
Quality of diet for older adults has declined heres how to fix it – Quality of diet for older adults has declined, here’s how to fix it. This isn’t just about eating well; it’s about maintaining health, energy, and overall well-being in later life. Changing dietary habits is possible, and this guide will explore the factors behind this decline, highlight the specific nutritional needs of older adults, and provide actionable steps to create a healthier and happier aging experience.
The decline in dietary quality among older adults is a multifaceted issue. From shifting cultural norms to the impact of socioeconomic factors, several elements contribute to poor nutrition in this demographic. Understanding these factors is the first step towards effective interventions. This guide also delves into the crucial role of personalized dietary advice and practical strategies for navigating meal planning, preparation, and access to healthy foods.
The consequences of poor nutrition, from physical health issues to cognitive decline, are substantial and underscore the urgency of this topic.
Understanding the Decline
The quality of diet among older adults has seen a concerning decline in recent decades. This shift is multifaceted, influenced by a complex interplay of societal changes, evolving lifestyles, and individual circumstances. Understanding the reasons behind this decline is crucial for developing effective strategies to improve nutritional well-being in this demographic.The dietary landscape of older adults has undergone significant transformations.
Historically, dietary habits were often shaped by readily available, locally sourced foods, and traditional cooking methods. However, globalization, industrialization, and changing economic conditions have led to greater access to processed foods, fast food, and restaurant meals, often with lower nutritional value. This shift in food choices has contributed to a noticeable decline in the overall quality of diets for older adults.
Historical Dietary Habits and Shifts
Older generations often adhered to dietary traditions passed down through families and communities. These traditions, while sometimes limited in variety, typically emphasized whole foods, locally sourced produce, and home-cooked meals. The prevalence of processed foods and convenience options has increased dramatically, particularly in the last few decades. This has contributed to a shift away from traditional, healthier eating patterns.
Prevalence of Poor Nutrition
Undernutrition, micronutrient deficiencies, and overconsumption of unhealthy foods are significant concerns among older adults. Studies have shown that a substantial percentage of older adults suffer from inadequate intake of essential vitamins and minerals. For instance, vitamin D and B12 deficiencies are prevalent, potentially impacting bone health and cognitive function. Simultaneously, overconsumption of saturated fats, sodium, and added sugars is also widespread, contributing to the rise in chronic diseases like heart disease and diabetes.
These issues are not isolated to specific demographics, but are common across a wide range of older adult populations.
Contributing Factors to the Decline
Several factors contribute to the decline in dietary quality among older adults. Socioeconomic factors play a crucial role. Lower income can limit access to fresh produce and nutrient-rich foods, often forcing individuals to rely on more affordable, less nutritious options. Limited access to grocery stores or transportation can further exacerbate these challenges. Cultural norms and preferences also influence food choices.
Traditional dishes or dietary habits may not always align with current dietary recommendations, potentially leading to inadequate nutrient intake. Health conditions, such as loss of appetite, difficulty chewing, or swallowing problems, can further restrict food choices and nutrient intake. Moreover, medications can sometimes affect appetite or nutrient absorption.
Consequences of Poor Nutrition
The consequences of poor nutrition in older adults are significant and far-reaching. Physical health impacts can include weakened immune systems, slower wound healing, decreased muscle mass, and increased susceptibility to infections. Cognitive decline, including impaired memory and reduced mental sharpness, is also linked to inadequate nutrient intake. Poor nutrition is strongly associated with an increased risk of chronic diseases like heart disease, stroke, type 2 diabetes, and certain types of cancer.
These negative outcomes underscore the importance of addressing dietary quality issues in older adults.
Identifying Nutritional Needs
Understanding the nutritional needs of older adults is crucial for maintaining their health and well-being. As we age, our bodies undergo various changes, impacting how we process nutrients and utilize energy. This necessitates a tailored approach to nutrition that acknowledges these shifts and provides the specific support older adults require. This section dives deep into the specific nutritional needs of this demographic, comparing and contrasting needs across different age groups and highlighting the importance of key nutrients.Older adults face unique challenges in maintaining optimal nutrition.
