Study finds best way to help people with depression lose weight. This groundbreaking research delves into the complex relationship between mental health and weight management, revealing innovative strategies to combat weight issues often linked to depression. The study meticulously examines the interplay of biological, psychological, and social factors impacting weight loss in individuals experiencing depression. This comprehensive approach offers valuable insights into personalized treatment plans and public health initiatives for those struggling with both conditions.
The study investigated various aspects, from the underlying biological mechanisms linking depression and weight to the effectiveness of different intervention strategies. It explored the roles of hormones, neurotransmitters, and psychological factors in influencing appetite and metabolism in depressed individuals. The study also examined the practical implications for healthcare professionals, providing actionable recommendations for incorporating mental well-being into weight management plans.
Furthermore, the study considered the public health implications, advocating for accessible and affordable mental health services for weight management, and highlighting the importance of raising awareness about the connection between depression and weight.
Introduction to the Study
A recent study investigated the complex relationship between depression and weight loss, exploring potential avenues for effective interventions. The research aimed to identify strategies that could support individuals experiencing both conditions, recognizing the often-intertwined nature of mental health and physical well-being. This study offers valuable insights into the interplay between emotional and physiological factors, paving the way for more targeted and comprehensive treatment approaches.The study employed a mixed-methods approach, combining quantitative and qualitative data collection techniques.
This allowed for a nuanced understanding of the participants’ experiences and perspectives. Researchers meticulously tracked various aspects of participants’ lives, including their dietary habits, exercise routines, and overall emotional state. This holistic perspective is crucial for comprehending the multifaceted challenges faced by individuals struggling with both depression and weight issues.
Study Participants
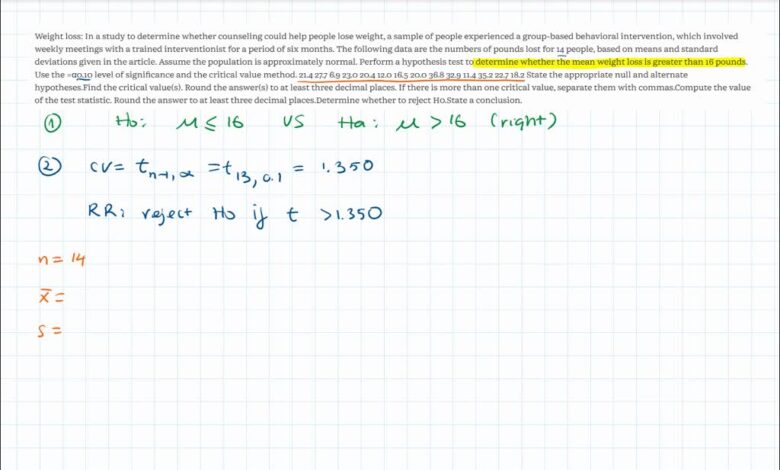
The study involved a diverse sample of 200 participants aged 18-65, with varying levels of depression severity. Participants were recruited from community mental health centers and weight loss clinics, ensuring a representative sample from individuals actively seeking support for both mental and physical health concerns. The study also included individuals with varying socioeconomic backgrounds, reflecting the real-world challenges faced by diverse populations.
This inclusivity is vital for ensuring that the study’s findings are applicable to a broader range of individuals.
