Should people with anorexia be force fed – Should people with anorexia be force-fed? This complex question sparks intense debate, raising critical ethical, medical, and psychological concerns. The decision to intervene with force-feeding in cases of anorexia nervosa is fraught with dilemmas, requiring careful consideration of the patient’s autonomy, potential risks, and alternative treatment options.
This exploration delves into the multifaceted nature of this issue, examining the ethical principles surrounding medical interventions, the potential medical complications and benefits, the psychological impact on the patient, and alternative treatment approaches. It also considers the cultural and societal factors influencing eating disorders and the legal frameworks governing such interventions. The aim is to provide a comprehensive overview of the issue, encouraging a nuanced understanding rather than a simple yes-or-no answer.
Ethical Considerations of Force-Feeding
The ethical implications of force-feeding individuals with anorexia nervosa are complex and deeply intertwined with fundamental principles of medical ethics. Decisions surrounding this intervention necessitate careful consideration of patient autonomy, potential benefits and harms, and the broader societal context. Force-feeding, while potentially life-saving, raises significant questions about the balance between medical intervention and individual rights.Medical interventions like force-feeding in cases of anorexia nervosa present a complex interplay of ethical principles.
Understanding these principles is crucial to navigating the challenges involved in providing appropriate care. A critical analysis requires examining the core values at stake and acknowledging the potential conflicts that arise when these values clash.
Ethical Principles in Medical Interventions
Medical interventions, including force-feeding, must adhere to established ethical principles. These principles, often interwoven, guide healthcare professionals in making decisions that respect patient well-being and autonomy while maintaining the integrity of the medical profession.
The debate around forcing food on someone with anorexia is complex. It’s a tough issue, and while some might think it’s the right approach, it’s crucial to consider the long-term well-being of the individual. Thankfully, resources like best foster parent blogs highlight the importance of understanding and supporting those in need, especially when dealing with complex mental health conditions.
Ultimately, forcing food isn’t the solution, but rather a more compassionate, holistic approach is necessary to address the root causes of the eating disorder.
- Autonomy: Respect for patient autonomy emphasizes the individual’s right to self-determination and decision-making regarding their own medical care. In cases of anorexia nervosa, respecting autonomy means recognizing the patient’s right to refuse treatment, even if that refusal might seem detrimental to their health.
- Beneficence: This principle compels healthcare professionals to act in the patient’s best interests. In the context of force-feeding, beneficence suggests that the intervention should aim to maximize the patient’s well-being and improve their health outcomes. However, the potential for harm associated with force-feeding must be carefully weighed against potential benefits.
- Non-maleficence: This principle emphasizes avoiding harm to the patient. Force-feeding, while intended to be beneficial, carries potential risks, including physical discomfort, psychological distress, and potential complications related to the procedure itself. Carefully assessing these potential risks and minimizing them is paramount.
- Justice: This principle demands fairness and equitable distribution of resources and care. In the context of force-feeding, justice considerations include ensuring that the intervention is applied consistently and fairly across all patients with anorexia nervosa, regardless of their socioeconomic status or other factors.
Conflicts in Ethical Principles
Ethical conflicts arise when principles like autonomy and beneficence clash. In anorexia nervosa, the patient’s refusal of treatment, rooted in their distorted body image and disordered eating, directly opposes the healthcare professional’s desire to restore their health. Resolving these conflicts requires a nuanced approach that considers the specific circumstances of each patient.
Healthcare Professionals’ Obligations vs. Patient Rights
The ethical obligations of healthcare professionals, including those related to patient safety and well-being, must be balanced against the patient’s right to self-determination and autonomy. These obligations often present a delicate dance where the professional’s responsibility to act in the patient’s best interest must be reconciled with the patient’s right to make choices about their own body and treatment.
Informed Consent and Vulnerability
Informed consent is a cornerstone of ethical medical practice. It involves providing the patient with sufficient information about the proposed intervention, including potential benefits and risks, to enable them to make an informed decision. However, individuals with anorexia nervosa might be vulnerable or unable to fully grasp the implications of their choices due to the illness. Assessing the patient’s capacity for decision-making and ensuring that the information is presented in a way they can understand is crucial.