Changes in metabolism, nutrient absorption, and overall health status can significantly impact the body’s ability to obtain and utilize essential nutrients. Furthermore, factors like decreased appetite, dental issues, and socioeconomic circumstances can further complicate dietary adherence.
Specific Nutritional Requirements of Older Adults
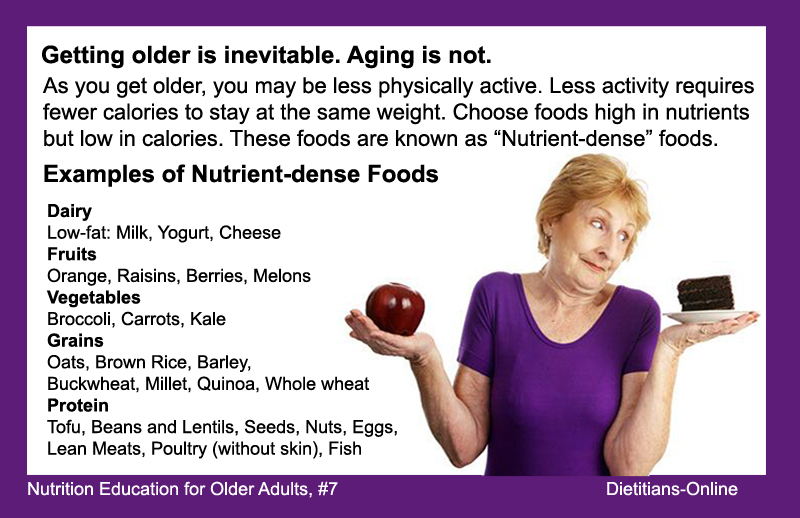
Older adults have different nutritional requirements compared to younger adults due to shifts in metabolism and absorption. Nutrient absorption often slows down, leading to a need for increased intake of certain vitamins and minerals to maintain optimal levels. Furthermore, muscle mass tends to decrease with age (sarcopenia), requiring a higher protein intake to maintain strength and function. Calorie needs also generally decrease, but this reduction should be carefully managed, considering individual activity levels and health conditions.
Comparison of Nutritional Needs Across Different Age Groups Within Older Adults
The nutritional needs of older adults are not uniform across all age groups. For instance, individuals in their 60s may have different requirements compared to those in their 80s or 90s. Those in their 60s may still be relatively active and have better digestive systems, allowing for a wider range of nutrient intake. Conversely, individuals in their 80s and 90s may experience significant declines in digestive function, affecting nutrient absorption.
Consequently, a tailored dietary approach for each specific age group within the older adult population is essential.
Importance of Key Nutrients
Protein plays a vital role in maintaining muscle mass, strength, and overall health. Adequate protein intake is crucial to combat age-related muscle loss (sarcopenia) and support recovery from injuries or illnesses. Vitamins and minerals are also essential for maintaining various bodily functions. For example, vitamin D is crucial for calcium absorption, which is vital for bone health, and vitamin B12 is essential for nerve function and red blood cell production, both of which can be affected by age-related changes.
The appropriate levels of these nutrients vary depending on individual needs and health conditions.
It’s concerning that the quality of diet for older adults has declined. One crucial aspect to consider is food safety. Understanding how government agencies like the FDA ensure food safety, through rigorous food safety government inspection procedures, is vital. This helps maintain the safety and nutritional value of food, which is paramount in creating a healthy diet for seniors.
Ultimately, focusing on safe, nutritious food choices is key to improving the diets of older adults.
Dietary Patterns for Optimal Nutrition in Older Adults
A balanced and varied diet is paramount for older adults. This involves incorporating a wide range of nutrient-rich foods, including fruits, vegetables, lean proteins, whole grains, and low-fat dairy products. Examples of dietary patterns that support optimal nutrition include the Mediterranean diet, which emphasizes fruits, vegetables, whole grains, and healthy fats, and the DASH (Dietary Approaches to Stop Hypertension) diet, which focuses on reducing sodium intake while increasing intake of potassium-rich foods.
The specific dietary pattern chosen should be tailored to the individual’s preferences, health conditions, and overall nutritional needs. Regular consultation with a registered dietitian or healthcare professional can provide personalized recommendations.
