This man with parkinsons experienced improvement after trying deep brain stimulation – This man with Parkinson’s experienced improvement after trying deep brain stimulation, a revolutionary treatment offering a glimmer of hope for those battling this debilitating disease. The procedure, involving the precise targeting of specific brain regions, aims to alleviate the debilitating symptoms of Parkinson’s. Understanding the science behind DBS, the individual case study, and the potential long-term implications is crucial for grasping the full impact of this transformative therapy.
Parkinson’s disease, characterized by tremors, rigidity, and slow movement, significantly impacts a patient’s quality of life. Deep brain stimulation (DBS) emerges as a potential solution, offering a surgical approach to alleviate these symptoms. This intervention involves implanting electrodes in specific areas of the brain, delivering electrical impulses that can modulate abnormal brain activity. The process, while complex, offers a pathway towards improved motor function, potentially leading to a more fulfilling life for those affected.
Introduction to Deep Brain Stimulation (DBS) for Parkinson’s Disease
Parkinson’s disease is a progressive neurological disorder affecting movement. Characterized by tremors, rigidity, slowness of movement (bradykinesia), and postural instability, it significantly impacts a person’s quality of life. The disease stems from the loss of dopamine-producing neurons in the brain, leading to an imbalance in neurotransmitters that control movement. Symptoms often start subtly and worsen over time, requiring ongoing management.Deep brain stimulation (DBS) is a surgical procedure that involves implanting electrodes in specific areas of the brain.
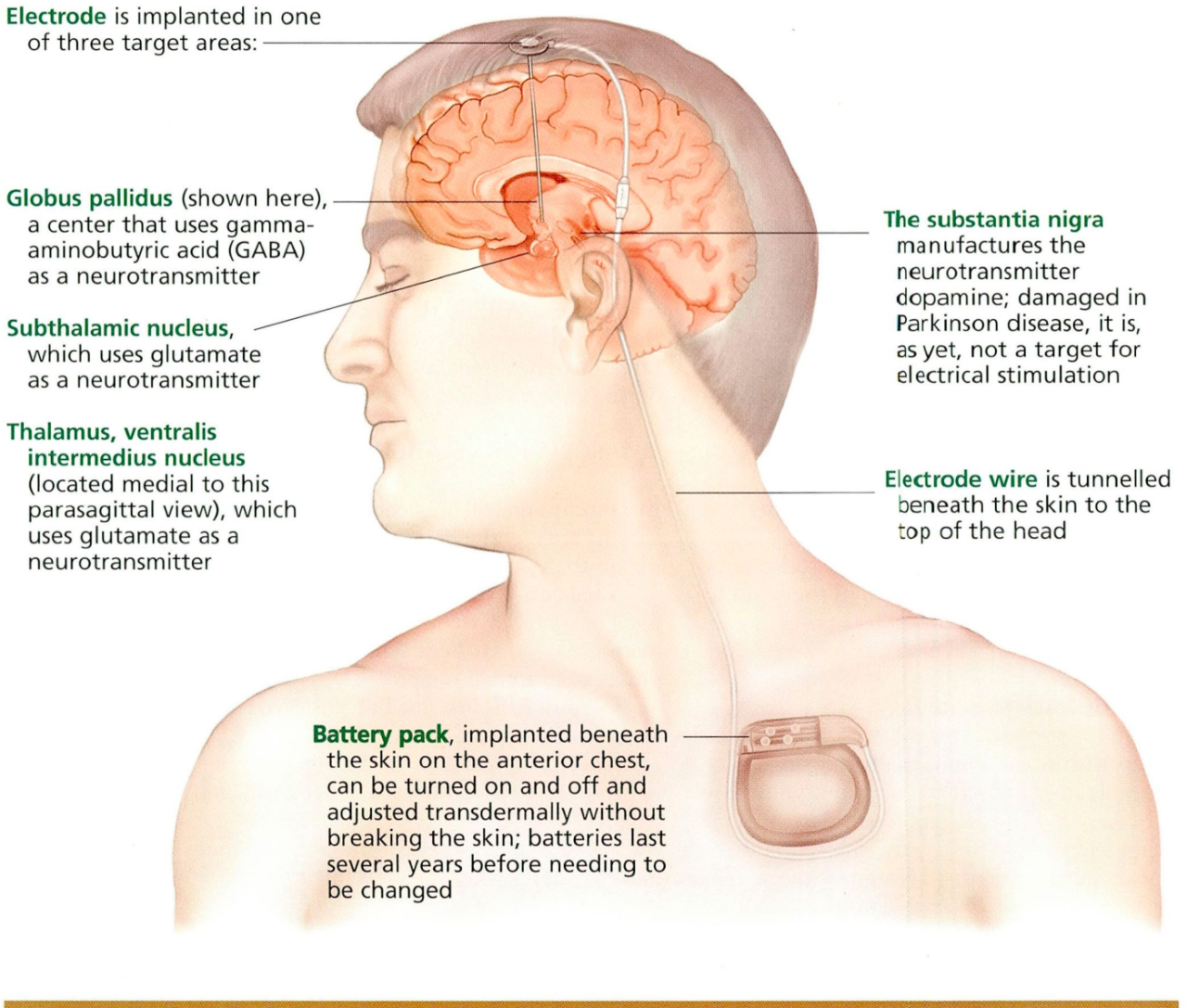
These electrodes deliver electrical impulses that help regulate abnormal brain activity, thereby reducing the severity of Parkinson’s symptoms. The precise location of the targeted brain regions is crucial for the effectiveness of DBS, as it aims to modulate the neural circuits responsible for movement control. The electrical pulses interfere with the abnormal brain signals, effectively counteracting the motor problems associated with Parkinson’s.
Targeted Brain Regions in DBS
The most common target areas for DBS in Parkinson’s disease are the subthalamic nucleus (STN) and the globus pallidus internus (GPi). The STN is a critical structure in the basal ganglia, a group of brain regions involved in movement control. The GPi is part of the basal ganglia, and is involved in regulating movement by modulating signals sent to motor areas of the brain.