Ethical Dilemmas in Force-Feeding
Real-life ethical dilemmas surrounding force-feeding in anorexia nervosa cases frequently involve patients who resist treatment, creating a conflict between their autonomy and the healthcare team’s desire to improve their health. For instance, a patient might refuse nutrition despite showing signs of severe malnutrition, presenting a difficult ethical decision-making process.
The debate around forcing food on individuals with anorexia is incredibly complex. It’s a situation where the well-being of the person is paramount, and while some might argue for intervention, there’s a real need for understanding. This brings up another issue with products like CBD; a growing concern regarding mislabeling is present in the market, with some products containing THC, which is a psychoactive compound.
For more information on this issue of cbd products often mislabeled some containing thc what to know , it’s important to know the potential dangers of these mislabeled products. Ultimately, the decision to force feed someone with anorexia is a medical one, requiring careful consideration and a deep understanding of the patient’s needs.
Ethical Frameworks and Force-Feeding
| Ethical Framework | View on Force-Feeding | Justification |
|---|---|---|
| Deontological | Generally opposed unless necessary to prevent immediate harm. | Focuses on duties and rules, prioritizing patient autonomy and refusal of treatment. |
| Consequentialist | May be permissible if the potential benefits outweigh the risks and potential harms. | Considers the overall outcome and focuses on maximizing positive outcomes. |
Medical Risks and Benefits of Force-Feeding: Should People With Anorexia Be Force Fed
Force-feeding, a controversial intervention in treating anorexia nervosa, presents a complex interplay of potential risks and benefits. While the goal is to restore nutritional balance and prevent further health deterioration, the procedure carries significant medical complications that must be carefully weighed against the potential gains. The decision to implement force-feeding requires a thorough understanding of these potential outcomes and a personalized approach that prioritizes the patient’s well-being.Force-feeding, in cases of severe malnutrition, can be a necessary measure to stabilize the patient’s health.
However, it’s crucial to recognize that the procedure is not without its dangers. Medical professionals must meticulously consider the potential risks and benefits, along with the patient’s unique circumstances, to create a treatment plan that maximizes positive outcomes and minimizes harm.
Potential Medical Complications
Force-feeding, even when conducted by medical professionals, can lead to a variety of complications, particularly affecting the gastrointestinal system. The sudden introduction of large volumes of food can overwhelm the digestive system, leading to nausea, vomiting, abdominal pain, and even esophageal tears. In severe cases, aspiration pneumonia, a potentially life-threatening condition, can occur if food is inhaled into the lungs.
Dehydration, electrolyte imbalances, and infections are also possible consequences. The risk of these complications increases with the severity of malnutrition and the speed of refeeding.
Potential Benefits of Force-Feeding
Force-feeding can be crucial in restoring nutritional balance and preventing further health deterioration. It can rapidly increase calorie and nutrient intake, preventing further loss of muscle mass and vital organ function. This is particularly important in cases where the patient is unable to consume sufficient calories through other means. Early intervention through force-feeding can be vital in stabilizing the patient’s condition and setting the stage for other therapies to be effective.
However, the benefits must be carefully balanced against the potential risks.
Importance of Individualized Treatment Plans
Force-feeding should never be a blanket approach. A personalized treatment plan is essential, taking into account the patient’s specific medical needs, the severity of their malnutrition, and their psychological state. The rate of refeeding must be gradual and closely monitored to minimize the risk of complications. Factors like the patient’s pre-existing health conditions, the presence of other psychological issues, and the patient’s ability to cooperate with the treatment plan must be meticulously considered.
Successful outcomes hinge on a comprehensive approach.
Comparison with Other Therapeutic Approaches
Compared to other therapies for anorexia, force-feeding can be a necessary intervention in severe cases of malnutrition. Nutritional counseling and support groups are often part of a comprehensive treatment plan. However, in cases where the patient is unable to eat, or where the level of malnutrition is critical, force-feeding might be a vital tool to support the patient’s recovery.
Examples of Successful and Unsuccessful Force-Feeding Interventions
“Case studies have shown that force-feeding, when conducted carefully and gradually, can be effective in stabilizing a patient’s condition and restoring nutritional balance, enabling the patient to then participate in other therapeutic approaches. However, if the refeeding is too rapid or not managed properly, it can lead to severe complications, requiring further interventions and potentially delaying recovery.”