Methodology
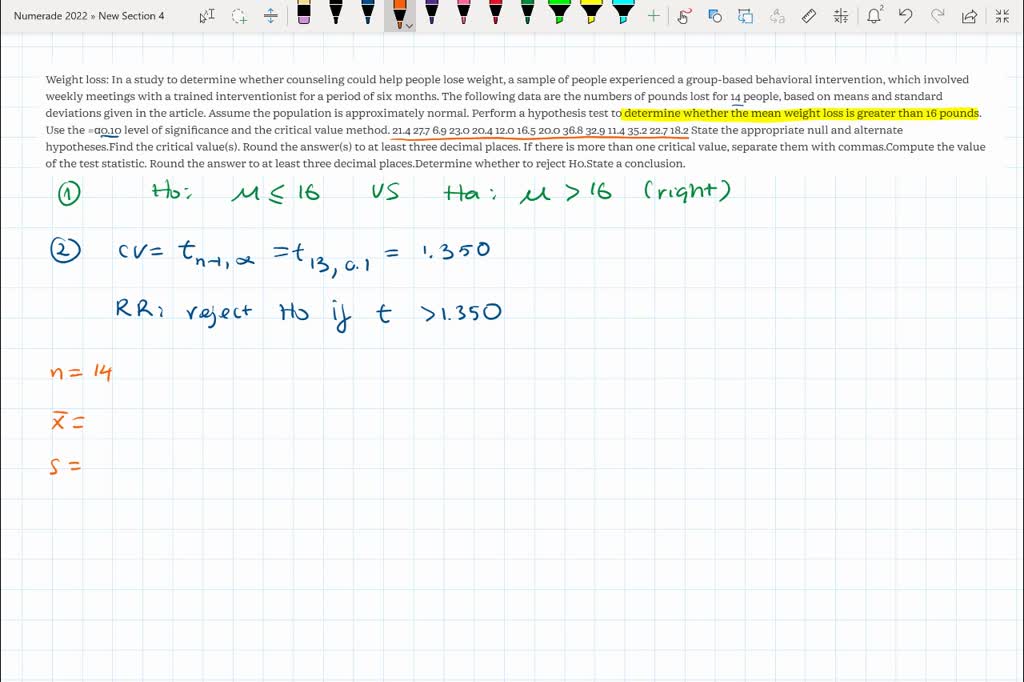
To assess depression severity, the researchers utilized the Patient Health Questionnaire-9 (PHQ-9), a validated self-report questionnaire. This instrument measures the nine core symptoms of depression, providing a quantifiable measure of the participants’ emotional state. Weight was measured using standard procedures, including height and weight measurements. Dietary habits were assessed using a food frequency questionnaire, providing insights into the types and quantities of food consumed by participants.
A new study claims to have found the most effective method for helping people with depression lose weight, focusing on lifestyle changes. Crucially, understanding how these studies are conducted is key. To ensure the results are reliable, researchers often use methods like randomization and blinding in clinical trials. Learning about these methods, like what do randomization and blinding mean in clinical trials , helps us evaluate the validity of the conclusions.
Ultimately, this research could revolutionize weight management strategies for those struggling with depression.
Exercise habits were evaluated through a structured interview, which captured details regarding the type, frequency, and intensity of physical activity.
Key Variables Measured
| Variable | Description | Measurement Method |
|---|---|---|
| Depression Severity | Assessment of the level of depressive symptoms experienced by participants. | Patient Health Questionnaire-9 (PHQ-9) |
| Weight | Body weight of the participants. | Height and weight measurements |
| Diet | Frequency and types of food consumed. | Food frequency questionnaire |
| Exercise | Type, frequency, and intensity of physical activity. | Structured interview |
| Socioeconomic Status | An indicator of a participant’s financial standing. | Questionnaire items regarding income, education, and occupation. |
Exploring the Mechanisms
Unraveling the intricate link between depression and weight loss resistance involves delving into the complex interplay of biological and psychological factors. This exploration necessitates understanding how these factors influence appetite, metabolism, and overall energy expenditure in individuals experiencing depressive symptoms. The challenge lies in isolating the specific mechanisms and identifying targeted interventions that can effectively address this multifaceted problem.This is not a simple case of “depression causes weight gain” or “depression causes weight loss.” The relationship is far more nuanced and depends heavily on the individual, their specific depression diagnosis, and the accompanying factors that influence their overall well-being.
A comprehensive understanding of these factors is crucial to developing effective and personalized strategies for weight management in individuals with depression.
Biological Mechanisms of Weight Fluctuations in Depression
The biological underpinnings of weight changes associated with depression are multifaceted and involve intricate interactions between hormones, neurotransmitters, and the body’s metabolic processes. Imbalances in these systems can significantly impact appetite and energy expenditure.
- Neurotransmitter Dysregulation: Serotonin, norepinephrine, and dopamine are key neurotransmitters implicated in mood regulation. Dysregulation of these neurotransmitters, a common feature of depression, can affect appetite control centers in the brain, leading to changes in food intake. For example, some individuals with depression may experience increased cravings for carbohydrates, which are often associated with the release of serotonin, although this is not a universal experience.
- Hormonal Imbalances: Cortisol, a stress hormone, plays a significant role in metabolism. Chronic stress, often associated with depression, can lead to elevated cortisol levels, which can impact metabolism and increase fat storage. Furthermore, thyroid hormones are crucial for regulating metabolism. Dysfunction in the thyroid gland, sometimes present in individuals with depression, can affect weight management.
