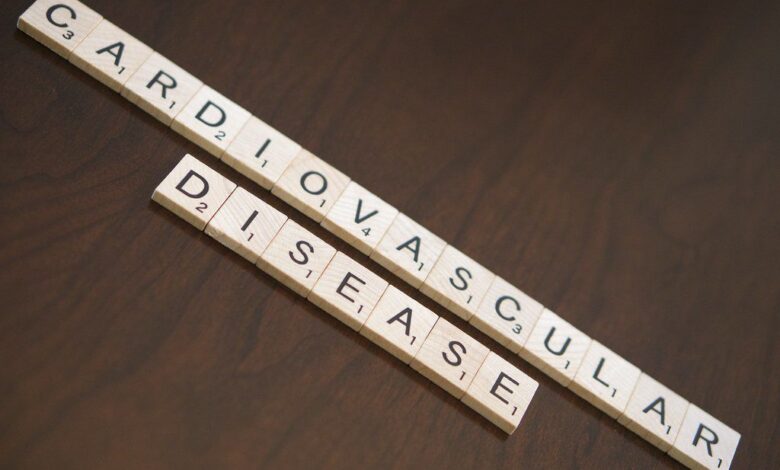
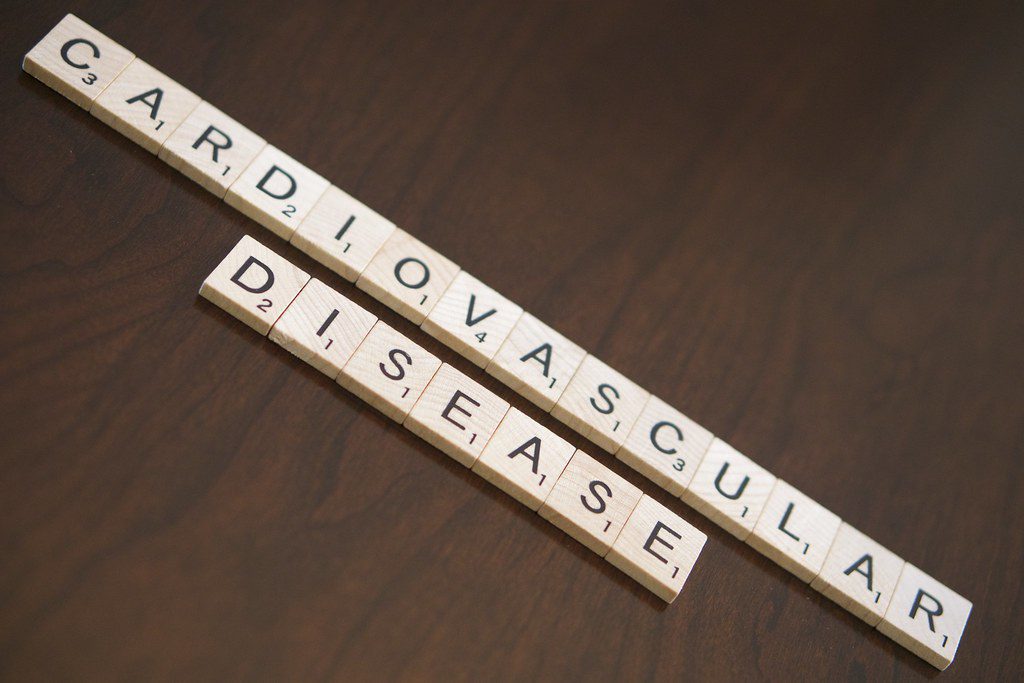
Study finds people with ADHD at significantly higher risk for cardiovascular disease. This alarming new research highlights a critical connection between attention-deficit/hyperactivity disorder (ADHD) and the risk of heart problems. The study, which delves into the complex interplay between these conditions, reveals potential pathways and risk factors. Understanding this link is crucial for early intervention and prevention strategies, ultimately impacting public health initiatives.