The success of force-feeding depends heavily on the patient’s individual response, the medical team’s expertise, and the careful monitoring of the patient’s condition. Factors such as the patient’s willingness to cooperate, the presence of any pre-existing health issues, and the overall treatment approach all play a critical role.
Table: Potential Short-Term and Long-Term Medical Risks and Benefits of Force-Feeding
| Aspect | Short-Term Risks | Short-Term Benefits | Long-Term Risks | Long-Term Benefits |
|---|---|---|---|---|
| Gastrointestinal Tract | Nausea, vomiting, abdominal pain, esophageal tears, aspiration pneumonia | Rapid restoration of caloric intake | Potential for chronic digestive issues | Improved nutrient absorption |
| Overall Health | Electrolyte imbalances, dehydration, infections | Stabilization of vital signs, prevention of further deterioration | Potential for organ damage | Improved overall health status, allowing for further therapies |
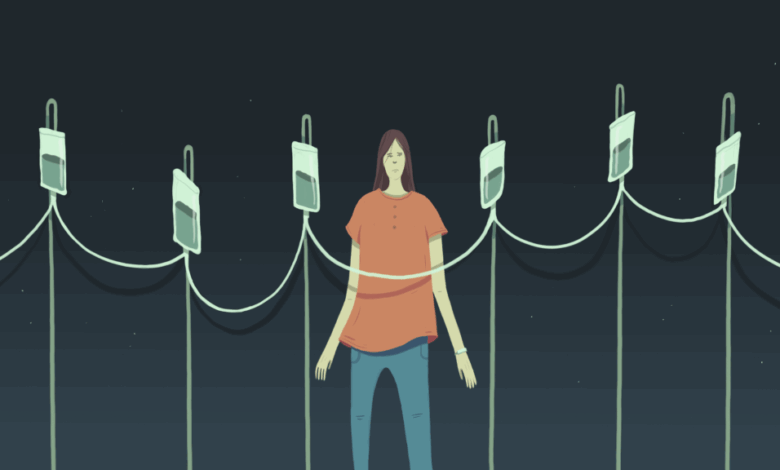
Psychological Impact of Force-Feeding

Force-feeding, a controversial intervention for individuals with anorexia nervosa, carries significant potential for psychological harm. Beyond the immediate physical discomfort, the act of being forced to consume food can profoundly impact a patient’s self-esteem, body image, and overall well-being, potentially exacerbating pre-existing anxieties and fostering feelings of control and powerlessness. Understanding these psychological ramifications is crucial in evaluating the ethical and therapeutic implications of this approach.Force-feeding, while aimed at restoring physical health, can inadvertently create a deeply negative psychological environment.
This environment often undermines the trust between patient and healthcare provider, fostering feelings of violation and distrust. A crucial consideration is the potential for this intervention to further entrench the patient’s disordered eating patterns and body image distortions. It’s essential to recognize that a patient’s psychological state significantly influences the efficacy of any intervention, including force-feeding.
Impact on Self-Esteem and Body Image
Force-feeding can severely damage a patient’s self-esteem. The experience of having food forced upon them can lead to feelings of shame, powerlessness, and a profound loss of control over their own bodies. This, in turn, can significantly impact their body image, potentially worsening their distorted perceptions and anxieties surrounding food and weight. A patient who feels their autonomy is constantly undermined may struggle to trust the intentions of those around them, which could hinder their engagement in subsequent therapeutic interventions.
This diminished trust can lead to increased resistance and decreased cooperation with future treatments.
Exacerbation of Control and Powerlessness
The inherent power imbalance inherent in force-feeding can exacerbate feelings of control and powerlessness in the patient. The act of having food forced into their system directly challenges their perceived ability to manage their own bodies and eating habits. This can lead to heightened anxiety, anger, and resentment. The patient might internalize the message that their choices and desires are insignificant, reinforcing the very patterns that contribute to their eating disorder.
Comparison with Alternative Interventions
Force-feeding is often contrasted with other approaches, such as psychotherapy and nutritional counseling. These alternative methods focus on addressing the underlying psychological and emotional factors contributing to the eating disorder. They empower patients to develop healthier coping mechanisms and a more positive relationship with food and their bodies. Therapy aims to understand the root causes of the eating disorder and build strategies for long-term change, in contrast to the immediate, often forceful approach of force-feeding.