Examples of Specific Dietary Recommendations
Daily protein intake should be adjusted based on individual needs, aiming for 1.2-1.5 grams of protein per kilogram of body weight.
- Incorporate a variety of colorful fruits and vegetables to ensure a diverse intake of vitamins, minerals, and antioxidants.
- Prioritize lean protein sources, such as fish, poultry, beans, and lentils, to support muscle maintenance.
- Choose whole grains over refined grains to obtain essential fiber, which is important for digestive health.
- Limit processed foods, sugary drinks, and excessive sodium intake.
Improving Dietary Quality
Nourishing older adults requires a multifaceted approach that goes beyond simply providing food. A focus on accessibility, practicality, and individualized needs is crucial for maintaining optimal health and well-being in this demographic. This section delves into practical strategies for improving dietary quality, addressing specific challenges faced by older adults.Addressing the nutritional needs of older adults requires a proactive and adaptable approach.
Simple modifications to existing meal plans can significantly enhance nutritional intake, promoting overall health and well-being.
Improving Access to Healthy, Affordable Food Options
Access to nutritious and affordable food is a significant challenge for many older adults, particularly those living in food deserts or experiencing poverty. Strategies to enhance access include partnerships with community organizations, farmers’ markets, and local food banks. Supporting initiatives that provide transportation assistance to grocery stores can also be a vital component. Financial assistance programs, such as senior nutrition programs, can further bridge the gap and ensure equitable access to healthy food options.
Practical Tips for Incorporating Healthy Foods
A key aspect of improving dietary quality is integrating more fruits, vegetables, lean proteins, and whole grains into daily routines. This section Artikels actionable strategies for achieving this goal.
- Increased fruit and vegetable consumption: Start by adding a serving of fruit or vegetables to each meal. Include a variety of colors to ensure a broader range of nutrients. Consider incorporating them into smoothies, salads, or as a side dish. For example, a simple side salad with a light vinaigrette dressing can add a variety of vegetables to a meal, while a smoothie can combine fruits and vegetables for a quick and nutritious breakfast or snack.
- Lean protein sources: Choose lean protein sources like poultry, fish, beans, lentils, and tofu. These options are often more affordable and can be easily incorporated into various meals. For instance, adding beans to chili or lentil soup adds protein and fiber, while baked fish can be a healthy and delicious weeknight meal.
- Whole grains: Opt for whole-grain bread, pasta, and cereals over refined options. Whole grains provide essential fiber, which aids digestion and helps regulate blood sugar levels. For example, swapping white bread for whole-wheat bread can significantly increase fiber intake, and using brown rice instead of white rice adds a valuable source of fiber and nutrients.
Meal Planning and Preparation for Older Adults
Meal planning and preparation can become challenging for older adults with limited mobility or cognitive decline. Strategies for addressing these challenges include simplifying recipes, using pre-cut vegetables and pre-cooked ingredients, and utilizing meal delivery services or meal kits.
Adapting Recipes for Specific Needs
Adapting recipes to meet individual dietary needs and preferences is vital. This includes accommodating allergies, intolerances, and cultural considerations. Substituting ingredients, adjusting portion sizes, and exploring diverse cooking methods can ensure that everyone can enjoy nutritious meals.
Addressing Barriers and Support Systems
Improving dietary quality for older adults isn’t just about knowing what to eat; it’s about navigating the practical realities that often stand in the way. Many factors influence food choices, and understanding these barriers is crucial to creating effective support systems. From financial constraints to cultural preferences, overcoming these obstacles is key to promoting healthy eating habits.Addressing the challenges older adults face in adopting healthier diets requires a multifaceted approach.
This includes identifying the specific barriers encountered by individuals, offering practical solutions, and fostering supportive environments that empower them to make positive changes. Ultimately, personalized support is essential to help older adults achieve and maintain healthy dietary habits.
Potential Barriers to Healthy Eating
Many factors can hinder older adults from adopting healthier diets. Financial limitations, limited access to nutritious foods, and cultural influences all play a role.
