorder , might offer valuable insights into stress reduction and emotional regulation, which could surprisingly complement the ongoing quest for Alzheimer’s solutions.
Ultimately, it all boils down to finding holistic approaches to improve well-being in various aspects of health.
Summary of Biomarker-Based Diagnostic Methods
| Biomarker-Based Diagnostic Method | Advantages | Disadvantages |
|---|---|---|
| Amyloid-beta PET scans | High sensitivity for detecting amyloid plaques; relatively non-invasive | Costly; potential for false positives; not indicative of all aspects of Alzheimer’s |
| Tau PET scans | Can detect tau tangles; complementary to amyloid-beta scans | Limited availability; cost; can be affected by other neurodegenerative diseases |
| CSF analysis | Provides direct measure of proteins in the brain; can offer insights into disease progression | Invasive procedure; potential for complications; requires specialized labs |
| Blood tests | Non-invasive; relatively inexpensive; can be used for large-scale screening | May have lower sensitivity compared to other methods; need for validation in diverse populations |
Innovations in Treatment Strategies
The quest for effective Alzheimer’s treatments extends beyond simply diagnosing the disease. Current therapies primarily focus on managing symptoms, but research is actively exploring new avenues to address the underlying causes and potentially slow or halt disease progression. This involves novel drug candidates and innovative therapeutic approaches. Understanding these advancements is crucial for potential future patient care and improving the lives of those affected by Alzheimer’s.
New Drug Candidates and Clinical Trials
Several promising drug candidates are currently undergoing clinical trials, targeting various aspects of Alzheimer’s pathology. These include medications aiming to reduce amyloid plaques and tau tangles, which are hallmarks of the disease, as well as therapies that enhance neuronal communication and protect brain cells from damage. For example, some trials are evaluating drugs that target specific enzymes involved in amyloid production, potentially preventing or reducing plaque accumulation.
Recent research on Alzheimer’s diagnostics and treatments is super exciting. Scientists are exploring new blood tests and imaging techniques to detect the disease earlier, potentially even before symptoms appear. While focusing on those breakthroughs, it’s also important to consider lifestyle factors that can contribute to overall well-being, like incorporating regular exercise into your routine. For example, walking is a fantastic way to ease menopause symptoms, as detailed in this helpful guide: ways to ease menopause symptoms with walking.
Ultimately, a holistic approach, including proactive research and healthy habits, is key to potentially combating Alzheimer’s.
Others are exploring therapies that enhance the clearance of amyloid plaques from the brain.
Promising Therapeutic Strategies Beyond Current Medications
Beyond conventional drug therapies, researchers are exploring innovative approaches. These include gene therapies, which could potentially modify the genetic predisposition to Alzheimer’s, and stem cell therapies, aimed at replacing damaged brain cells. Also, non-pharmacological interventions, like lifestyle modifications and cognitive training, are being investigated for their potential to mitigate disease progression and improve cognitive function. These non-pharmacological approaches can be particularly valuable for individuals in the early stages of the disease, and may prove to be crucial in combination with pharmacological therapies.
Comparison of Treatment Approaches for Different Stages
Treatment strategies should be tailored to the specific stage of Alzheimer’s disease. Early-stage interventions, focusing on lifestyle modifications, cognitive stimulation, and medication to preserve cognitive function, may prove more effective than treating advanced stages. In the middle stages, managing behavioral and psychological symptoms becomes a crucial aspect of care. In the later stages, care shifts towards comfort and support for both the patient and their caregivers.
Table of Alzheimer’s Disease Stages and Corresponding Treatment Options
| Stage of Alzheimer’s Disease | Description | Treatment Options |
|---|---|---|
| Early Stage | Mild cognitive decline, noticeable memory problems, difficulty performing complex tasks. | Lifestyle modifications (diet, exercise, social engagement), cognitive training, medications to preserve cognitive function. |
| Middle Stage | Increased cognitive decline, significant memory loss, difficulty with daily tasks, behavioral and psychological symptoms may emerge. | Medication to manage behavioral and psychological symptoms, support groups, home care, and potentially medications to maintain cognitive function. |
| Late Stage | Severe cognitive decline, inability to perform daily tasks, loss of communication and motor skills. | Comfort care, palliative care, and support for caregivers. Medications are often used to manage symptoms, such as agitation and wandering. |
Challenges and Future Directions
The journey toward effective Alzheimer’s diagnostics and treatments faces significant hurdles. While recent research offers promising glimpses, translating these advancements into widespread clinical use requires overcoming substantial obstacles. The complexity of the disease, coupled with the multifaceted nature of its progression, necessitates a multifaceted approach to research and development.The current state of research reveals a complex interplay of factors contributing to the challenges.