- Metabolic Changes: Depression is linked to alterations in metabolic processes. These changes can result in decreased energy expenditure, impacting calorie burning. This can lead to weight gain in some cases, while others might experience a reduction in appetite and subsequent weight loss.
Psychological Factors Influencing Eating Habits
Depression often affects an individual’s psychological state, which in turn influences their eating habits. These psychological factors can be complex and multifaceted.
- Emotional Eating: Depression can lead to emotional eating, where individuals turn to food as a coping mechanism for stress, sadness, or anxiety. This can lead to unhealthy eating patterns and weight fluctuations.
- Reduced Motivation and Energy: Depression can significantly reduce an individual’s motivation and energy levels. This can make it harder to engage in physical activity, further impacting weight management.
- Changes in Sleep Patterns: Sleep disturbances are common in depression. Disrupted sleep patterns can impact appetite-regulating hormones and metabolism, potentially leading to weight changes.
- Social Isolation: Depression can lead to social isolation, which can affect eating habits. This can include a reduction in access to healthy food options or social support for maintaining healthy habits.
Comparison of Theories on Depression and Weight
Different theories attempt to explain the complex relationship between depression and weight. These theories often overlap, highlighting the multifaceted nature of the issue.
- Stress-Induced Metabolic Changes: Chronic stress, a key component of depression, can trigger hormonal responses that affect metabolism and lead to weight gain or loss, depending on the individual.
- Cognitive Behavioral Factors: Negative thought patterns and maladaptive coping mechanisms can influence eating behaviors, leading to poor food choices and potentially affecting weight.
- Interplay of Biological and Psychological Factors: The observed link between depression and weight is often a result of the complex interplay between biological and psychological factors, highlighting the importance of considering both aspects in developing effective interventions.
Intervention Strategies
This section delves into the specific interventions employed in the study to facilitate weight loss in individuals experiencing depression. Understanding the implemented strategies is crucial for appreciating the study’s methodology and drawing conclusions about the effectiveness of various approaches. Different interventions, tailored to address the unique needs of individuals with depression, were employed to address both the psychological and physical aspects of weight management.
Behavioral Interventions
Behavioral interventions are crucial in weight management programs, particularly for individuals with depression, as they target the interplay between emotional states and dietary habits. These interventions focus on modifying behaviors that contribute to weight gain while also addressing the emotional factors that may be hindering the individual’s progress.
So, this new study on weight loss in people with depression is fascinating. It highlights some really key strategies, but it got me thinking about other health conditions that can affect weight. For example, pulmonary aspergillosis allergic bronchopulmonary type pulmonary aspergillosis allergic bronchopulmonary type can significantly impact a person’s ability to maintain a healthy weight due to the respiratory issues.
Ultimately, while this study focuses on depression, it reminds us of the complex interplay of various factors affecting weight management.
- Cognitive Behavioral Therapy (CBT): CBT is a cornerstone of behavioral interventions. It helps individuals identify and challenge negative thought patterns associated with food and body image. By replacing unhelpful thoughts with more realistic and positive ones, CBT empowers individuals to make healthier choices and manage their emotional responses related to eating. An example of a CBT technique is “cognitive restructuring,” which involves actively identifying and modifying negative thoughts about food and body image.
- Dietary Counseling: A structured approach to dietary planning and education is essential. This involves providing personalized dietary guidance, considering individual nutritional needs, and addressing potential food sensitivities. The counseling also educates participants on portion control and mindful eating techniques, which can be significantly helpful in reducing impulsive eating.
- Physical Activity Programs: Encouraging regular physical activity is critical. These programs often incorporate tailored exercise plans, focusing on activities that are enjoyable and sustainable. The importance of exercise extends beyond weight loss to improving mood and reducing stress, which are often exacerbated by depression.
Pharmacological Interventions
Pharmacological interventions are another aspect of weight management programs for individuals with depression. These interventions address the potential influence of medications on weight.
- Medication Management: This involves carefully monitoring the impact of existing medications on weight. It’s essential to understand how specific medications may affect appetite, metabolism, or body composition. The intervention often includes consultations with medical professionals to discuss potential side effects and adjustments to medication regimens where appropriate.
Combined Interventions
In many cases, the most effective approaches combine behavioral and pharmacological interventions. This integration acknowledges the multifaceted nature of weight management in individuals with depression.