- Cost: Fresh produce and lean protein can be expensive, making it challenging for those on fixed incomes to maintain a healthy diet. For example, a senior on a limited budget might opt for cheaper, less nutritious processed foods due to their affordability.
- Access: Lack of access to grocery stores, farmers’ markets, or healthy food options in a community can make it difficult to obtain fresh produce and other healthy foods. This can be particularly true for seniors living in rural areas or those with mobility limitations.
- Cultural Influences: Traditional dietary habits and cultural norms often influence food choices. Breaking away from established patterns can be difficult, requiring a thoughtful approach to dietary changes that respects cultural preferences.
- Physical Limitations: Conditions like arthritis or limited mobility can make grocery shopping and meal preparation more challenging. Seniors with these conditions may need assistance with meal preparation or transportation to obtain healthy foods.
- Knowledge and Skills: Some older adults may lack the knowledge or skills to prepare healthy meals or understand nutrition labels. This could lead to poor food choices and hinder the adoption of healthier dietary habits.
Support Systems and Resources
Fortunately, a range of support systems and resources are available to assist older adults in making positive dietary changes.
- Healthcare Professionals: Doctors, registered dietitians, and other healthcare professionals can provide personalized dietary advice, conduct assessments, and create tailored meal plans. They can also address any underlying health conditions that may impact dietary choices.
- Family and Friends: Family members and friends can play a significant role in supporting dietary changes. They can offer encouragement, help with meal preparation, and provide transportation to grocery stores. Sharing healthy recipes and participating in meals together can foster positive dietary habits.
- Community Organizations: Local senior centers, community gardens, and nutrition programs often provide resources and support to older adults. These organizations can offer cooking classes, nutrition education workshops, and access to healthy food options.
- Government Programs: Programs like SNAP (Supplemental Nutrition Assistance Program) and Meals on Wheels provide vital support for older adults struggling with food insecurity. These programs can help ensure access to nutritious foods and reduce financial barriers to healthy eating.
Importance of Personalized Dietary Advice
Personalized dietary advice is crucial for older adults due to the diverse range of needs and circumstances. A one-size-fits-all approach may not be effective, and individual assessments are necessary to tailor recommendations to specific situations.
- Individual Assessments: A healthcare professional should assess an individual’s medical history, dietary preferences, and lifestyle to create a personalized dietary plan. This approach considers individual needs, potential allergies or sensitivities, and existing health conditions.
- Tailored Meal Plans: Personalized meal plans can incorporate the individual’s preferences while meeting their nutritional needs. These plans should be flexible and adaptable to changes in lifestyle or health conditions.
- Monitoring Progress: Regular monitoring of progress and adjustments to the dietary plan as needed are vital to ensure that the plan remains effective and meets the individual’s evolving needs.
Promoting Healthy Eating Habits
Encouraging healthy eating habits in older adults is crucial for maintaining their well-being and quality of life. This involves more than just providing nutritional information; it requires a multifaceted approach that addresses individual needs, preferences, and potential barriers. Successful interventions empower older adults to adopt sustainable dietary changes that enhance their overall health.Effective communication strategies are essential for educating older adults about healthy eating.
Older adults often have diverse backgrounds, experiences, and levels of understanding regarding nutrition. Tailoring communication to individual needs and preferences is key. This includes using clear, simple language, avoiding jargon, and incorporating visual aids like infographics and recipes. Active listening and acknowledging their existing knowledge and preferences are equally important.
It’s concerning how the quality of diet for older adults has declined lately. One key factor to consider, though, is the parallel issue of emotional eating in teenagers. Understanding how gateway foods influence teen dietary habits, as explored in this insightful article on teen dietary habits what parents should know about emotional eating and gateway foods , can offer valuable lessons for improving the nutritional choices of older adults too.
Ultimately, fostering healthy eating habits, regardless of age, requires a multi-faceted approach.
Effective Communication Strategies
Effective communication strategies focus on clear, concise, and culturally sensitive information delivery. This approach ensures that the message resonates with older adults and fosters understanding. For example, using relatable examples, such as recipes using familiar ingredients, can significantly improve engagement. Simple language, avoiding complex medical terminology, and utilizing visuals, like colorful posters and easy-to-understand diagrams, can make the information more accessible and appealing.
