Sense of smell could be a signal of MS progression, potentially offering a new avenue for early detection and monitoring of this complex disease. Multiple sclerosis (MS) is a debilitating autoimmune disease affecting the central nervous system, often characterized by unpredictable symptoms and challenging to manage. Understanding the nuances of MS progression is crucial, and this exploration delves into the potential connection between olfactory function and the development or progression of MS.
We’ll examine the neural pathways involved in olfaction, the potential physiological mechanisms linking smell changes to MS, and the current research findings on the subject. A variety of factors influence MS progression, including genetics, environmental factors, and lifestyle choices. This exploration will also cover the different types of MS and their typical symptoms, including possible olfactory changes.
The potential for smell changes to act as a biomarker for MS progression is intriguing, offering a potentially non-invasive method for monitoring disease activity and treatment response. This could lead to earlier diagnosis, allowing for timely interventions and potentially altering the course of the disease. We will explore the potential diagnostic and prognostic value of olfactory dysfunction as a marker for MS progression, contrasting it with other clinical markers.
The potential mechanisms linking smell changes to MS progression will also be discussed, including inflammatory and degenerative processes, oxidative stress, neuroinflammation, axonal damage, and demyelination.
Introduction to Multiple Sclerosis (MS)
Multiple Sclerosis (MS) is a chronic, autoimmune disease affecting the central nervous system. Characterized by inflammation and demyelination, MS disrupts the communication pathways between the brain and the body. This complex interplay of factors leads to a wide range of symptoms, impacting different individuals in varying ways. Understanding the disease’s unpredictable progression is crucial for effective management and support.The current understanding of MS progression highlights its variability.
While some individuals experience periods of remission, others face a more progressive decline in function. Predicting the course of the disease remains a significant challenge, impacting treatment strategies and patient expectations. Factors such as genetic predisposition, environmental exposures, and lifestyle choices all play a role in shaping the disease’s trajectory.
Factors Influencing MS Progression
Several factors contribute to the progression of MS, highlighting the complexity of the disease. Genetic predisposition plays a substantial role, as individuals with a family history of MS are at increased risk. Environmental exposures, such as infections and geographic location, are also considered contributing factors. Lifestyle choices, including diet, exercise, and stress management, are recognized to potentially influence the disease’s course.
The precise interaction of these factors remains an area of ongoing research.
MS Subtypes and Symptom Profiles
The following table Artikels different MS subtypes and their common symptom profiles, including potential olfactory (smell) changes. Note that these are general trends, and individual experiences can vary significantly.
| MS Subtype | Typical Symptoms | Potential Olfactory Changes |
|---|---|---|
| Relapsing-Remitting MS (RRMS) | Characterized by periods of relapse followed by remission. Common symptoms include numbness, tingling, vision problems, muscle weakness, and fatigue. | Possible, but less frequently reported compared to other sensory changes. May include a decreased ability to detect smells or changes in smell perception. |
| Primary Progressive MS (PPMS) | Symptoms gradually worsen from the onset, without distinct relapses or remissions. Progressive neurological deficits are observed. | Possible, but again, less frequently reported compared to other sensory changes. Changes in smell perception or reduced sensitivity might be present. |
| Secondary Progressive MS (SPMS) | Initially presents as relapsing-remitting, but eventually transitions into a progressive course. Symptoms steadily worsen over time. | Possible, and the frequency may increase as the disease progresses. Changes in smell perception or a reduced ability to detect smells might be observed. |
| Progressive-Relapsing MS (PRMS) | Progressive neurological decline from the onset, with superimposed relapses. | Potential for olfactory changes, though the specific patterns might vary depending on the individual’s experience with the disease. |
The Sense of Smell and Neurological Function
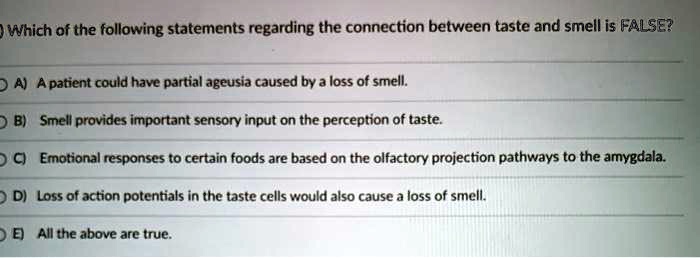
Our sense of smell, or olfaction, is more than just a pleasant experience; it’s deeply intertwined with our neurological well-being. The intricate pathways connecting our noses to our brains highlight the interconnectedness of various neurological systems. Understanding these connections is crucial, especially when considering potential links to neurological conditions like Multiple Sclerosis (MS).Olfactory pathways begin with sensory neurons in the nasal cavity.