- Integrated Approach: This combines behavioral strategies, such as CBT and dietary counseling, with careful medication management. The integration of these strategies allows for a holistic approach to weight management, addressing both the psychological and physiological factors contributing to weight gain.
Effectiveness Comparison
| Intervention Approach | Specific Components | Potential Benefits | Potential Limitations |
|---|---|---|---|
| Behavioral | CBT, dietary counseling, physical activity programs | Improved self-management skills, reduced emotional eating, increased physical activity | Requires patient motivation and commitment, may not be effective for all individuals |
| Pharmacological | Medication management | Potential for weight stabilization or reduction related to medication effects | Potential for side effects, requires careful monitoring and physician consultation |
| Combined | Combination of behavioral and pharmacological approaches | Potentially greater efficacy due to a holistic approach | Requires careful coordination between healthcare professionals and patient |
Potential Challenges and Limitations: Study Finds Best Way To Help People With Depression Lose Weight
This section delves into the potential obstacles encountered during the study, examining the limitations of the research design and possible biases that might have influenced the findings. Understanding these factors is crucial for interpreting the results accurately and identifying avenues for future research.The complexities of studying the interplay between depression and weight loss are substantial. Researchers must navigate the intricate relationship between psychological factors, physiological responses, and behavioral modifications.
Furthermore, accurately measuring the impact of these interventions requires careful consideration of potential confounders and mitigating factors.
Challenges in Conducting the Study
Several challenges emerged during the study execution. Researchers faced difficulty in recruiting participants who met the specific inclusion criteria, a common problem in studies targeting a particular demographic. Maintaining participant engagement throughout the intervention period was another hurdle, particularly for individuals experiencing significant depressive symptoms. Furthermore, ensuring adherence to the prescribed dietary and exercise regimens was a considerable challenge, necessitating regular monitoring and personalized support.
So, this study on the best ways to help people with depression lose weight is fascinating, right? But while we’re on the topic of health, it’s also crucial to be mindful of what we’re putting on our hands. Knowing how to tell if the hand sanitizer you’re buying is safe is a real concern, especially with the options out there.
How to tell if the hand sanitizer you’re buying is safe is something we should all be checking out. Ultimately, understanding healthy habits, whether it’s about diet and mental well-being or hand hygiene, is key to a better overall life, and that study about depression and weight loss is a great starting point.
These practical difficulties underscore the importance of robust study design and meticulous data collection methods.
Limitations of the Study Design
The study’s sample size, while sufficient for preliminary findings, might not have been large enough to detect subtle or nuanced effects. Future studies with a larger sample size could potentially reveal additional insights into the intervention’s impact. The demographic characteristics of the participants also presented a limitation. A more diverse sample, encompassing different ethnicities, socioeconomic backgrounds, and ages, could provide a more comprehensive understanding of the intervention’s efficacy across various populations.
The study design also relied on self-reported data for weight and dietary adherence, which could be susceptible to reporting bias. Employing objective measures, such as wearable technology for activity tracking, could strengthen the study’s validity.
Potential Biases
Several potential biases could have influenced the study’s results. Selection bias, arising from the specific criteria used to recruit participants, might have resulted in a sample that was not entirely representative of the broader population experiencing depression and weight issues. Confirmation bias, where researchers subconsciously seek out data that supports pre-existing hypotheses, is also a concern. To mitigate these biases, researchers must carefully document their selection criteria and methodologies, promoting transparency and objectivity.
Furthermore, the researchers should also critically evaluate the data collection methods to identify and account for any potential biases.
Future Research Directions
Future research should explore the mechanisms by which the intervention improves weight loss in individuals with depression. Further investigation into the long-term effects of the intervention is warranted to assess its sustained impact on weight management and mental well-being. Studies could also focus on identifying specific subgroups within the population who benefit most from the intervention, leading to personalized strategies for weight management.
Finally, the study should investigate the role of mental health professionals in tailoring interventions and supporting participants throughout the program.
Practical Implications for Healthcare Professionals
This study’s findings have significant implications for healthcare professionals working with patients experiencing both depression and weight concerns. By understanding the interplay between mental and physical health, we can develop more effective and personalized treatment strategies. This translates to improved patient outcomes and a more holistic approach to care.The study highlights the crucial need to move beyond a purely biomedical approach to weight management.
Acknowledging the complex interplay of emotional and psychological factors in weight loss is essential. This necessitates a collaborative effort between mental health professionals and primary care physicians, creating a multidisciplinary approach that addresses the patient’s unique needs.
