Retinal implant hope of cure for macular degeneration is a revolutionary concept, offering a glimmer of hope for millions affected by this debilitating eye disease. This exploration dives deep into the technology, examining its potential to restore or enhance vision in patients suffering from macular degeneration. We’ll look at the different types of retinal implants, their historical development, and the ongoing clinical trials.
Moreover, we’ll discuss the challenges and limitations of this innovative approach, the ethical considerations, and patient perspectives.
Macular degeneration, a leading cause of vision loss, robs individuals of their ability to see fine details and colors, impacting their daily lives profoundly. This article meticulously examines the disease’s various forms, its impact, current treatments, and the crucial role retinal implants may play in improving or restoring sight. Understanding the potential of these implants, along with the associated risks, is essential for informed decision-making.
Introduction to Retinal Implants

Retinal implants are revolutionary devices designed to restore some vision in individuals with severe retinal diseases, such as macular degeneration and retinitis pigmentosa. These innovative technologies offer a glimmer of hope for those facing profound visual impairment, by bypassing the damaged retinal cells and directly stimulating the remaining healthy cells. The hope lies in the possibility of restoring visual function, though the degree of restoration varies greatly depending on the individual’s specific condition and the type of implant used.These devices work by employing micro-electrodes to deliver electrical signals to the remaining retinal cells, stimulating them to generate signals that the brain can interpret as visual information.
This process, while still under development, aims to mimic the natural electrical signaling pathways of the eye, effectively creating an artificial pathway for visual input. The success of retinal implants depends on several factors, including the extent of retinal damage, the individual’s brain plasticity, and the ongoing advancement of implant technology.
Types of Retinal Implants
Currently, several types of retinal implants are available, each with its own strengths and limitations. These differences in functionality stem from varied electrode configurations and stimulation protocols. One common type uses a multi-electrode array to stimulate a larger area of the retina, potentially enabling a wider field of vision. Another approach focuses on stimulating specific retinal cells, aiming for higher resolution and improved visual acuity.
Historical Development of Retinal Implants
The journey towards retinal implants has been a long and arduous one, marked by both significant breakthroughs and setbacks. Early experiments focused on understanding the electrical activity within the retina and developing methods for delivering electrical stimuli. The early successes paved the way for more complex designs, leading to the current generation of implants that offer a degree of visual function to patients.
Key milestones in this field include the development of improved electrode materials, enhanced stimulation protocols, and more sophisticated signal processing algorithms.
Key Components of a Retinal Implant System
Understanding the intricate workings of a retinal implant system requires examining its core components. Each component plays a critical role in the overall functionality of the device.
| Component | Function | Material |
|---|---|---|
| Micro-electrode Array | Directly stimulates the remaining retinal cells | Biocompatible materials like platinum, gold, or silicon |
| Stimulator/Processor | Generates and delivers electrical pulses to the micro-electrode array | Integrated circuit, specialized microchips |
| Optical Imaging System | Captures light and converts it into electrical signals for the implant | Miniaturized cameras or optical lenses |
| Surgical Implantation Device | Facilitates safe and precise placement of the implant into the eye | Sterile, biocompatible materials |
| Connective Tissues/Electrodes | Transmits signals between the micro-electrode array and the implant’s processor | Flexible, biocompatible materials, insulated wires |
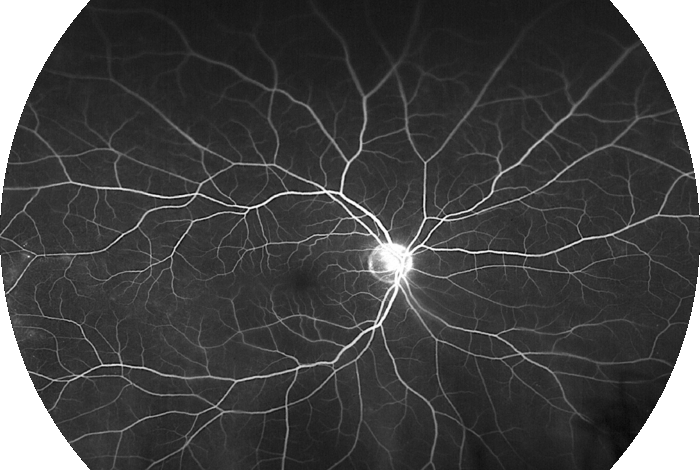
Macular Degeneration
Macular degeneration, a leading cause of vision loss in older adults, affects the macula, the central part of the retina responsible for sharp, central vision. This crucial area of the eye allows us to read, drive, and recognize faces. Understanding the different types, causes, and treatment options is vital for those affected and those seeking to prevent or manage this condition.Macular degeneration isn’t a single entity; it encompasses several forms, each with its own characteristics.