These specialized receptors detect airborne odor molecules, triggering electrical signals that travel along specific neural pathways to the olfactory bulb, a key structure in the brain. From there, these signals are relayed to various brain regions, including the limbic system, which is heavily involved in emotions and memory, and the cortex, where higher-level processing and interpretation of the smell occur.
This complex network underscores the profound influence of olfaction on our cognitive and emotional experience.
Neural Pathways in Olfaction
The olfactory system stands out for its direct connection to the brain, bypassing the thalamus, the primary relay station for most sensory information. This direct route emphasizes the crucial role of smell in quickly triggering responses, including emotional and behavioral ones. The intricate interplay between the olfactory bulb and the limbic system highlights the profound influence of smell on memory and emotion.
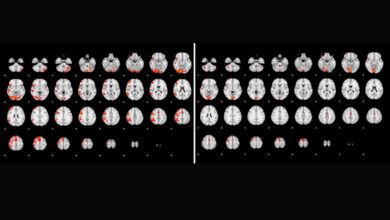
Recent research suggests a fascinating connection between a diminished sense of smell and Multiple Sclerosis progression. It’s a complex area, and while studying how brain imaging in autism children helps us understand neurological pathways, autism children brain imaging might offer parallels. Perhaps the olfactory system, or sense of smell, could be a sensitive indicator of neurological changes in MS.
Further investigation into this link is crucial for better understanding and potential early detection.
Potential Link Between Olfactory Function and Other Neurological Systems
Olfaction isn’t isolated; it interacts extensively with other neurological systems. The interconnectedness of the olfactory system with the limbic system, responsible for memory and emotion, highlights the potential impact of smell-related changes on cognitive function. Similarly, the links between the olfactory system and the central nervous system, particularly the brainstem, could indicate a broader influence on neurological processes, including autonomic functions.
Factors Affecting Olfactory Perception
Several factors can influence olfactory perception, making it a complex and nuanced experience. Age, for example, often plays a role; olfactory sensitivity tends to decrease with age. Gender differences in olfactory perception also exist, although the specific reasons for these variations are still under investigation. Underlying medical conditions, such as nasal congestion, upper respiratory infections, or even neurological disorders like MS, can significantly affect the ability to perceive odors.
These factors need careful consideration when assessing olfactory function.
Potential Physiological Mechanisms Linking Smell Changes and MS Progression
| Potential Physiological Mechanism | Explanation |
|---|---|
| Axonal Degeneration | Damage to the axons, the long extensions of neurons, can disrupt the transmission of signals along olfactory pathways. This can lead to reduced olfactory sensitivity. |
| Inflammation | MS involves inflammation in the central nervous system. Inflammation within the olfactory pathways can interfere with signal transmission and perception. |
| Myelin Dysfunction | Myelin, the protective covering around axons, plays a critical role in signal transmission. Myelin damage in MS can impact the efficiency of olfactory signal conduction. |
| Neurotransmitter Imbalance | Neurotransmitters are crucial for signal transmission within the brain. Disruptions in neurotransmitter levels in the olfactory pathways could affect olfactory perception. |
| Structural Changes in the Olfactory Bulb | MS can cause structural changes in the olfactory bulb, the primary processing center for smell. These changes can alter the processing of olfactory information. |
Olfactory Dysfunction in Neurological Diseases
Our sense of smell, or olfaction, is intricately linked to our overall neurological health. Disruptions in this system can be early indicators of underlying neurological conditions. Understanding how olfactory dysfunction manifests in various diseases is crucial for early diagnosis and potentially predicting disease progression. This exploration delves into the patterns of smell loss in conditions like Parkinson’s and Alzheimer’s, contrasting them with potential changes in MS.The loss of smell, or anosmia, isn’t simply a nuisance; it can be a symptom that signals deeper neurological issues.
In some cases, olfactory dysfunction can precede other, more noticeable symptoms, making it a potentially valuable biomarker. Identifying specific patterns in how smell is affected across different neurological conditions can aid in differential diagnosis and potentially predict disease progression.
Olfactory Dysfunction in Parkinson’s Disease
Parkinson’s disease, characterized by the progressive degeneration of dopamine-producing neurons, often presents with hyposmia (reduced smell) or anosmia. This olfactory impairment typically occurs early in the disease process and is often an early indicator of the condition. It is often accompanied by other motor and non-motor symptoms. The precise mechanisms linking dopamine depletion and olfactory dysfunction are still under investigation, but research suggests a connection between the olfactory bulb and the dopaminergic pathways in the brain.