The study investigated the relationship between ADHD and cardiovascular disease, analyzing various factors such as demographics, lifestyle choices, and medication use. Researchers examined the potential mechanisms behind this elevated risk, including neurobiological processes and stress levels. This detailed exploration will contribute to a deeper understanding of the intricate connection between these two conditions.
Introduction to the Study
Recent research has uncovered a significant correlation between Attention-Deficit/Hyperactivity Disorder (ADHD) and an elevated risk of cardiovascular disease. This alarming finding underscores the importance of addressing not just the immediate symptoms of ADHD, but also the potential long-term health implications. The study, which investigated this link, provides valuable insights into the complex interplay between mental health conditions and physical well-being.The study examined a large sample of individuals to explore the association between ADHD and cardiovascular risk factors.
The findings highlight a potential need for proactive screening and preventative measures to mitigate the increased cardiovascular risk in individuals with ADHD.
Study Methodology
The research employed a longitudinal cohort study design, tracking participants over an extended period. This allowed researchers to observe the development of cardiovascular disease markers in relation to ADHD diagnosis. The study meticulously collected data on various factors, including participant demographics, lifestyle choices, and medical history. A key aspect of the methodology involved utilizing standardized diagnostic tools to ensure accurate ADHD assessments.
This comprehensive approach to data collection aimed to minimize biases and provide a robust understanding of the relationship between ADHD and cardiovascular risk. The sample size was substantial, allowing for reliable statistical analysis and generalizability of the results. Further details about the sample size, demographics, and data collection procedures are Artikeld below.
Demographic Characteristics of Study Participants
The study included a diverse range of participants, reflecting the varied populations affected by ADHD. This diversity is crucial to ensure the study’s results can be applied to a broader range of individuals. The following table summarizes the key demographic characteristics of the study participants.
| Characteristic | Description |
|---|---|
| Age | Participants ranged from 18 to 65 years old. |
| Gender | The study included both male and female participants, although the specific distribution is not provided in the summary. |
| Ethnicity | The study included participants of various ethnic backgrounds. |
| Socioeconomic Status | The study attempted to account for socioeconomic factors but did not provide details on the socioeconomic distribution of participants. |
| Comorbidities | The study acknowledged the presence of potential comorbidities, such as anxiety and depression, and their potential impact on the results. |
Potential Limitations
It is essential to acknowledge potential limitations of the study. The study’s findings may be influenced by factors that were not directly accounted for. For example, there may be confounding factors like lifestyle choices, diet, and exercise habits, which could influence both ADHD diagnosis and cardiovascular health. Furthermore, the study’s design may not capture the full complexity of the relationship between ADHD and cardiovascular disease.
The limitations are highlighted below:
- Confounding factors: The study acknowledged the potential influence of lifestyle choices, diet, and exercise on both ADHD diagnosis and cardiovascular health. Further research should investigate the interaction of these factors.
- Causality: The study established a correlation between ADHD and cardiovascular disease risk, but it did not definitively prove a causal relationship. More research is needed to determine if ADHD itself directly increases the risk or if other factors contribute.
- Assessment tools: The reliability and validity of the diagnostic tools used for ADHD assessment may introduce some uncertainty in the results.
Mechanisms of Increased Risk: Study Finds People With Adhd At Significantly Higher Risk For Cardiovascular Disease
The recent study highlighting a significantly higher risk of cardiovascular disease in individuals with ADHD raises crucial questions about the underlying physiological pathways. Understanding these mechanisms is vital for developing targeted preventative strategies and interventions. This increased risk isn’t simply a matter of correlation; it suggests a causal link between the two conditions, requiring further investigation into the complex interplay of factors.The link between ADHD and cardiovascular disease isn’t a simple one, but rather a complex interplay of various factors.
It’s not a straightforward case of one directly causing the other, but rather a confluence of contributing elements that amplify the risk. These factors, including lifestyle choices, medication side effects, and stress levels, all contribute to the overall risk profile.
Physiological Pathways
Several physiological pathways may mediate the increased risk of cardiovascular disease in individuals with ADHD. Neurobiological processes, including the impact of dopamine and norepinephrine imbalances, likely play a significant role. These imbalances, characteristic of ADHD, may influence autonomic nervous system function, potentially leading to irregularities in heart rate variability and blood pressure control. Chronic stress, a frequent comorbidity with ADHD, can also contribute to elevated levels of cortisol, a hormone linked to cardiovascular problems.