The two primary types, age-related macular degeneration (AMD), and other less common types, manifest differently and require specific approaches to diagnosis and management. The underlying causes are a complex interplay of genetic predisposition and environmental factors, and often include lifestyle choices.
Types of Macular Degeneration
Age-related macular degeneration (AMD) is the most common form, broadly categorized into two main types: dry and wet. Dry AMD, the more prevalent form, develops gradually, often over years, with the gradual breakdown of light-sensitive cells in the macula. Wet AMD, a more aggressive form, involves abnormal blood vessel growth under the macula, leading to rapid vision loss.
Causes of Macular Degeneration
While the precise causes of macular degeneration remain somewhat elusive, several factors contribute to its development. Genetics play a significant role, with family history often being a risk indicator. Environmental factors such as exposure to sunlight and smoking also contribute. Furthermore, lifestyle choices, such as diet and overall health, can influence the risk of developing the condition.
Impact on Vision and Daily Life
Macular degeneration significantly impacts vision, affecting the ability to perform daily tasks. Central vision loss makes reading, driving, and recognizing faces challenging. Individuals may experience distorted or blurred central vision, leading to difficulties with tasks requiring precise detail. The impact extends to social interactions, professional life, and overall quality of life. For example, someone with significant macular degeneration might find it hard to read a menu or recognize a friend’s face.
Current Treatment Options
Currently, there’s no cure for macular degeneration. Treatment options focus on slowing the progression of the disease and managing symptoms. For dry AMD, there are no specific treatments, and the focus is on managing risk factors and lifestyle modifications. For wet AMD, anti-VEGF injections can help stop or slow the growth of abnormal blood vessels. Laser therapy is another treatment option that may slow the progression of the condition in some cases.
Recent advancements in retinal implants offer a glimmer of hope for those battling macular degeneration. These innovative devices could potentially restore sight, but the changing healthcare landscape, particularly the shift in patient preferences and access to care, raises questions about the future of traditional family medicine. For example, are millennials killing the family doctor? are millennials killing the family doctor ?
Ultimately, these technological leaps, combined with a nuanced understanding of healthcare access, could pave the way for a future where more people can benefit from improved vision and access to quality medical care.
Limitations of Current Treatments
Despite advancements, current treatments for macular degeneration have limitations. Anti-VEGF injections, while effective in some cases, require repeated treatments, potentially causing side effects. Furthermore, the effectiveness of these treatments varies from individual to individual, and the long-term effects are still being studied. Laser therapy can also have limitations in its ability to fully restore vision.
Effectiveness of Treatment Approaches
Comparing the effectiveness of different treatment approaches is complex, as outcomes vary significantly. Factors like the type and severity of AMD, individual patient response, and adherence to treatment protocols all influence results. While anti-VEGF injections can halt or slow vision loss in some patients with wet AMD, their long-term effectiveness needs further investigation.
Stages of Macular Degeneration
| Stage | Symptoms | Potential Impact on Visual Acuity |
|---|---|---|
| Early Dry AMD | Mild blurring or distortion of central vision, often unnoticed. | Minimal to moderate reduction in visual acuity. |
| Intermediate Dry AMD | Increasing difficulty with fine details, reduced color perception. | Moderate to significant reduction in visual acuity. |
| Advanced Dry AMD | Significant loss of central vision, making everyday tasks difficult. | Marked reduction in visual acuity, potential for legal blindness. |
| Early Wet AMD | Sudden onset of blurry or distorted central vision, sometimes with a dark spot in the center of vision. | Rapid and significant reduction in visual acuity. |
| Advanced Wet AMD | Progressive vision loss, often with severe distortion and loss of central vision. | Severe reduction in visual acuity, potential for legal blindness. |