Olfactory Dysfunction in Alzheimer’s Disease, Sense of smell could be a signal of ms progression
Alzheimer’s disease, a progressive neurodegenerative disorder, is also associated with olfactory dysfunction. Patients with Alzheimer’s often experience hyposmia or anosmia, frequently occurring in the early stages of the disease. The olfactory deficits are thought to be linked to the accumulation of amyloid plaques and neurofibrillary tangles, characteristic pathologies of Alzheimer’s. These abnormalities disrupt the neural pathways responsible for olfactory processing.
Olfactory Dysfunction in Multiple Sclerosis (MS)
While olfactory dysfunction is less prominent in MS than in Parkinson’s or Alzheimer’s, it can still occur. The pattern of smell loss in MS is variable and not as clearly defined as in other neurological conditions. Potential olfactory changes in MS might be subtle and could involve both hyposmia and dysosmia (distorted sense of smell). These changes are thought to stem from demyelination affecting the olfactory pathways, but further research is needed to fully elucidate the relationship.
Comparison of Olfactory Loss Patterns
| Disease | Olfactory Dysfunction Pattern | Potential MS Correlation ||——————-|——————————————————————————————-|————————-|| Parkinson’s Disease | Typically early onset, often progressive hyposmia or anosmia, often accompanied by motor symptoms | Potential early indicator of MS-related olfactory dysfunction, but requires further research || Alzheimer’s Disease | Frequently early onset, often progressive hyposmia or anosmia, often accompanies cognitive decline | Potential early indicator of MS-related olfactory dysfunction, but requires further research || Multiple Sclerosis | Variable pattern, potentially subtle hyposmia or dysosmia, not as consistently associated with other symptoms | Could be an early, subtle indicator of MS progression, requires further research |
Olfactory Assessment Methods
Accurate assessment of olfactory function is essential for detecting and characterizing olfactory dysfunction. Various methods are employed to evaluate the sense of smell, including standardized olfactory tests and questionnaires.
Recent research suggests a surprising connection between a diminished sense of smell and the progression of multiple sclerosis (MS). This fascinating finding raises important questions about early detection and treatment. Considering the complexities of healthcare decisions, especially in the context of death with dignity laws in the Trump era , it’s crucial to examine how such advancements in medical understanding impact patient autonomy and the choices available.
Ultimately, a better understanding of MS progression, including subtle indicators like smell changes, could lead to more effective strategies for managing this challenging condition.
Olfactory Tests
A variety of tests are used to assess olfactory function. These tests typically present a series of odors, and the patient identifies the scents. The Sniffin’ Sticks test is a commonly used tool. This test involves a series of odorants, each presented to one nostril at a time, and the patient identifies the odors. The results are scored based on the patient’s ability to correctly identify the odors.
Questionnaires
Olfactory questionnaires are self-reported assessments that gauge the patient’s perception of their sense of smell. These questionnaires often include questions about the ability to detect common odors, changes in smell over time, and any perceived distortions in smell. The University of Pennsylvania Smell Identification Test (UPSIT) is an example of a widely used questionnaire. The results from these questionnaires can be used to complement objective olfactory tests.
Potential Mechanisms Linking Smell Changes to MS Progression
The intricate relationship between the sense of smell and the progression of Multiple Sclerosis (MS) is a fascinating area of ongoing research. While the exact mechanisms are not fully understood, emerging evidence suggests a potential link between olfactory dysfunction and the underlying inflammatory and degenerative processes characteristic of MS. This exploration delves into the possible pathways connecting these two seemingly disparate aspects of neurological health.The olfactory system, responsible for our sense of smell, is intimately connected to other brain regions involved in MS pathology.
Damage to this system could be a reflection of broader neurological deterioration, potentially providing valuable insights into the disease’s progression. Understanding the potential mechanisms involved is crucial for developing more effective diagnostic tools and potentially new therapeutic strategies.
Potential Inflammatory and Degenerative Processes
The immune system’s attack on the myelin sheath, the protective covering around nerve fibers, is a hallmark of MS. This demyelination process can disrupt the normal functioning of nerve pathways, leading to a range of neurological symptoms. The olfactory bulb, a crucial component of the olfactory system, is particularly vulnerable to these inflammatory processes. Chronic inflammation in this area can directly damage olfactory receptor neurons and disrupt the intricate neural circuits responsible for smell perception.
This inflammatory response may also indirectly affect other brain regions through the body’s immune response. Furthermore, ongoing inflammation can contribute to oxidative stress, which plays a significant role in the progression of MS.