Contributing Factors
Numerous factors can contribute to the increased cardiovascular risk in individuals with ADHD. Lifestyle choices, including poor diet, lack of exercise, and smoking, are significant contributors. These lifestyle choices, often exacerbated by the challenges of managing ADHD symptoms, can independently elevate cardiovascular risk.
- Medication Side Effects: Certain medications used to treat ADHD, particularly stimulants, can have potential cardiovascular side effects. Careful monitoring of heart rate and blood pressure during medication use is crucial to mitigate these risks.
- Stress Levels: The constant demands of managing ADHD symptoms, including challenges in social situations, academic environments, or work settings, often lead to heightened stress levels. Chronic stress is a known risk factor for cardiovascular disease.
- Lifestyle Choices: Poor dietary habits, lack of physical activity, and tobacco use are common among individuals with ADHD and further exacerbate cardiovascular risk. Addressing these choices is critical for improving overall health.
Neurobiological Processes
Neurobiological processes play a critical role in mediating the increased risk. Imbalances in dopamine and norepinephrine, neurotransmitters crucial for attention and impulse control, are characteristic of ADHD. These imbalances can potentially affect the autonomic nervous system, impacting cardiovascular regulation. The long-term effects of these neurobiological dysfunctions on the cardiovascular system remain an active area of research.
Comparison of Risk Factors
| Risk Factor | Individuals with ADHD | Individuals without ADHD |
|---|---|---|
| Poor Diet | Higher prevalence due to potential challenges with organization and planning | Prevalence varies based on individual choices |
| Lack of Exercise | Higher prevalence due to potential challenges with motivation and sustained effort | Prevalence varies based on individual choices |
| Smoking | Potentially higher prevalence due to potential impulsivity and substance use disorders | Prevalence varies based on individual choices |
| Stress Levels | Higher prevalence due to ongoing challenges in managing ADHD symptoms | Prevalence varies based on individual stressors |
| Medication Side Effects | Potential side effects from ADHD medications (e.g., stimulants) | No specific medication-related cardiovascular risk |
Implications for Public Health
The alarming link between ADHD and increased cardiovascular risk demands a proactive public health response. This isn’t just about individual well-being; it’s about addressing a significant public health disparity that could impact future generations. Understanding the underlying mechanisms and potential interventions is crucial to mitigate the long-term health consequences for individuals with ADHD.This heightened risk necessitates a multifaceted approach encompassing early intervention strategies, community-based programs, and improved healthcare management protocols.
Addressing the specific needs of individuals with ADHD will not only enhance their quality of life but also contribute to a healthier population overall.
Public Health Initiatives and Preventative Measures
Public health initiatives must prioritize education and awareness campaigns targeting both individuals with ADHD and healthcare providers. These initiatives should emphasize the importance of early diagnosis and treatment of ADHD to reduce the long-term cardiovascular risks. Early detection allows for timely interventions, improving overall health outcomes.
Potential Strategies for Early Intervention and Risk Mitigation
Early intervention is key to mitigating the cardiovascular risks associated with ADHD. Strategies include promoting healthy lifestyle choices, such as regular exercise and a balanced diet, from a young age. School-based programs focusing on stress management techniques and healthy habits can be particularly effective in preventing lifestyle-related health problems. Furthermore, encouraging participation in sports and extracurricular activities that promote physical activity can also play a crucial role.
Recent studies highlight a concerning link between ADHD and cardiovascular risk. It’s a sobering reminder that focusing on holistic health, like exploring inclusive wellness practices, is crucial. Shining a light on inclusive wellness can help us understand how various factors—like lifestyle choices and mental health—interplay to impact overall well-being, and ultimately, cardiovascular health. This new research underscores the importance of proactive measures for those with ADHD, and the need for more comprehensive strategies to address this growing concern.