The multifaceted nature of the disease, spanning various biological pathways and brain regions, presents a formidable obstacle to creating targeted interventions. Early detection remains elusive, often requiring advanced imaging techniques or invasive procedures, leading to difficulties in widespread implementation. Furthermore, the heterogeneity of Alzheimer’s, where different individuals may experience varying symptoms and disease progression, poses a significant challenge for developing therapies with universal efficacy.
Challenges Hindering Development and Implementation, Qa whats new in research for alzheimers diagnostics treatments
Several obstacles hinder the development and implementation of effective Alzheimer’s diagnostics and treatments. These include the lack of reliable biomarkers for early detection, the complexity of the disease mechanisms, and the challenges in translating research findings into clinical practice. The significant financial investment required for large-scale clinical trials also contributes to the challenge.
- Biomarker Limitations: Current diagnostic tools often lack the sensitivity and specificity required for early and accurate detection. This limitation hinders the identification of individuals at risk and hampers the development of personalized treatment strategies.
- Disease Complexity: The intricate interplay of genetic, environmental, and lifestyle factors contributing to Alzheimer’s pathogenesis makes it challenging to pinpoint the critical mechanisms responsible for disease progression. This complexity poses a hurdle to the development of effective treatments that target specific pathways.
- Translation Gap: Moving research findings from the laboratory to clinical settings often faces obstacles. The high cost and time-consuming nature of clinical trials, coupled with the need for robust data validation, frequently slows down the translation process.
- Financial Constraints: Significant financial resources are required for large-scale clinical trials, potentially deterring research efforts and delaying the development of new treatments.
Ethical Considerations
New diagnostic tools and therapies raise important ethical considerations. Ensuring equitable access to these advancements, minimizing potential biases in research and clinical practice, and addressing the potential for misdiagnosis are crucial.
- Equity of Access: The high cost of advanced diagnostic tools and therapies could create disparities in access, potentially exacerbating existing health inequities. Strategies for ensuring equitable access are critical for maximizing the impact of new interventions.
- Bias Mitigation: Research and clinical trials should actively address potential biases in participant selection and data interpretation. The use of diverse populations in research is essential to ensure the development of treatments that are effective for a broad range of individuals.
- Minimizing Misdiagnosis: The development of robust diagnostic criteria and standardized protocols is essential to minimize the risk of misdiagnosis, particularly in cases where symptoms overlap with other neurological conditions. This requires a multidisciplinary approach to diagnosis, incorporating a range of perspectives and expertise.
Promising Research Areas for Prevention and Cure
Future research should focus on preventative strategies and potentially curative therapies. These strategies should incorporate lifestyle modifications, targeted therapies, and regenerative approaches. The development of personalized medicine approaches, tailored to individual genetic profiles and risk factors, is a key area of focus.
- Lifestyle Interventions: Research should focus on identifying and implementing lifestyle interventions that can mitigate the risk of developing Alzheimer’s disease, such as dietary modifications, exercise regimens, and cognitive stimulation activities.
- Targeted Therapies: The identification of specific molecular targets and the development of therapies that can effectively modulate these targets is crucial for the development of effective treatments.
- Regenerative Medicine: Approaches that focus on stimulating the regeneration of damaged brain cells or replacing them with healthy ones could potentially offer a curative approach. This area requires extensive research to address the challenges of cell transplantation and regeneration in the central nervous system.
- Personalized Medicine: The development of personalized treatments based on an individual’s genetic profile and risk factors holds great promise. This approach can lead to more effective and targeted therapies.
Key Areas for Further Research
| Research Area | Specific Focus |
|---|---|
| Early Detection | Development of sensitive and specific biomarkers for early detection, including blood-based tests and advanced neuroimaging techniques. |
| Disease Mechanisms | Identification of key molecular pathways involved in Alzheimer’s pathogenesis and development of novel therapeutic targets. |
| Treatment Strategies | Development of effective therapies that can slow or halt disease progression, including those targeting amyloid plaques, tau tangles, and neuroinflammation. |
| Prevention Strategies | Identification of modifiable risk factors and development of interventions that can reduce the incidence of Alzheimer’s disease, such as lifestyle modifications and cognitive training programs. |
| Ethical Considerations | Establishment of ethical guidelines and frameworks for the development, implementation, and use of new diagnostic tools and therapies. |
Illustrative Examples of Diagnostic Tools
Unveiling the secrets of Alzheimer’s often hinges on precise diagnostic tools. These tools, ranging from advanced imaging techniques to sophisticated biomarker analysis, offer crucial insights into the disease’s progression and potential for early detection. The quest for effective diagnostic tools is paramount, paving the way for timely interventions and improved patient outcomes.