Role of Oxidative Stress and Neuroinflammation
Oxidative stress, characterized by an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to neutralize them, is a key player in MS pathogenesis. This imbalance can damage neuronal structures, including the olfactory bulb, potentially leading to olfactory dysfunction. Neuroinflammation, the immune response within the central nervous system, is also strongly linked to MS progression.
Recent studies suggest a loss of smell might be an early indicator of Multiple Sclerosis (MS) progression. This fascinating link between olfactory function and neurological conditions is intriguing, but what about the surprising connection to things like sugar-free gummy bears laxatives? While the connection between these two seemingly disparate subjects might seem tenuous, understanding the complex interplay of bodily systems is crucial.
The research on how these unusual digestive aids could indirectly influence the nervous system is ongoing. Ultimately, a diminished sense of smell could still be a valuable early warning sign for MS. Sugar free gummy bears laxatives might have an indirect role, but the primary focus remains on the vital role of the sense of smell in diagnosing potential MS.
The inflammatory cascade can further exacerbate oxidative stress, creating a vicious cycle of damage to nerve cells and supporting structures, potentially including the olfactory system.
Mechanisms of Axonal Damage and Demyelination
Axonal damage and demyelination are crucial features of MS. Axonal degeneration, the loss of nerve fibers, is believed to contribute significantly to the progressive nature of MS symptoms. The olfactory system, with its intricate network of axons, may be susceptible to these damaging processes. Demyelination, the breakdown of the myelin sheath, can disrupt the efficient transmission of signals along these axons, potentially impairing olfactory function.
The extent of axonal damage and demyelination may vary across individuals, correlating with the severity of olfactory dysfunction and overall MS disease progression.
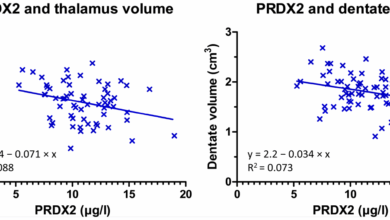
Current Research Findings on the Connection Between Olfactory Function and MS Disease Activity
Studies investigating the relationship between olfactory function and MS disease activity are ongoing. Early research suggests a correlation between reduced olfactory function and higher disease activity measures, including brain lesions observed on MRI scans. However, the specific mechanisms underlying this correlation remain to be fully elucidated. Further research is needed to determine if olfactory testing could serve as a useful biomarker for MS disease activity and progression.
Future studies could explore the potential of olfactory dysfunction as an early indicator of MS progression, providing a window into the disease’s trajectory.
Potential Diagnostic and Prognostic Value of Smell Changes
The sense of smell, often overlooked, plays a surprisingly crucial role in our overall health and well-being. Its connection to neurological function is well-established, and emerging research suggests a potential link between olfactory dysfunction and the progression of multiple sclerosis (MS). This opens up exciting possibilities for using smell changes as a diagnostic and prognostic tool in MS.Early detection and accurate prediction of MS progression are paramount for timely intervention and improved patient outcomes.
Current clinical markers, while helpful, may not always capture the subtle shifts in disease activity. Olfactory dysfunction, potentially reflecting underlying neurological damage, could offer a valuable complementary approach.
Olfactory Dysfunction as a Marker for MS Progression
Olfactory dysfunction, or hyposmia (reduced sense of smell), is a common neurological symptom reported by MS patients. Studies have shown a correlation between the severity of olfactory impairment and disease duration or disability. This suggests that olfactory tests might serve as an indicator of ongoing or worsening MS-related damage. Furthermore, the specific patterns of olfactory loss could potentially provide insights into the specific areas of the nervous system affected.
This specificity is important for distinguishing MS from other neurological conditions with similar symptoms.
Predictive Value of Olfactory Tests Compared to Other Clinical Markers
Several clinical markers are currently used to assess MS progression, including Expanded Disability Status Scale (EDSS) scores, MRI scans, and cerebrospinal fluid (CSF) analysis. While these markers provide valuable information, olfactory tests may offer a unique perspective. For instance, olfactory tests can potentially detect subtle neurological damage earlier than other markers, providing an opportunity for earlier intervention. This early detection could allow for more targeted therapies and improved disease management.
The predictive value of olfactory tests will need to be rigorously evaluated in comparison to existing clinical markers in large-scale clinical trials.
Potential of Olfactory Assessments for Monitoring Disease Activity and Treatment Response
Regular olfactory assessments could potentially provide valuable insights into the dynamic nature of MS. Monitoring olfactory function over time could help gauge disease activity and the efficacy of treatment strategies. For example, a reduction in olfactory dysfunction following a new treatment could indicate a positive response, while persistent or worsening impairment could suggest the need for adjustments to the treatment plan.