Consider group discussions and interactive workshops, allowing for questions and shared experiences.
Simple and Engaging Activities
Promoting healthy eating habits goes beyond simply providing information. Engaging activities can motivate older adults to adopt healthier lifestyles. Cooking classes, led by experienced chefs and nutritionists, can be particularly effective. They can provide hands-on experience with preparing nutritious meals and offer practical tips for incorporating healthy ingredients into daily routines. Community gardens, offering opportunities to grow fresh produce and connect with peers, can foster a sense of community and encourage healthy food choices.
Group meal preparation sessions, facilitated by trained professionals, can be social and enjoyable while teaching practical cooking skills and promoting healthy eating patterns.
Infographic: Weekly Meal Plan for Older Adults
| Day | Breakfast | Lunch | Dinner |
|---|---|---|---|
| Monday | Oatmeal with berries and nuts | Grilled chicken salad with mixed greens and vinaigrette | Baked salmon with roasted vegetables (broccoli, carrots, sweet potatoes) |
| Tuesday | Scrambled eggs with whole-wheat toast and avocado | Lentil soup with whole-grain bread | Lean beef stir-fry with brown rice and plenty of colorful vegetables |
| Wednesday | Yogurt with granola and fruit | Tuna salad sandwich on whole-wheat bread with a side of fruit | Chicken breast with quinoa and steamed green beans |
| Thursday | Smoothie with fruit, yogurt, and spinach | Leftovers from dinner | Turkey meatballs with zucchini noodles and marinara sauce |
| Friday | Whole-wheat pancakes with fruit and syrup | Hummus and vegetable wrap with whole-wheat tortilla | Vegetarian chili with cornbread |
| Saturday | Breakfast burritos with eggs, beans, and cheese | Leftovers from dinner | Homemade pizza with whole-wheat crust and plenty of vegetables |
| Sunday | French toast with berries | Soup and salad | Roast chicken with mashed potatoes and steamed asparagus |
This infographic provides a sample weekly meal plan, highlighting a variety of healthy food choices. Adjust portion sizes and ingredients based on individual needs and preferences. Remember to incorporate plenty of fruits, vegetables, lean protein, and whole grains.
Motivating Sustainable Dietary Changes
Motivating older adults to make sustainable dietary changes involves understanding their individual needs and preferences. Personalized goals, tailored to each person’s abilities and interests, are crucial. Positive reinforcement, such as acknowledging progress and celebrating milestones, plays a vital role in fostering motivation. Encouraging a supportive environment, whether through family, friends, or support groups, can significantly enhance the likelihood of long-term adherence.
Providing clear and practical strategies for incorporating healthy choices into existing routines and addressing potential challenges are essential.
Illustrative Examples: Quality Of Diet For Older Adults Has Declined Heres How To Fix It
Nourishing meals and snacks play a crucial role in maintaining health and well-being, especially for older adults. Proper nutrition supports physical function, cognitive abilities, and overall quality of life. These examples demonstrate how to incorporate diverse nutrients into meals while considering potential dietary restrictions and mobility challenges.
Healthy Breakfast Option for Older Adults
A balanced breakfast is essential for providing energy and essential nutrients to start the day. This option focuses on whole grains, protein, and healthy fats, while being easy to prepare and digest.A great breakfast option includes oatmeal with berries and nuts. The oatmeal provides complex carbohydrates for sustained energy, while the berries offer vitamins, minerals, and antioxidants. Nuts contribute healthy fats, protein, and fiber.
- Ingredients: ½ cup rolled oats, 1 cup water or milk (dairy or non-dairy), ½ cup mixed berries (fresh or frozen), ¼ cup chopped nuts (almonds, walnuts, or pecans), 1 tablespoon chia seeds (optional).
- Preparation: Combine oats and liquid in a saucepan. Bring to a boil, then reduce heat and simmer for 5-7 minutes, or until desired consistency is reached. Stir in berries, nuts, and chia seeds. Serve warm.