Retinal Implants for Macular Degeneration
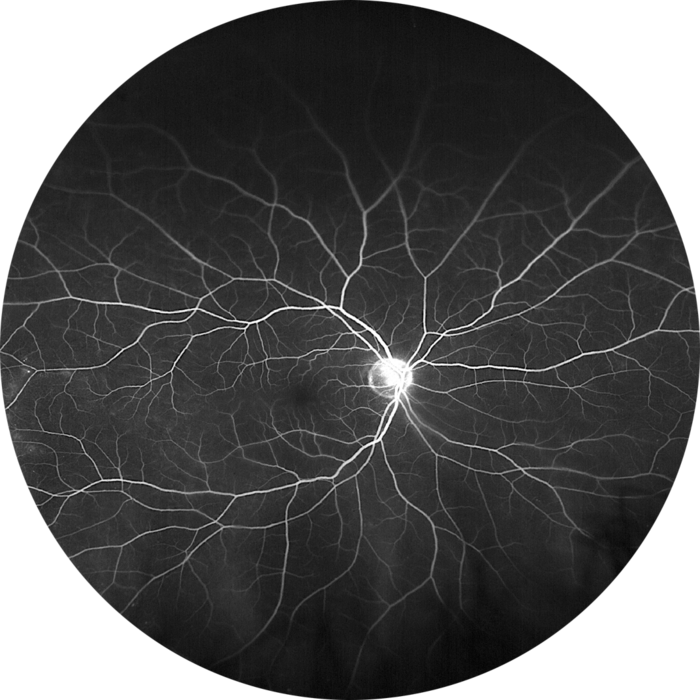
Retinal implants offer a glimmer of hope for individuals suffering from macular degeneration, a leading cause of vision loss. While not a cure, these innovative devices hold the potential to restore some sight and improve quality of life for those whose vision has been severely impacted. The technology is still evolving, and much research remains to be done, but early results are promising and highlight the potential for significant advancements in treating this debilitating condition.Retinal implants work by bypassing the damaged cells in the retina and directly stimulating the remaining healthy nerve cells.
This stimulation can create visual signals that the brain can potentially interpret, leading to improved vision. The ultimate goal is not just to restore vision to normal levels, but to enhance functional vision, enabling patients to perform everyday tasks more easily. The technology relies on the concept of bypassing the damaged photoreceptors and directly stimulating the retinal ganglion cells.
Potential Improvements in Vision
Retinal implants can potentially restore or enhance vision in patients with macular degeneration by stimulating the remaining healthy retinal cells. The stimulation can create rudimentary visual patterns, which the brain can sometimes interpret. The level of visual recovery varies significantly depending on the individual’s remaining retinal function, the specific implant design, and the level of stimulation. Some patients may experience improvements in visual acuity, while others might gain the ability to perceive shapes, light, and motion.
Challenges and Limitations
Several challenges hinder the widespread adoption of retinal implants for macular degeneration. One major hurdle is the complex nature of the eye and the intricate neural pathways involved in vision. Precise placement of the implant is critical for optimal stimulation and minimizing damage to surrounding tissues. Furthermore, the brain’s ability to interpret the signals generated by the implant can be variable and unpredictable.
The visual field produced by the implant is often limited and does not fully replicate natural vision. Long-term stability and effectiveness of the implant, as well as the potential for device failure, are also critical concerns.
Benefits and Risks
Potential benefits for patients with macular degeneration include improved quality of life, enhanced independence, and a renewed ability to participate in activities that require visual input. However, risks associated with retinal implants include infection, inflammation, and the potential for device malfunction or damage to surrounding tissues. Careful consideration of these risks and the patient’s overall health is crucial before proceeding with implant surgery.
Proper post-operative care and regular follow-up appointments are also essential for managing potential complications.
Comparison with Other Treatment Options
| Treatment Option | Effectiveness | Pros | Cons |
|---|---|---|---|
| Retinal Implants | Variable, dependent on individual and implant type | Potential for significant visual improvement, bypassing damaged areas | Complex surgery, potential for complications, variable outcomes, long-term effects uncertain |
| Vision Therapy | Limited, generally for specific visual impairments | Non-invasive, cost-effective | Not suitable for all types of macular degeneration, limited improvement |
| Low Vision Aids | Limited, enhances existing vision | Cost-effective, readily available | Does not restore vision, may not be suitable for all activities |
| Medications | Limited, primarily for slowing progression | Can slow the progression of macular degeneration | Does not restore vision, potential side effects |
The table above provides a basic comparison of retinal implant effectiveness against other treatment options. Each method has its own advantages and disadvantages, and the best course of action should be determined in consultation with an ophthalmologist or retina specialist, taking into account the specific characteristics of the patient’s condition.
Clinical Trials and Research
Retinal implants for macular degeneration are currently undergoing rigorous clinical trials to assess their efficacy and safety. These trials are crucial for determining whether these devices can truly restore vision for patients suffering from this debilitating condition. The ongoing research seeks to improve the implant technology, refine surgical techniques, and understand the long-term effects of the implants.