Influence of Psychological State on Intervention Success
A patient’s psychological state significantly influences the outcome of any intervention, including force-feeding. Patients who are experiencing high levels of anxiety, depression, or feelings of hopelessness may react negatively to force-feeding, potentially increasing their resistance and hindering progress. Conversely, patients who are receptive to therapy and demonstrate a willingness to engage in treatment are more likely to respond positively to more supportive and collaborative approaches.
Examples of Violation and Trauma
Force-feeding can create feelings of violation and trauma, especially when carried out without the patient’s informed consent or understanding. The experience can be perceived as a violation of bodily autonomy and personal boundaries, leading to lasting psychological distress. Instances where the patient feels a lack of control over their own bodies and choices can lead to long-term emotional scarring.
Furthermore, the lack of trust that develops from such procedures can hinder future progress in treatment.
Psychological Impact on Different Patient Populations
| Patient Population | Potential Psychological Impacts |
|---|---|
| Adolescents | Increased feelings of shame, social isolation, and potential for peer-related stigma. A greater vulnerability to negative body image and potential for future trauma. |
| Young Adults | Potentially increased feelings of resentment and anger. Greater risk of developing trust issues and difficulties in forming healthy relationships. |
| Adults | Potentially increased feelings of helplessness and loss of control. Increased potential for emotional and behavioral withdrawal, impacting overall well-being. |
Alternative Treatment Approaches

Anorexia nervosa is a complex eating disorder that requires a multifaceted approach to treatment. While force-feeding is a controversial and often ineffective method, alternative approaches prioritize the patient’s well-being and autonomy. These methods aim to address the underlying psychological and emotional factors contributing to the disorder, fostering a sustainable recovery rather than merely suppressing symptoms. A comprehensive treatment plan integrating various therapies can significantly improve outcomes and create a supportive environment for recovery.
Psychotherapy Approaches
Psychotherapy plays a crucial role in addressing the root causes of anorexia. Different types of therapy can be effective in helping individuals understand their relationship with food, body image, and emotions. Cognitive Behavioral Therapy (CBT) is frequently used to identify and modify negative thought patterns and behaviors related to eating. Dialectical Behavior Therapy (DBT) helps individuals develop coping mechanisms for difficult emotions and improve interpersonal relationships.
Family-based therapy, in particular, often proves beneficial by engaging family members in the treatment process, fostering support and promoting healthy communication patterns.
Nutritional Counseling
Nutritional counseling is essential for restoring a healthy relationship with food. A registered dietitian or nutritionist can provide personalized guidance on creating a balanced meal plan that meets the individual’s nutritional needs while promoting a healthy relationship with food. This process helps patients understand the importance of nutrition for overall well-being, moving away from restrictive eating patterns. Crucially, the goal is not to impose specific food choices but to foster understanding and autonomy in food choices.
Family Therapy
Family-based therapy (FBT) is often a cornerstone of anorexia treatment, particularly for adolescents. This approach involves the entire family in the therapeutic process, addressing family dynamics, communication patterns, and the impact of the eating disorder on the family unit. It encourages open communication and fosters a supportive environment where the individual can gradually re-engage with food and normal eating habits.
FBT often shows positive results due to the active involvement of the family in the recovery process.
Comprehensive Treatment Plan Integration
A comprehensive treatment plan should integrate psychotherapy, nutritional counseling, and family therapy. These approaches are not mutually exclusive; rather, they complement each other. For example, nutritional counseling can provide the necessary tools to understand food and nutrition, which can then be further explored in psychotherapy sessions. Family therapy helps create a supportive environment for implementing these changes.
Therapists should collaborate closely to create a coordinated and individualized treatment plan, ensuring consistency and addressing specific needs.
Addressing Resistance to Traditional Treatment
Individuals with anorexia may be resistant to traditional treatment methods due to deeply ingrained anxieties and beliefs. A key aspect of effective treatment involves building trust and rapport with the patient. Empathy, patience, and understanding are essential in creating a safe space for exploration and change. The therapist should actively listen to the patient’s concerns and address them with sensitivity and respect.
Restoring Positive Relationship with Food and Addressing Underlying Issues
Alternative approaches can help restore a positive relationship with food by challenging distorted body image perceptions and negative thought patterns. By addressing the underlying psychological issues, these approaches can help individuals develop healthier coping mechanisms and improve their overall well-being. This holistic approach aims to foster a sustainable recovery by nurturing a positive relationship with food and self-esteem, rather than relying on restrictive measures.