- Nutritional Benefits: This breakfast provides complex carbohydrates for sustained energy, fiber for digestive health, antioxidants from berries, protein and healthy fats from nuts, and omega-3 fatty acids (if chia seeds are used). It’s also low in fat and high in fiber.
Sample Lunch Menu for Older Adults with Mobility Issues
A suitable lunch menu for older adults with arthritis or other mobility challenges should prioritize easy-to-eat foods and nutrients.For older adults with arthritis or limited mobility, a well-structured lunch menu that avoids difficult-to-chew foods is crucial. This sample lunch focuses on soft textures and easily digestible nutrients.
- Main Course: Chicken or fish salad sandwich on whole-wheat bread. The salad can be made with shredded cooked chicken or fish, light mayonnaise, diced vegetables (carrots, celery, bell peppers), and herbs. The sandwich provides protein and essential nutrients.
- Side Dish: A large portion of mixed greens with a light vinaigrette dressing. This adds fiber, vitamins, and minerals to the meal.
- Dessert: A small portion of fruit salad (e.g., melon, berries, or grapes). The fruit provides natural sugars and vitamins.
Healthy Dinner Recipe with Cultural Appropriateness, Quality of diet for older adults has declined heres how to fix it
Many older adults have cultural preferences and dietary restrictions. This recipe incorporates familiar flavors and ingredients while meeting nutritional needs.For a culturally sensitive dinner, consider a recipe that incorporates familiar ingredients and spices while ensuring the meal is nutritious. A lentil soup, for example, can be adapted to various cultural preferences.
- Ingredients: 1 tbsp olive oil, 1 onion, 2 carrots, 2 celery stalks, 2 cloves garlic, 1 cup red lentils, 4 cups vegetable broth, 1 tsp cumin, ½ tsp turmeric, salt and pepper to taste, chopped cilantro (optional), cooked rice or naan bread for serving.
- Preparation: Sauté onion, carrots, and celery in olive oil until softened. Add garlic, cumin, and turmeric. Add lentils and vegetable broth. Bring to a boil, then simmer for 20-25 minutes, or until lentils are tender. Season with salt and pepper.
It’s disheartening to see the quality of diet in older adults declining. It’s a real struggle, like Randy Travis’s long road back to recovery after his health challenges. Randy Travis’s long road back highlights the importance of proactive steps to improve health and well-being. Fortunately, there are actionable strategies to reverse this trend and ensure a better quality of life for seniors.
Small, consistent changes can make a big difference, from incorporating more fruits and vegetables to managing portion sizes effectively.
Garnish with cilantro if desired. Serve with rice or naan bread.
- Nutritional Benefits: This recipe provides a good source of protein, fiber, and complex carbohydrates. Lentils are a good source of iron and other minerals. It can be easily adapted to different cultural preferences by adjusting spices and serving accompaniments.
Healthy Snack for Older Adults
Snacks provide essential nutrients between meals and help maintain energy levels. For older adults, easy-to-eat and nutritious snacks are crucial.This snack is an easy, convenient option for older adults, focusing on protein and healthy fats.
- Ingredients: Greek yogurt (plain or with a small amount of fruit), handful of mixed nuts (almonds, walnuts, or cashews), and a small handful of berries.
- Preparation: Combine Greek yogurt, nuts, and berries in a small bowl. This is a simple and quick snack that is ready in minutes.
- Nutritional Benefits: Greek yogurt provides protein and calcium, while nuts offer healthy fats and protein. Berries add vitamins and antioxidants. This combination offers a balanced mix of nutrients to maintain energy levels between meals.
Practical Tools and Resources

Taking a proactive approach to improving dietary quality for older adults requires practical tools and resources. These tools empower individuals to make informed choices and create sustainable, healthy eating habits. This section offers concrete steps and resources to support successful dietary changes.Understanding the specific nutritional needs of older adults, coupled with accessible tools, creates a path towards enhanced well-being.
Practical strategies, such as meal planning and nutritional comparisons, empower individuals to make informed decisions, ultimately contributing to better health outcomes.