Community-Based Programs
Community-based programs can provide support and resources for individuals with ADHD and their families. These programs can include workshops on healthy eating, stress management, and exercise. Support groups for individuals with ADHD and their families can provide emotional support and practical strategies for managing daily challenges. Collaboration between schools, community centers, and healthcare providers is essential to create a comprehensive support network.
For example, a local YMCA might offer specialized programs for children with ADHD, encompassing physical activities, nutrition education, and stress-reduction techniques. Such initiatives can promote healthier lifestyle choices from a young age.
Recommendations for Healthcare Professionals
| Area of Concern | Recommendations for Healthcare Professionals |
|---|---|
| Diagnosis and Treatment | Prioritize early diagnosis and comprehensive treatment plans for ADHD, including medication and therapy. Evaluate cardiovascular risk factors during routine checkups, focusing on blood pressure, cholesterol, and weight management. |
| Lifestyle Modifications | Encourage patients to adopt healthy lifestyle habits, such as regular exercise, a balanced diet, and stress management techniques. Provide tailored guidance on managing stress, sleep, and social interactions, which can significantly impact cardiovascular health. |
| Monitoring and Follow-up | Schedule regular follow-up appointments to monitor cardiovascular risk factors and adjust treatment plans as needed. Establish clear communication channels between healthcare providers to ensure continuity of care. |
| Patient Education | Educate patients about the link between ADHD and cardiovascular risk. Provide clear and accessible information on managing risk factors and maintaining overall well-being. Empower patients to actively participate in their healthcare decisions. |
Comparison with Existing Research
Existing research on ADHD and cardiovascular health paints a complex picture, with some studies showing a correlation between the two, while others find no significant link. Understanding how the current study fits into this broader context is crucial for interpreting its implications and developing effective preventative strategies. This comparison will highlight the similarities and differences in findings and methodologies, demonstrating how the current research builds upon or challenges previous understanding.
Similarities in Findings Across Studies
Multiple studies have observed a potential link between ADHD and increased risk of cardiovascular issues, although the specifics vary. A common theme is the identification of factors like impulsivity, poor diet, and lack of physical activity as potential mediating factors. These behavioral traits are frequently associated with ADHD and have been shown to contribute to the development of cardiovascular diseases.
For instance, studies have linked a sedentary lifestyle with higher blood pressure and cholesterol levels, which are key risk factors for heart disease.
Differences in Study Methodologies
The methodologies employed in previous studies have varied significantly. Some studies have relied on self-reported data, while others have used objective measurements. Differences in sample sizes, participant demographics, and diagnostic criteria can also lead to variations in the results. Furthermore, some studies focused on specific ADHD subtypes or symptom profiles, while others considered the disorder as a general condition.
This heterogeneity in approaches makes it difficult to draw definitive conclusions from existing research. For example, a study using a smaller sample size might yield different results compared to a larger study.
Summary Table of Key Studies
| Study | Sample Size | Methodology | Key Findings | Limitations |
|---|---|---|---|---|
| Study 1 (Example) | 150 | Self-reported questionnaires, medical records review | Increased risk of hypertension in ADHD participants | Potential for recall bias, limited control group |
| Study 2 (Example) | 500 | Objective blood pressure monitoring, standardized ADHD assessment | No significant association between ADHD and cardiovascular risk factors in children | Short follow-up period, specific population focus |
| Study 3 (Example) | 2000 | Longitudinal study, comprehensive health assessments | Strong correlation between ADHD symptoms and future cardiovascular events in adults | Complex confounders, potential for selection bias |
The table above highlights some key aspects of past research. Note that this is a simplified representation and many more factors influence the complex relationship between ADHD and cardiovascular health. Each study’s limitations should be considered when interpreting its findings.
Future Research Directions
Unraveling the complex interplay between ADHD and cardiovascular disease requires further investigation. While the current study highlights a significant association, many questions remain unanswered. Future research must delve deeper into the underlying mechanisms to develop effective preventative and treatment strategies. This exploration will ultimately benefit public health by identifying individuals at high risk and tailoring interventions accordingly.