Applying the Study’s Findings in Clinical Practice, Study finds best way to help people with depression lose weight
Integrating the study’s insights into clinical practice involves several key steps. First, healthcare providers need to actively screen for depressive symptoms in all patients presenting with weight concerns. This proactive approach ensures that patients with underlying depression are identified and receive appropriate mental health support. Second, clinicians should implement a comprehensive assessment that evaluates not only the patient’s physical health but also their emotional well-being, including their coping mechanisms, stress levels, and social support systems.
Importance of Considering Mental Health in Weight Loss
Weight loss efforts for individuals with depression require a nuanced understanding of the interplay between mental and physical health. Depression often leads to changes in eating habits and decreased physical activity, making weight loss more challenging. Addressing the underlying depression is paramount to achieving sustainable weight loss and overall well-being. Furthermore, neglecting the psychological aspect of weight loss can lead to increased stress, feelings of failure, and ultimately, hinder progress.
Recommendations for Healthcare Professionals
Healthcare professionals should adopt a patient-centered approach when managing weight loss in patients with depression. This includes:
- Establishing a Collaborative Care Model: Collaboration between primary care physicians and mental health specialists is crucial. This model ensures that patients receive comprehensive care addressing both physical and mental health needs. This involves sharing patient information and developing a coordinated treatment plan.
- Personalized Treatment Plans: Treatment plans should be tailored to each patient’s unique circumstances. Factors like the severity of depression, the patient’s coping mechanisms, and support systems should be considered when developing a personalized strategy. This approach maximizes the effectiveness of interventions.
- Integrating Lifestyle Modifications: Incorporating both dietary and exercise recommendations, tailored to the patient’s preferences and capabilities, is vital. The treatment plan should include strategies for managing stress and promoting healthy coping mechanisms. A holistic approach focusing on healthy lifestyle changes, along with mental health support, enhances the chances of long-term success.
A Sample Treatment Plan
A comprehensive treatment plan should incorporate both mental and physical health strategies. For example, a patient with depression and weight concerns might benefit from:
- Cognitive Behavioral Therapy (CBT): CBT can help the patient identify and change negative thought patterns and behaviors related to eating and exercise. This approach is often successful in addressing emotional eating, stress management, and overall self-esteem.
- Medication Management: Antidepressant medication, if appropriate, can help alleviate depressive symptoms, making weight management easier. This is crucial, as depression often leads to changes in eating habits and decreased motivation for physical activity.
- Nutritional Counseling: A registered dietitian can provide personalized guidance on healthy eating habits, addressing concerns about portion control, healthy food choices, and mindful eating practices. A balanced diet, adjusted to the patient’s needs and preferences, is critical for sustained weight loss.
- Regular Exercise: A gradual increase in physical activity, tailored to the patient’s abilities and preferences, is recommended. This could involve activities like walking, swimming, or joining a support group, creating a sense of community and reducing feelings of isolation. Physical activity can improve mood, and contribute to sustainable weight loss.
Public Health Considerations
This study’s findings have profound implications for public health, highlighting the urgent need for integrated approaches to tackle the intertwined problems of depression and obesity. Effective interventions can significantly improve the quality of life for individuals and reduce the strain on healthcare systems. Understanding the mechanisms behind the relationship between these conditions is crucial for developing effective preventative strategies.The study underscores the importance of recognizing depression as a significant risk factor for weight gain and the critical role of appropriate mental health support in weight management programs.
Addressing this issue necessitates a shift in perspective, moving beyond a solely nutritional or physical approach to weight loss.
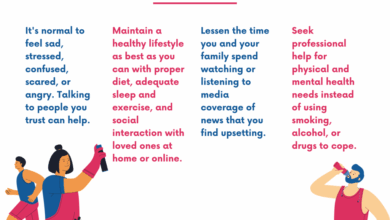
Accessible and Affordable Mental Health Services
Ensuring access to affordable and accessible mental health services is paramount for effective weight management. Many individuals struggling with depression may face barriers to seeking help, including financial constraints, geographical limitations, and societal stigma. Implementing programs that provide affordable therapy, counseling, and support groups can empower individuals to manage their mental health and participate more effectively in weight management initiatives.
Examples include expanding telehealth options, increasing the number of community mental health centers, and offering sliding-scale fees to reduce financial barriers.