Sample Weekly Meal Plan for Older Adults
A well-structured meal plan is crucial for ensuring adequate nutrient intake. The following sample weekly meal plan incorporates a variety of food groups, while adhering to general dietary guidelines for older adults. It emphasizes balanced portions and nutrient-dense foods.
| Day | Breakfast | Lunch | Dinner | Snacks |
|---|---|---|---|---|
| Monday | Oatmeal with berries and nuts | Turkey and avocado sandwich on whole-wheat bread | Baked salmon with roasted vegetables | Greek yogurt with fruit, hard-boiled egg |
| Tuesday | Scrambled eggs with spinach and whole-wheat toast | Lentil soup with whole-grain bread | Chicken stir-fry with brown rice | Apple slices with peanut butter, small handful of almonds |
| Wednesday | Smoothie with protein powder, fruit, and vegetables | Leftover chicken stir-fry | Lean ground beef and bean chili with whole-wheat tortilla chips | Cottage cheese with sliced peaches, small bowl of popcorn |
| Thursday | Whole-wheat pancakes with fruit and syrup (in moderation) | Tuna salad sandwich on whole-wheat bread with a side of baby carrots | Turkey meatballs with zucchini noodles | Rice cakes with hummus and cucumber slices, a handful of walnuts |
| Friday | Yogurt parfait with granola and fruit | Leftover turkey meatballs and zucchini noodles | Baked chicken breast with sweet potato and green beans | String cheese, small banana |
| Saturday | Breakfast burrito with eggs, beans, and salsa | Salad with grilled chicken or fish, mixed greens, and a light vinaigrette | Pasta with marinara sauce and lean ground turkey | Edamame, a small portion of dark chocolate |
| Sunday | French toast with fruit and maple syrup (in moderation) | Leftover pasta and turkey | Roast chicken with roasted root vegetables | Hard-boiled eggs, small apple |
Nutritional Value Comparison of Food Choices
Understanding the nutritional content of different foods allows individuals to make informed choices. The table below illustrates the approximate nutritional value of common food choices, highlighting the variability in calories, protein, and vitamins across different food groups.
| Food | Calories | Protein (grams) | Vitamin C (mg) | Calcium (mg) |
|---|---|---|---|---|
| Baked Chicken Breast (4oz) | 150 | 30 | 0 | 10 |
| Oatmeal (1 cup cooked) | 180 | 5 | 1 | 20 |
| Salmon (4oz) | 200 | 25 | 0 | 15 |
| Beans (1 cup cooked) | 250 | 15 | 3 | 25 |
| Yogurt (1 cup) | 120 | 10 | 5 | 300 |
Creating a Personalized Meal Plan
Developing a personalized meal plan involves several steps. These steps ensure that the plan aligns with individual needs and preferences.
- Assess Nutritional Needs: Consider age, activity level, health conditions, and any allergies or dietary restrictions. Consult a healthcare professional or registered dietitian for personalized guidance.
- Identify Food Preferences and Habits: Acknowledge current eating habits and preferences to make the transition easier and more sustainable.
- Set Realistic Goals: Establish achievable goals for gradual dietary improvements, rather than drastic changes.
- Incorporate Variety: Include a wide range of nutrient-rich foods from all food groups.
- Monitor Progress and Adjust: Track progress regularly and make adjustments to the plan as needed.
Community Resources and Support Groups
Community resources can provide valuable support for older adults seeking to improve their nutrition.
- Local Senior Centers: Many senior centers offer nutrition education programs, meal services, and support groups.
- Registered Dietitians: Registered dietitians can provide personalized dietary counseling and meal planning assistance.
- Community Health Clinics: Community health clinics often offer nutrition counseling and resources for older adults.
- Support Groups: Joining support groups allows for shared experiences, encouragement, and peer-to-peer learning.
- Online Forums: Online forums dedicated to nutrition and healthy aging can offer valuable information and support.
Closing Notes
In conclusion, improving the quality of diet for older adults requires a comprehensive approach. From understanding nutritional needs to addressing barriers and promoting healthy habits, this guide provides a roadmap for positive change. By focusing on personalized plans, accessible resources, and community support, we can empower older adults to maintain optimal health and well-being throughout their later years.
Ultimately, prioritizing a nutritious diet is an investment in a healthier and happier future for older adults.