Table of Alternative Treatment Approaches
| Treatment Approach | Brief Description |
|---|---|
| Cognitive Behavioral Therapy (CBT) | Identifies and modifies negative thought patterns and behaviors related to eating. |
| Dialectical Behavior Therapy (DBT) | Develops coping mechanisms for difficult emotions and improves interpersonal relationships. |
| Family-Based Therapy (FBT) | Involves the entire family in the therapeutic process, addressing family dynamics and promoting healthy communication. |
| Nutritional Counseling | Provides personalized guidance on creating a balanced meal plan that meets nutritional needs. |
Cultural and Societal Factors
The pressures of our modern world, particularly those surrounding body image and societal ideals, often play a significant role in the development and perpetuation of eating disorders like anorexia nervosa. These factors can influence not only the initial onset of the disorder but also the individual’s willingness to seek help and the effectiveness of treatment approaches. Understanding the cultural and societal context is crucial for developing compassionate and effective strategies to address this complex issue.Cultural attitudes towards body image significantly impact the treatment approaches for anorexia.
In societies that prioritize thinness, individuals with anorexia may face pressure to conform to these ideals, leading to difficulties in accepting and addressing the underlying issues that contribute to their eating disorder. This, in turn, can affect the effectiveness of treatment interventions, as patients might struggle with the perceived conflict between their cultural values and the need for healing.
A critical element in effective treatment is addressing these cultural influences alongside the psychological and medical aspects of the disorder.
Cultural Attitudes Towards Body Image and Eating Disorders
Cultural ideals about beauty and body shape vary widely across societies and evolve over time. These norms can significantly influence how individuals perceive themselves and their bodies. In some cultures, thinness is highly valued, leading to a greater risk of developing eating disorders. Conversely, in cultures that prioritize larger body sizes, the risk factors may be different. For example, a cultural emphasis on curvaceousness can, paradoxically, create pressures on individuals to conform to an ideal body shape that might lead to disordered eating.
Influence of Societal Pressures on Treatment Approaches
Societal pressures can significantly impact the treatment approaches for anorexia. The stigma associated with eating disorders can discourage individuals from seeking help. For instance, fear of judgment from family, friends, or the community can prevent individuals from disclosing their struggles. This reluctance to seek help often results in prolonged illness and can make recovery more challenging. Treatment programs need to address this stigma by promoting understanding and acceptance.
Open dialogue about eating disorders and the provision of supportive environments are crucial for successful interventions.
Stigma Associated with Eating Disorders and Treatment Decisions
The stigma surrounding eating disorders is a significant barrier to effective treatment. This stigma manifests in various forms, including negative stereotypes, misunderstandings, and social isolation. These factors can contribute to feelings of shame, guilt, and self-criticism in individuals with eating disorders, making it more difficult for them to acknowledge their illness and seek help. Consequently, individuals may delay or avoid treatment, potentially leading to more severe complications.
Furthermore, the stigma can influence family and friends’ responses to the individual’s condition, exacerbating the problem. A crucial aspect of addressing this issue is to promote greater understanding and empathy towards individuals with eating disorders.
Societal Norms and Expectations Affecting Help-Seeking Behavior
Societal norms and expectations can influence the willingness of individuals to seek help for anorexia. Individuals may fear the judgment or disapproval of others if they disclose their struggles with an eating disorder. In some cultures, mental health issues are often stigmatized, making it even harder for individuals to reach out for support. Furthermore, societal pressures to maintain a certain image can contribute to feelings of inadequacy and shame, discouraging help-seeking behavior.
Addressing these factors through education and destigmatization efforts is essential to encourage help-seeking.
The question of whether people with anorexia should be force-fed is a complex one, deeply rooted in ethical dilemmas. It’s a similar debate to the ongoing fight for reproductive rights, where, like in the case of abortion opponents emboldened trump administration actions , a certain group’s strong beliefs clash with individual autonomy. Ultimately, forcing someone to eat against their will raises serious concerns about bodily autonomy, and the ethical line between intervention and violation.
The potential for physical and psychological harm must be carefully considered.