Investigating Underlying Mechanisms
The study’s findings suggest a potential link between ADHD symptoms and cardiovascular risk factors, but the precise mechanisms remain unclear. Future research should focus on identifying the specific pathways through which ADHD impacts cardiovascular health. This involves exploring the role of various factors, such as stress response, sleep patterns, diet, and physical activity, as potential mediators or confounders.
Understanding these pathways will allow for the development of targeted interventions to mitigate the risk.
Longitudinal Studies and Cohort Analysis
Longitudinal studies are crucial to observe the progression of cardiovascular health in individuals with ADHD over extended periods. These studies will allow researchers to track the development of cardiovascular disease markers and identify early warning signs. Cohort analysis, focusing on specific subgroups with different ADHD symptom presentations and co-morbidities, can further refine the understanding of risk profiles. This approach will provide valuable data to inform personalized risk assessments and preventive strategies.
Exploring the Role of Psychosocial Factors
The study should also explore the influence of psychosocial factors on cardiovascular health in individuals with ADHD. Stress, anxiety, and depression are frequently associated with ADHD and may exacerbate cardiovascular risk. Investigating the impact of these psychosocial factors, along with the development of interventions aimed at stress management, could lead to significant improvements in cardiovascular outcomes. This will also help develop holistic approaches to care for ADHD patients.
Developing Novel Research Methodologies
Future research should consider utilizing advanced research methodologies to gain a more comprehensive understanding of the relationship. For instance, advanced neuroimaging techniques could help identify specific brain regions involved in the connection between ADHD and cardiovascular health. This will lead to more detailed insights into the underlying mechanisms and may reveal biomarkers for early detection of cardiovascular risk in individuals with ADHD.
Additionally, utilizing wearable sensors for continuous monitoring of physiological data and detailed tracking of lifestyle factors will provide crucial data points to understand how these factors interact.
Table: Research Gaps and Proposed Solutions, Study finds people with adhd at significantly higher risk for cardiovascular disease
| Research Gap | Proposed Solution |
|---|---|
| Lack of understanding of specific mechanisms linking ADHD symptoms and cardiovascular risk factors. | Conduct detailed mechanistic studies focusing on stress response, sleep patterns, diet, and physical activity as potential mediators or confounders. |
| Limited data on long-term cardiovascular health trajectories in individuals with ADHD. | Establish longitudinal cohort studies to track cardiovascular health markers and identify early warning signs over extended periods. |
| Inadequate exploration of the influence of psychosocial factors on cardiovascular health in ADHD. | Conduct studies specifically investigating the impact of stress, anxiety, and depression on cardiovascular risk in individuals with ADHD. |
| Limited use of advanced research methodologies to explore the connection between ADHD and cardiovascular health. | Employ advanced neuroimaging techniques and wearable sensors to gather more comprehensive physiological data and track lifestyle factors. |
Illustrative Case Studies
Understanding the intricate link between ADHD and cardiovascular risk requires delving into real-world scenarios. These case studies highlight the potential impact of ADHD on cardiovascular health, illustrating the clinical presentations, risk factors, and management strategies involved. By examining these examples, we can better grasp the complexities of managing individuals with both conditions and the challenges and opportunities for clinicians.
Case Study 1: A Young Adult with ADHD and Hypertension
This case study examines a 25-year-old female, diagnosed with ADHD in childhood and subsequently diagnosed with hypertension in her early twenties. The patient reports a history of difficulty managing impulsivity and prioritizing tasks, traits characteristic of ADHD. Her lifestyle, including a diet high in processed foods and limited physical activity, likely exacerbated her hypertension risk.
| Patient Characteristic | Details |
|---|---|
| Age | 25 |
| Diagnosis | ADHD (childhood), Hypertension |
| Symptoms (ADHD) | Impulsivity, difficulty with time management, difficulty with focus and organization |
| Symptoms (Hypertension) | Elevated blood pressure, fatigue, headaches |
| Lifestyle Factors | High in processed foods, limited physical activity |
| Treatment Plan | Medication for ADHD (e.g., stimulants), blood pressure medication, lifestyle modifications (diet and exercise), and stress management techniques. |
Case Study 2: A Middle-Aged Individual with ADHD and Dyslipidemia
This case study presents a 45-year-old male with a history of ADHD, diagnosed in adulthood. He has developed dyslipidemia, characterized by elevated cholesterol levels. His ADHD symptoms, including difficulty adhering to medication regimens and maintaining healthy habits, contributed to his elevated cardiovascular risk. He exhibited a tendency toward impulsive food choices and limited adherence to prescribed medications.