This real-time monitoring could lead to more personalized and effective management of MS.
Strengths and Weaknesses of Using Smell Changes as a Biomarker
| Strengths | Weaknesses |
|---|---|
| Potentially detects subtle neurological damage earlier than other markers. | Standardization of olfactory testing methods is still evolving, which could affect the reliability of results. |
| Could provide a more dynamic assessment of disease activity compared to static assessments. | The correlation between olfactory dysfunction and MS progression may not be uniform across all patients, requiring careful stratification and analysis. |
| Relatively inexpensive and non-invasive compared to some other diagnostic tests. | The exact mechanisms linking olfactory dysfunction to MS progression are not fully understood. |
| Could facilitate more personalized and effective disease management. | Further research is needed to validate the predictive value of olfactory tests in different MS subtypes and disease stages. |
Future Directions and Research Needs: Sense Of Smell Could Be A Signal Of Ms Progression
The potential link between olfactory dysfunction and MS progression warrants further investigation. Understanding this connection could lead to earlier diagnosis, more effective monitoring of disease activity, and potentially, novel therapeutic targets. This exploration necessitates a multifaceted approach, combining rigorous research designs, innovative diagnostic tools, and a careful consideration of the ethical implications.The existing research provides a foundation for future exploration, but critical gaps remain in our understanding of the precise mechanisms driving this link.
Further studies are needed to confirm and expand upon the observations made thus far, laying the groundwork for the development of improved diagnostic and therapeutic strategies.
Key Areas for Future Research
To fully elucidate the complex relationship between smell changes and MS progression, several key areas require focused research efforts. These include investigating the specific olfactory pathways and neural circuits affected in MS, exploring the potential role of inflammation and demyelination in olfactory dysfunction, and examining the correlation between the severity of olfactory impairment and the rate of MS progression.
These studies will provide a more complete picture of the underlying mechanisms and help to identify potential biomarkers for disease activity.
Development of Novel Diagnostic Tools
The identification of reliable and accessible diagnostic tools is crucial for early detection and monitoring of MS. Olfactory testing could be incorporated into existing MS diagnostic protocols. This involves developing standardized olfactory tests that are sensitive enough to detect subtle changes and are readily applicable in clinical settings. Further research into the use of advanced neuroimaging techniques, such as functional MRI (fMRI) and diffusion tensor imaging (DTI), could provide additional insights into the neural correlates of olfactory dysfunction in MS.
This integration could improve diagnostic accuracy and allow for a more comprehensive assessment of disease activity.
Development of Therapeutic Strategies Targeting the Olfactory System
Investigating the potential for olfactory-targeted therapies in MS is another important area of research. These strategies might involve the development of compounds that promote olfactory nerve regeneration or protect against further damage. Identifying specific molecular targets associated with olfactory dysfunction in MS patients could pave the way for the development of targeted therapies. This approach could not only improve olfactory function but also potentially slow or halt MS progression.
Ethical Considerations
The use of smell as a diagnostic tool for MS raises several ethical considerations. Ensuring patient autonomy and informed consent is paramount. Clinicians must be transparent about the limitations and potential benefits of such testing. Equally important is the need for equitable access to olfactory testing and potential therapies, avoiding exacerbating existing health disparities. Careful consideration must be given to potential stigmatization and psychological impacts associated with a diagnosis based on olfactory testing.
Research Study: Investigating the Potential Link Between Smell Changes and MS Progression
| Study Objective | Methodology | Expected Outcomes |
|---|---|---|
| To determine the correlation between the severity of olfactory impairment and the rate of MS progression. | Recruit a cohort of MS patients at various disease stages. Administer standardized olfactory tests at baseline and at regular intervals. Assess MS progression using established clinical scales (e.g., Expanded Disability Status Scale – EDSS) and MRI scans. | Establish a statistically significant correlation between olfactory dysfunction and MS progression. Identify potential olfactory biomarkers for disease activity. Evaluate the predictive value of olfactory tests for future disease progression. |
Last Word

In conclusion, the connection between olfactory dysfunction and MS progression warrants further investigation. While current research suggests a potential link, more rigorous studies are needed to solidify this connection and explore its potential clinical implications. Olfactory testing could potentially provide a valuable tool for monitoring disease activity and treatment response in MS. This could lead to earlier diagnoses and more personalized treatment approaches.
The potential diagnostic and prognostic value of olfactory dysfunction as a marker for MS progression remains an exciting area of research, promising a deeper understanding of MS and potentially paving the way for innovative treatments.