Ongoing Clinical Trials
Several clinical trials are actively recruiting participants or analyzing data to evaluate retinal implants. These trials vary in their design, focusing on different aspects of the technology and its impact on vision. The diversity of these trials reflects the need for a comprehensive understanding of how retinal implants function and how they can best be integrated into the lives of patients.
Trial Methodologies and Designs
Clinical trials investigating retinal implants for macular degeneration employ various methodologies. Some trials use a randomized, controlled design, comparing the implant group to a control group receiving standard care. Others may focus on specific aspects of the implant, such as optimizing stimulation protocols or evaluating the integration of the implant with the retina. Data collection methods include visual acuity testing, electroretinography, and patient questionnaires to capture subjective experiences and assess the quality of life improvement.
These trials are often multi-center studies, conducted at multiple medical institutions across the globe. The data collected from these trials is meticulously analyzed to draw reliable conclusions.
Key Findings and Results
Early clinical trials have provided valuable insights into the potential of retinal implants. While results vary, some studies have demonstrated improvements in visual function, such as increased visual field or improved ability to perceive shapes and colors. However, the success of these implants is not uniform and depends on several factors, including the individual characteristics of the patient and the specific design of the implant.
Continued monitoring of patients over extended periods is essential to evaluate the long-term effects and complications of the implant.
Metrics for Evaluating Success
| Metric | Description | Importance |
|---|---|---|
| Visual Acuity | Sharpness of vision, measured in letters on an eye chart. | Fundamental measure of improved vision. |
| Visual Field | Extent of the visual field, measured in degrees. | Quantifies the expanded range of sight. |
| Contrast Sensitivity | Ability to distinguish objects with similar brightness. | Assesses ability to see in varied lighting conditions. |
| Color Vision | Perception of different colors. | Important for daily activities and quality of life. |
| Quality of Life Measures | Patient-reported assessments of daily activities and well-being. | Evaluates overall improvement in functional abilities. |
| Safety and Complications | Frequency and severity of adverse events. | Critical to ensure the implants are safe for long-term use. |
These metrics are essential for evaluating the efficacy and safety of retinal implants. Consistent and rigorous evaluation through these metrics is paramount to ensuring the ethical and reliable advancement of the technology.
Future Directions and Potential: Retinal Implant Hope Of Cure For Macular Degeneration
Retinal implants are rapidly evolving, offering a glimmer of hope for restoring vision in patients with severe eye conditions like macular degeneration. Current technology has demonstrated the potential to stimulate the remaining retinal cells, but significant advancements are necessary to achieve optimal outcomes. This exploration delves into the exciting future of retinal implants, considering improved designs, materials, and the broader implications for treating a wider range of eye diseases.The current state of retinal implant technology is characterized by various approaches, each with its own set of advantages and limitations.
Some implants utilize electrical stimulation to activate remaining retinal cells, while others employ light-sensitive components. While progress has been made, challenges remain in terms of long-term stability, visual acuity, and the overall patient experience.
Improved Designs and Materials, Retinal implant hope of cure for macular degeneration
Retinal implants are currently being refined to enhance their efficacy and safety. Engineers are focusing on miniaturization and biocompatibility to reduce the size and potential for rejection. Advanced materials, such as biodegradable polymers and biocompatible metals, are being investigated to create more robust and durable implants. These improvements are crucial for long-term success, minimizing the risk of complications and maximizing the implant’s longevity.
For example, recent developments in 3D printing techniques allow for more customized implant designs tailored to individual patient needs, potentially leading to improved visual outcomes.
Recent breakthroughs in retinal implants offer a glimmer of hope for a cure for macular degeneration. While these advancements are promising, it’s worth noting that the sheer volume of people predisposed to cholesterol issues, as highlighted in a recent study ( more born with cholesterol risk than previously thought ), might indicate a need for broader preventative measures alongside these exciting new treatments.
Ultimately, the future of retinal implant technology could significantly improve the lives of many, potentially even surpassing existing challenges.
Impact on Patients with Macular Degeneration
The expected impact of advancements in retinal implant technology on patients with macular degeneration is substantial. Improved designs, particularly those that provide more precise stimulation patterns, could potentially restore functional vision, enabling patients to perform everyday tasks like reading, recognizing faces, and navigating their surroundings with greater independence. Enhanced integration between the implant and the patient’s existing neural pathways will be critical for better visual perception and integration.
Early clinical trials are demonstrating promising results in terms of improving visual acuity and the ability to discern shapes and colors.