Amyloid PET Scans
Amyloid PET scans, a cutting-edge imaging technology, play a vital role in detecting amyloid plaques in the brain. These plaques are a hallmark of Alzheimer’s disease and their presence correlates with the disease’s progression. The technique leverages a radioactive tracer that binds to amyloid proteins, allowing specialized equipment to visualize these protein aggregates in the brain. The scan provides a detailed image of amyloid deposition, helping clinicians differentiate Alzheimer’s from other neurodegenerative conditions.
Tau PET Imaging
Tau PET imaging is another valuable tool in Alzheimer’s diagnostics. This technique focuses on visualizing tau tangles, another crucial protein implicated in the disease’s pathology. Similar to amyloid PET scans, a radioactive tracer is used, but this tracer binds specifically to tau proteins. The resulting images reveal the distribution and density of tau tangles, offering a deeper understanding of the disease’s neurodegenerative process.
The combination of amyloid and tau PET imaging can provide a more comprehensive assessment of Alzheimer’s disease.
Cerebrospinal Fluid (CSF) Biomarker Analysis
Cerebrospinal fluid (CSF) contains a wealth of information about the brain’s health. Analysis of CSF can reveal the presence of specific biomarkers that reflect the disease’s progression. For instance, reduced levels of amyloid-beta peptides or increased levels of phosphorylated tau protein in CSF can be indicative of Alzheimer’s. This analysis provides a valuable liquid biopsy, complementing imaging techniques and aiding in diagnosis, especially in cases where imaging results are inconclusive.
Genetic Analysis for Early Detection
Genetic predispositions play a significant role in Alzheimer’s development. Specific genetic variations, such as mutations in the APOE gene, can increase an individual’s risk of developing the disease. Genetic testing can identify these variations, allowing for early identification of individuals at higher risk. While not a definitive diagnosis, genetic analysis can be a valuable tool in risk assessment, prompting proactive lifestyle adjustments and enabling earlier monitoring.
It’s important to remember that genetic predisposition doesn’t guarantee disease development, and other factors also contribute to the condition.
Illustrative Examples of Treatment Approaches: Qa Whats New In Research For Alzheimers Diagnostics Treatments
The quest for effective Alzheimer’s treatments is multifaceted, encompassing various approaches, from targeting underlying mechanisms to modifying lifestyle factors. This section explores promising strategies, including novel drug candidates, preventive measures, and personalized medicine techniques. These examples illustrate the diverse and evolving landscape of Alzheimer’s research.
Novel Drug Candidates in Clinical Trials
Several drug candidates are currently undergoing clinical trials, aiming to target specific molecular pathways implicated in Alzheimer’s disease. One such example involves a monoclonal antibody targeting amyloid-beta oligomers. These oligomers, smaller aggregates of amyloid-beta peptides, are believed to be particularly harmful, disrupting neuronal communication and contributing to cognitive decline. This antibody is designed to bind to and neutralize these harmful oligomers, potentially preventing their aggregation and reducing neuronal damage.
Early trial results suggest promise, though further studies are needed to confirm long-term efficacy and safety.
Promising Therapeutic Strategies for Preventing Amyloid Plaque Formation
Preventing the formation of amyloid plaques, a hallmark of Alzheimer’s, is a crucial target for preventative therapies. One promising strategy involves modulating the activity of enzymes involved in amyloid-beta production. Specific inhibitors are being developed to reduce the production of amyloid-beta peptides. If successful, these inhibitors could potentially halt the progression of the disease by preventing the accumulation of toxic amyloid plaques.
Lifestyle Interventions to Mitigate Alzheimer’s Risk
Lifestyle factors play a significant role in Alzheimer’s risk mitigation. Maintaining a healthy diet rich in fruits, vegetables, and omega-3 fatty acids, coupled with regular physical exercise, is linked to a lower risk of cognitive decline. Cognitive stimulation through activities like reading, learning new skills, and engaging in social interactions also appears to be beneficial. These lifestyle modifications are not a cure, but rather a preventative measure that may delay the onset or slow the progression of Alzheimer’s disease.