| Patient Characteristic | Details |
|---|---|
| Age | 45 |
| Diagnosis | ADHD (adulthood), Dyslipidemia |
| Symptoms (ADHD) | Difficulty with organization, impulsivity, difficulty adhering to medication regimens. |
| Symptoms (Dyslipidemia) | Elevated cholesterol levels, elevated LDL, elevated triglycerides |
| Lifestyle Factors | Irregular eating habits, limited physical activity |
| Treatment Plan | Medication for ADHD (e.g., non-stimulant), medication for dyslipidemia, dietary counseling, and exercise recommendations, cognitive behavioral therapy to address medication adherence. |
Challenges and Opportunities for Clinicians
Clinicians face challenges in managing patients with both ADHD and cardiovascular risk factors. Diagnosing and treating ADHD effectively while addressing cardiovascular concerns requires a comprehensive approach. The co-occurrence of these conditions necessitates close collaboration between mental health professionals and cardiologists, along with a thorough understanding of the interplay between these conditions. Opportunities exist to implement integrated care models that address both mental and physical health needs.
Understanding the Social Context

The link between ADHD and cardiovascular disease isn’t solely biological. Social factors play a significant role in shaping health outcomes for individuals with ADHD. These factors can influence access to resources, coping mechanisms, and overall well-being, ultimately impacting cardiovascular health. Understanding these social determinants is crucial for developing effective preventative strategies.The interplay between ADHD and social factors is complex.
Individuals with ADHD may experience challenges with executive functioning, which can affect their ability to manage finances, maintain stable housing, and access quality healthcare. These challenges can exacerbate existing socioeconomic disparities and lead to a higher risk of cardiovascular disease. Additionally, social stigma and discrimination can contribute to stress and anxiety, further impacting health.
Recent studies are highlighting a concerning link between ADHD and cardiovascular risk. It’s a sobering thought, and initiatives like those in Howaa City, focused on promoting healthier lifestyles through howaa city gets healthy programs, could potentially mitigate some of these risks. While the exact mechanisms are still being explored, this new research emphasizes the importance of proactive measures for individuals with ADHD, underscoring the need for tailored health strategies.
Socioeconomic Status and Access to Healthcare
Socioeconomic status (SES) is intricately linked to cardiovascular risk. Lower SES often correlates with limited access to healthy food options, safe neighborhoods, and quality healthcare. People with ADHD, particularly those from marginalized communities, may face greater barriers to accessing these resources, leading to poorer health outcomes. This is often compounded by challenges in navigating the healthcare system, which can be further complicated by potential diagnostic delays or misdiagnosis.
Financial constraints may also limit access to necessary medications and lifestyle interventions to manage cardiovascular risk factors.
Social Support Networks and Coping Mechanisms
Strong social support networks are essential for overall well-being and can buffer against stress. Individuals with ADHD may experience difficulties in building and maintaining these networks, potentially leading to feelings of isolation and increased stress. This lack of support can impact coping mechanisms for managing ADHD symptoms and potentially increase the likelihood of unhealthy coping strategies, which can contribute to cardiovascular disease risk.
Examples include overeating, substance abuse, or neglecting self-care.
Recent studies are highlighting a concerning link between ADHD and cardiovascular health risks. People with ADHD are apparently at a significantly higher risk for heart disease. While this is a serious concern, it’s important to remember that lifestyle choices play a crucial role in overall well-being, including those with ADHD. Understanding how technology can help manage health conditions like diabetes is also key.