Areas of Future Research and Development
Further research is crucial to enhance the effectiveness and long-term success of retinal implants. One area of focus is improving the resolution and clarity of the visual field. Researchers are exploring ways to increase the number of electrodes or photoreceptors in the implant, potentially leading to sharper images and a wider field of view. Additionally, optimizing the stimulation protocols and algorithms will be vital for enhancing visual perception and reducing side effects.
Studies on the impact of long-term stimulation on retinal health and the development of new strategies to prevent potential complications are also crucial.
Evolution in Treating Other Eye Conditions
The potential of retinal implants extends beyond macular degeneration. The technology could revolutionize the treatment of other retinal diseases like retinitis pigmentosa and diabetic retinopathy. The ability to stimulate or replace damaged retinal cells holds immense promise for restoring or enhancing vision in individuals suffering from these conditions. As the technology advances and becomes more refined, it is plausible that retinal implants could play a critical role in restoring vision for a broader spectrum of eye diseases, paving the way for a future where sight loss is not inevitable.
Patient Experiences and Perspectives
Retinal implants, while offering a glimmer of hope for restoring vision, are more than just medical procedures. They profoundly impact patients’ lives, altering their perspectives and creating a unique tapestry of experiences. This section delves into the realities of patients who have undergone these procedures, exploring the emotional, practical, and psychological journeys they embark on.The transformative nature of regaining or partially regaining sight is undeniable, but the path to recovery isn’t always straightforward.
While retinal implants offer a glimmer of hope for curing macular degeneration, it’s crucial to remember that the path to a healthier future often involves proactive steps. For example, if you’re experiencing flu-like symptoms, it’s wise to prepare a list of questions for your doctor, such as those found in this helpful guide on what to ask doctor about flu.
Ultimately, the ongoing research and development surrounding retinal implants provide a hopeful future for those impacted by macular degeneration.
Understanding the experiences, challenges, and triumphs of these patients provides crucial insight into the future of this innovative technology.
Real-Life Patient Accounts
Patient narratives offer invaluable insights into the human experience of vision restoration. Many individuals describe a profound sense of relief and empowerment when they regain a degree of visual function. This newfound ability to see faces, read, or simply appreciate the world around them often leads to a profound shift in their outlook. For example, a patient with macular degeneration might initially feel isolated and restricted, but the ability to see loved ones’ expressions again can be incredibly therapeutic.
Impact on Daily Life
Retinal implants can significantly enhance a patient’s daily life. For example, activities previously impossible, such as recognizing faces, reading simple text, or navigating familiar surroundings, become achievable. The ability to participate more fully in social interactions and maintain independence are often cited as significant benefits. However, it’s also important to acknowledge that the visual experience produced by these implants is not identical to natural vision.
The level of detail, sharpness, and color perception can vary significantly.
Challenges Faced by Patients
While the benefits of retinal implants are undeniable, patients also face unique challenges. One key area of concern is the adjustment period. Learning to interpret the altered visual input and adapt to the new way of seeing can be a complex process. Further, the ongoing need for follow-up care, rehabilitation, and potential adjustments to the implant itself are significant factors to consider.
Furthermore, the psychological impact of living with vision loss and then undergoing a procedure to restore it can be substantial.
Effectiveness and Safety: Patient Feedback
| Aspect | Positive Feedback | Negative Feedback |
|---|---|---|
| Visual Acuity | Improved ability to recognize faces, read, and navigate | Variable levels of visual clarity and detail |
| Daily Activities | Increased independence and participation in social activities | Difficulties with adapting to the new visual input |
| Psychological Impact | Increased confidence and emotional well-being | Adjustment period can be emotionally challenging |
| Safety | Minimal reported complications | Potential for side effects and long-term issues |
This table summarizes patient feedback on the effectiveness and safety of retinal implants. The feedback highlights both the positive and negative aspects, illustrating the complexity of the patient experience. It is crucial to approach this information with nuance and acknowledge that individual experiences will vary significantly.
Psychological Aspects of Vision Restoration
The restoration of vision through retinal implants is a multifaceted process that has a profound impact on the patient’s psychological well-being. The emotional journey from vision loss to potential restoration can be complex, involving periods of grief, adjustment, and hope. Patients might experience feelings of anxiety or uncertainty as they learn to navigate their new visual world. However, many patients report experiencing increased confidence, improved mood, and a renewed sense of purpose.
Furthermore, the ability to reconnect with loved ones and engage with the world in a more meaningful way can lead to significant improvements in quality of life.