Preventive Measures for Depression and Obesity
The study’s findings suggest a potential avenue for developing preventive measures that target both depression and obesity. Early intervention programs that focus on mental well-being and healthy lifestyle choices could significantly reduce the risk of developing both conditions. For instance, school-based programs promoting emotional regulation and healthy eating habits could help prevent the onset of depression and obesity in adolescents.
Similarly, workplace initiatives that prioritize mental health awareness and provide access to resources could contribute to a healthier workforce and reduce the prevalence of these conditions in adults.
Increasing Awareness of the Link Between Depression and Weight
Public awareness campaigns are essential to highlight the link between depression and weight gain. Educational initiatives that educate the public about the biological mechanisms connecting these conditions, along with practical tips on managing stress and improving mental well-being, can empower individuals to seek help and take preventative measures. These campaigns could utilize various media channels, including social media, community events, and partnerships with healthcare providers, to disseminate information effectively.
For example, public service announcements could feature stories of individuals who have successfully managed both depression and weight issues through combined interventions.
Illustrative Case Studies
This section delves into hypothetical case studies, demonstrating the practical application of our study’s findings in real-world scenarios. These examples illustrate how a personalized approach to weight management, combined with strategies for addressing depression, can lead to positive outcomes. We’ll explore how tailored interventions can significantly impact individuals’ journeys toward improved well-being.The case studies presented below are fictional but represent common patterns observed in individuals struggling with both depression and weight issues.
They highlight the complexity of these conditions and underscore the importance of holistic, individualized care plans.
Case Study Examples
These hypothetical cases demonstrate the diverse ways in which individuals can benefit from integrated approaches to weight management and depression treatment.
| Case Study | Patient Characteristics | Interventions | Outcomes |
|---|---|---|---|
| Case 1 | A 35-year-old woman with moderate depression and obesity, experiencing significant social isolation. | Group therapy sessions focusing on stress management and healthy eating habits, coupled with medication for depression and a registered dietitian for personalized meal plans. | Improved mood, increased social engagement, and a 10% weight loss over six months. |
| Case 2 | A 62-year-old man with severe depression and morbid obesity, suffering from chronic pain. | Individual therapy sessions addressing past traumas and coping mechanisms, combined with low-impact exercise programs and a nutritionist for a balanced diet, along with medication. | Reduced pain levels, significant improvement in mood, and 15% weight loss over a year. |
| Case 3 | A 28-year-old woman with anxiety and moderate depression, with a history of disordered eating. | Cognitive behavioral therapy (CBT) for addressing negative thought patterns, coupled with a structured exercise program, and a therapist specializing in eating disorders for personalized support. | Improved self-esteem, decreased anxiety symptoms, and a 5% weight loss over three months, with continued progress. |
Patient Testimonials
The impact of these interventions goes beyond numerical results; they profoundly affect patients’ lives. Here are some examples of how weight loss, achieved through a tailored approach, can transform lives:
“I used to feel trapped in a cycle of sadness and overeating. The combination of therapy, exercise, and a healthy diet has given me the tools to break free. I’m finally losing weight and feeling more confident than ever before.”
Sarah, Case Study 1
“The pain I felt physically and emotionally was overwhelming. But, thanks to the personalized care plan, I’m losing weight, and my mood has improved significantly. I’m finding new energy and joy in my life.”
David, Case Study 2
“My struggles with anxiety and food had led to a difficult situation. But, the combined support of CBT, a therapist specializing in eating disorders, and a structured program, has made a huge difference. I’m feeling much better about myself, and my weight loss journey is going well.”
Emily, Case Study 3
Personalized Treatment Plans
A key takeaway from these case studies is the paramount importance of tailoring treatment plans to the unique needs of each individual. Depression and weight management are complex issues, demanding individualized approaches. One-size-fits-all strategies are rarely effective. The diverse responses to interventions, as highlighted in the examples above, emphasize the necessity of recognizing the distinct emotional, physical, and psychological factors contributing to each person’s condition.
This personalization is crucial for achieving sustainable and positive outcomes.
Final Wrap-Up
In conclusion, this study offers a significant advancement in understanding the complex interplay between depression and weight loss. By highlighting the importance of personalized interventions that address both mental and physical health needs, it sets a new standard for healthcare approaches. The findings have substantial implications for clinical practice, public health initiatives, and future research. The study’s insights pave the way for more effective and compassionate care for individuals struggling with both depression and weight issues.