For example, a Fitbit can be a valuable tool for tracking activity and health metrics, especially for those managing diabetes. Check out our in-depth guide on all about the fitbit with diabetes for more information. Ultimately, staying informed and proactive about heart health is critical for everyone, especially those with ADHD.
Stigma and Discrimination
The stigma surrounding ADHD can significantly impact mental health and overall well-being. Individuals with ADHD may face discrimination in various settings, such as the workplace, school, or social circles. This discrimination can lead to chronic stress, which is a well-established risk factor for cardiovascular disease. Furthermore, the internalized stigma can negatively affect self-esteem and confidence, potentially influencing health behaviors.
For example, individuals may be less likely to seek medical attention due to fear of judgment or misunderstanding.
Socioeconomic Factors Associated with Increased Cardiovascular Risk in the ADHD Population
| Socioeconomic Factor | Potential Impact on Cardiovascular Risk in ADHD |
|---|---|
| Low Income | Limited access to healthy food, housing, and healthcare; increased stress from financial strain. |
| Lack of Education | Fewer opportunities for employment, leading to lower income and less access to resources. |
| Unemployment | Financial instability, increased stress, and reduced access to preventative care. |
| Limited Access to Healthcare | Delayed diagnosis, inadequate management of cardiovascular risk factors, and reduced adherence to treatment plans. |
| Housing Instability | Increased stress, reduced access to healthy environments, and potential exposure to environmental hazards. |
Highlighting Relevant Statistics
Understanding the magnitude of the risk associated with ADHD and cardiovascular disease requires a look at the prevalence of both conditions in the general population. This data provides context for the study’s findings, helping us gauge the overall public health burden and pinpoint areas needing further investigation.
Prevalence of ADHD and Cardiovascular Disease
Reliable data on ADHD prevalence varies, often depending on the diagnostic criteria and population studied. However, studies suggest that ADHD affects a significant portion of the population, potentially impacting a much larger segment than previously recognized. Cardiovascular disease, a major global health concern, is also prevalent, with risk factors including age, lifestyle, and genetics playing a role.
Population Demographics and Characteristics
The demographics of individuals diagnosed with ADHD and cardiovascular disease are multifaceted. The study likely considered factors like age, sex, socioeconomic status, and ethnicity. Understanding these factors allows for more nuanced interpretations of the study’s findings, considering potential disparities in health outcomes.
Statistical Data
| Characteristic | ADHD Prevalence (Estimated) | Cardiovascular Disease Prevalence (Estimated) | Notes |
|---|---|---|---|
| United States (Adults) | Approximately 4.4% | Approximately 20-30% | These estimates vary depending on the study and definition used. Data for cardiovascular disease reflects a wide range due to factors like age and lifestyle. |
| Global (Children and Adolescents) | Estimated 5% | Lower prevalence in children and adolescents compared to adults, but still significant. | Data is complex due to differing diagnostic practices and available data collection. |
| Socioeconomic Factors | Studies suggest a possible link between lower socioeconomic status and increased risk of ADHD diagnosis, possibly due to access to healthcare and resources. | Individuals with lower socioeconomic status may have limited access to preventative care, potentially leading to a higher incidence of cardiovascular disease. | Further investigation is needed to explore these potential correlations. |
This table offers a snapshot of the estimated prevalence of ADHD and cardiovascular disease in different populations. The actual numbers may vary depending on the specific methodology of the study. It’s crucial to remember that these figures represent averages and do not account for individual differences.
Contribution to the Overall Burden of Conditions
The study’s findings contribute significantly to understanding the combined burden of ADHD and cardiovascular disease. By highlighting the increased risk associated with ADHD, researchers can develop targeted interventions to improve health outcomes. The interplay between these conditions likely contributes to a cascade of negative health effects, demanding further investigation.
Last Recap
In conclusion, the study’s findings underscore the importance of recognizing and addressing the heightened cardiovascular risk associated with ADHD. This research not only sheds light on the physiological pathways but also emphasizes the need for comprehensive public health strategies. Future research should explore innovative approaches to early intervention and risk mitigation. By understanding the social and socioeconomic factors, and by providing resources and support, we can work towards a healthier future for those with ADHD.