Personalized Medicine Approaches in Alzheimer’s Treatment
Personalized medicine aims to tailor treatments to individual patients based on their genetic makeup, lifestyle, and other factors. In the context of Alzheimer’s, this could involve identifying genetic markers associated with disease susceptibility and tailoring treatment strategies accordingly. For example, individuals with specific gene variants might benefit from particular drug therapies or lifestyle interventions more effectively than others.
This approach, while still in its early stages, holds great promise for improving treatment outcomes and reducing adverse effects.
Public Health Implications
The advancements in Alzheimer’s diagnostics and treatments hold immense promise for improving the lives of millions affected by this devastating disease. Beyond individual benefits, these breakthroughs offer significant public health implications, impacting society and economies worldwide. The potential for reducing the global burden of Alzheimer’s is substantial, and understanding these broader impacts is crucial for effective implementation and resource allocation.
Societal Impact of Improved Diagnostics and Treatments
Improved diagnostics lead to earlier detection, enabling timely interventions and support systems. This allows individuals to maintain independence and quality of life for longer periods, reducing the strain on caregivers and healthcare systems. Early intervention also facilitates the development of personalized treatment plans tailored to individual needs, maximizing the effectiveness of interventions. Furthermore, accurate diagnostics empower individuals and their families to make informed decisions about their future, including planning for care and support needs.
Economic Implications of Early Detection and Effective Treatment
Early detection allows for earlier interventions, potentially reducing the long-term care costs associated with Alzheimer’s. By delaying the onset of severe symptoms, effective treatments can lessen the financial burden on individuals, families, and healthcare systems. The economic benefits extend beyond direct healthcare costs. Reduced caregiving responsibilities can boost productivity in the workforce, as caregivers can return to work or maintain employment more easily.
Potential for Reducing the Global Burden of Alzheimer’s
The global burden of Alzheimer’s is substantial, impacting individuals, families, and healthcare systems. Improved diagnostics and treatments can significantly reduce this burden. For instance, earlier detection allows for timely interventions, potentially slowing disease progression and mitigating the severity of symptoms. This, in turn, reduces the long-term care needs of individuals, freeing up resources for other health priorities.
Additionally, a reduced burden on healthcare systems allows for increased investment in other critical areas of public health.
Summary of Economic and Societal Benefits
| Benefit Category | Description | Illustrative Example |
|---|---|---|
| Reduced Healthcare Costs | Early detection and treatment can lower the long-term costs associated with Alzheimer’s care, such as hospitalization, long-term care facilities, and medications. | A study in the US estimated that early intervention programs could save billions of dollars by reducing the need for intensive care and institutionalization. |
| Increased Productivity | Reduced caregiving responsibilities can enable caregivers to return to work, improving workforce participation and economic output. | Caregivers who are able to maintain employment due to effective treatments for Alzheimer’s contribute to the economy through their work and tax payments. |
| Improved Quality of Life | Early diagnosis and treatment allow individuals to maintain independence and quality of life for longer periods, reducing stress on caregivers and individuals. | Individuals with Alzheimer’s can continue to live independently in their homes for longer periods with effective interventions, maintaining their dignity and quality of life. |
| Reduced Burden on Caregivers | Effective treatments and support systems alleviate the emotional and financial strain on family caregivers. | Caregiver support groups and respite care services can help caregivers manage the demands of caring for a loved one with Alzheimer’s, allowing them to maintain their well-being. |
| Enhanced Social Participation | Improved quality of life allows individuals to maintain social connections and engagement in communities, reducing social isolation. | Community support programs and social activities can help individuals with Alzheimer’s maintain social connections and participation in their communities. |
Closing Summary
In conclusion, the research landscape surrounding Alzheimer’s diagnostics and treatments is rapidly evolving. Exciting breakthroughs in biomarker discovery, imaging techniques, and potential therapies offer hope for improved early detection and more effective interventions. However, significant challenges remain, including ethical considerations and the need for further research. The future holds immense potential, and continued advancements in this field are crucial for improving the lives of those affected by this debilitating disease.
This exploration offers a glimpse into the exciting and complex world of Alzheimer’s research, highlighting the importance of ongoing efforts to find better diagnostics and treatments.