Ethical Considerations and Societal Impact
Retinal implants, while promising a potential cure for macular degeneration, raise complex ethical and societal concerns. The transformative potential of this technology demands careful consideration of its implications for individuals, society, and the healthcare system. Access, equity, and the long-term impact on quality of life must be evaluated alongside the technical advancements.
Ethical Concerns
The ethical landscape surrounding retinal implants is multifaceted. Fundamental questions about informed consent, particularly for vulnerable populations, and the potential for coercion or undue influence are paramount. Furthermore, the potential for unintended consequences, such as dependence on technology or the creation of new social inequalities, requires careful consideration. The cost-effectiveness of this technology and its impact on healthcare resource allocation also deserve scrutiny.
- Informed Consent and Vulnerable Populations: Ensuring patients, especially those with cognitive impairments or visual impairments, understand the complexities of retinal implants and the potential risks and benefits is crucial. Processes for informed consent need to be tailored to individual needs and capacities. This includes clear, accessible language and culturally sensitive approaches to communication. Examples of vulnerable populations include those with limited literacy or language barriers, or individuals with diminished cognitive function.
- Coercion and Undue Influence: The potential for coercion or undue influence exists if the societal pressure to adopt this technology becomes significant. This could manifest as financial incentives, social stigma against non-adoption, or even family pressure. Policies and regulations need to be in place to safeguard individual autonomy and decision-making. An example is the historical pressure on individuals with disabilities to adopt specific interventions or therapies.
- Potential for Unintended Consequences: The long-term effects of retinal implants on daily life and societal integration are not fully understood. Psychological and social impacts, including the possible creation of new inequalities or dependencies on technology, need careful monitoring and research. This can be seen in the adoption of assistive technologies where unintended consequences such as social isolation have been noted.
- Cost-Effectiveness and Resource Allocation: Retinal implants are likely to be expensive. Determining the cost-effectiveness compared to other treatment options and the potential impact on healthcare resource allocation is vital. Considerations should include the cost of the device, surgery, and long-term maintenance. Examples of similar situations include the pricing of advanced cancer therapies or organ transplants.
Societal Implications
Accessibility and equity are key societal concerns surrounding retinal implant technology. The potential for a technology divide, where access to advanced treatments is limited to those with financial resources, could exacerbate existing health disparities. The potential for social stigma and discrimination toward those who choose not to utilize the technology must be addressed.
- Accessibility and Equity: Ensuring equitable access to retinal implants for all individuals, regardless of socioeconomic status, is critical. This requires policies that address affordability, availability, and geographical access to the technology. This includes developing strategies to reduce the financial burden for patients and families.
- Technology Divide: The potential for a technology divide, where access to advanced treatments is limited to those with financial resources, could exacerbate existing health disparities. Efforts must be made to mitigate this issue through subsidies, insurance coverage, and public funding initiatives.
- Social Stigma and Discrimination: Individuals who choose not to utilize retinal implants might face social stigma or discrimination. Public awareness campaigns and educational initiatives can help reduce the stigma and promote understanding. This is similar to the challenges faced by individuals who choose not to use assistive devices in other contexts.
Healthcare System and Economic Impact
The widespread adoption of retinal implant technology will significantly impact the healthcare system and economy. Increased demand for specialized personnel, infrastructure, and research will place pressure on existing resources. The potential economic burden on healthcare systems and insurance providers needs careful analysis.
| Ethical Concern | Possible Solutions |
|---|---|
| Informed Consent | Tailored consent processes, accessible language, cultural sensitivity |
| Coercion/Undue Influence | Clear policies and regulations, independent oversight, ethical review boards |
| Unintended Consequences | Longitudinal studies, public health surveillance, ongoing evaluation |
| Cost-Effectiveness | Comparative studies, cost-benefit analyses, alternative funding models |
| Accessibility and Equity | Affordable pricing, insurance coverage, equitable access |
| Technology Divide | Subsidies, public funding, accessible technology |
| Social Stigma | Public awareness campaigns, educational initiatives, promoting inclusivity |
Ultimate Conclusion
In conclusion, retinal implants hold significant promise for treating macular degeneration, offering a potentially life-altering solution for those suffering from this debilitating eye condition. While challenges remain, ongoing research and clinical trials are pushing the boundaries of this innovative technology. The ethical considerations, societal impact, and future developments of retinal implants deserve careful attention. The potential for improved quality of life for patients, alongside the need for responsible development and accessibility, should be at the forefront of discussions surrounding this technology.