Cultural Influences on the Acceptability of Force-Feeding
Cultural beliefs and norms play a crucial role in determining the acceptability of force-feeding as a treatment option. In cultures where the individual’s autonomy is highly valued, force-feeding is often viewed as unethical and unacceptable. Conversely, in cultures where there is less emphasis on individual rights, the practice might be considered more acceptable. Understanding the cultural context is paramount in making informed decisions about treatment options for individuals with eating disorders.
It’s important to emphasize that force-feeding is rarely a sustainable or ethical solution, as it often fails to address the underlying psychological and emotional factors that contribute to the disorder.
Impact of Cultural Norms on Body Image and Eating Disorders
| Cultural Norm | Impact on Body Image | Impact on Eating Disorders |
|---|---|---|
| Thinness is highly valued | Increased pressure to be thin, body dissatisfaction | Higher risk of anorexia, body dysmorphia |
| Curvaceousness is idealized | Pressure to conform to specific body shapes, body dissatisfaction | Potential for disordered eating, body image issues |
| Larger body sizes are accepted | Reduced pressure to conform to specific body shapes | Lower risk of anorexia, body image issues might be related to other factors |
| Emphasis on physical appearance | Increased focus on appearance, body scrutiny | Higher risk of body dissatisfaction, eating disorders |
Legal and Regulatory Frameworks
Navigating the complex landscape of medical interventions, especially those involving potentially controversial procedures like force-feeding, necessitates a strong understanding of legal and regulatory frameworks. These frameworks aim to protect patient rights while ensuring appropriate medical care. The interplay between ethical considerations and legal requirements is crucial in cases of anorexia nervosa, where the patient’s autonomy and well-being are paramount.Force-feeding, a highly sensitive procedure, is governed by a multitude of laws and regulations, primarily designed to protect vulnerable individuals and ensure medical professionals act responsibly.
The specific application of these laws can vary significantly depending on the jurisdiction, highlighting the need for a nuanced understanding of the legal landscape in each particular context.
Legal Considerations Surrounding Force-Feeding
The legal considerations surrounding force-feeding in cases of anorexia nervosa are intricate and often hinge on the patient’s capacity to consent. In situations where a patient lacks the capacity to make decisions about their own medical care, legal guardians or court orders may be required to authorize interventions. This underscores the importance of a thorough assessment of the patient’s mental capacity and the involvement of relevant legal authorities.
Medical Professional’s Role in Adherence to Legal and Regulatory Guidelines
Medical professionals play a critical role in upholding legal and regulatory guidelines when considering force-feeding. They must thoroughly document the patient’s condition, including their capacity to consent or refusal of treatment. This documentation forms a crucial component of any legal proceedings related to the intervention. Professionals should also consult with legal counsel to ensure their actions comply with relevant laws and regulations.
Interplay of Ethical and Legal Considerations, Should people with anorexia be force fed
Ethical considerations often intertwine with legal requirements in cases of force-feeding. While ethical principles emphasize patient autonomy and beneficence, legal frameworks may require interventions in situations where the patient’s actions pose a direct threat to their health or life. This delicate balance necessitates careful consideration and collaboration between medical professionals, legal experts, and potentially, ethics committees.
Table Outlining Legal and Regulatory Aspects of Force-Feeding
| Aspect | Description |
|---|---|
| Patient Capacity | Assessment of the patient’s ability to make informed decisions regarding medical interventions, including force-feeding. |
| Informed Consent | The legal requirement that patients must understand and agree to a medical intervention, or in cases of incapacity, a legal guardian or court order is needed. |
| Court Orders | Legal documents authorizing medical interventions when a patient lacks the capacity to consent. |
| Documentation | Thorough medical records documenting the patient’s condition, including attempts to obtain informed consent and the rationale for the intervention. |
| Legal Representation | Potential need for legal counsel to ensure compliance with relevant laws and regulations during the force-feeding process. |
Closing Summary
Ultimately, the decision regarding force-feeding in anorexia nervosa cases demands a holistic approach. While potentially beneficial in restoring nutritional balance, the potential for psychological harm and violation must be carefully weighed against the risks of inaction. The exploration of alternative treatments, the recognition of cultural and societal influences, and adherence to robust ethical guidelines are crucial for developing a compassionate and effective treatment strategy.
This complex issue requires a deep understanding of the individual’s needs, their autonomy, and the well-being that should always be at the forefront of any intervention.