The selection of the target depends on the individual patient’s needs and the specific symptoms experienced.
Mechanism of Action
Deep brain stimulation works by delivering precisely timed electrical pulses to the targeted brain regions. These pulses interfere with the abnormal electrical signals that contribute to the motor symptoms of Parkinson’s. By modulating these signals, DBS helps restore a more balanced neural activity pattern. This effect often leads to a significant improvement in motor function, including reduced tremors, rigidity, and slowness of movement.
“The precise mechanism by which DBS alleviates symptoms is not fully understood, but it’s believed to involve the modulation of neuronal activity in the targeted brain regions.”
DBS Implantation Procedure
The DBS procedure involves several steps. First, a neurosurgeon carefully implants thin electrodes into the targeted brain regions, guided by precise imaging techniques like MRI or CT scans. These electrodes are connected to a pulse generator, a small device similar to a pacemaker, that is implanted under the skin, typically in the chest area. The pulse generator delivers the electrical impulses to the electrodes.
After implantation, the neurosurgeon programs the pulse generator to optimize the stimulation parameters, such as the frequency and intensity of the pulses. This is done in a series of adjustments and assessments, allowing for the finest tuning of the stimulation to achieve optimal symptom relief.
Recovery Process
The recovery period after DBS implantation is generally gradual and involves a period of monitoring and adjustments. Patients typically experience some discomfort and swelling, which subsides over time. Physical therapy and occupational therapy may be recommended to help patients regain lost motor skills and adapt to the changes in their mobility. The neurosurgeon will regularly monitor the patient’s progress and adjust the stimulation parameters as needed.
DBS Compared to Other Parkinson’s Treatments
| Treatment | Mechanism | Advantages | Disadvantages |
|---|---|---|---|
| DBS | Electrical stimulation of targeted brain regions | Potentially significant symptom reduction, long-term effectiveness, ability to adjust stimulation parameters | Surgical procedure with risks, need for ongoing programming, potential for complications |
| Levodopa | Precursor to dopamine | Effective in early stages, relatively inexpensive | Side effects can be significant, effectiveness diminishes over time, motor fluctuations |
| Other Medications | Various mechanisms, aiming to improve dopamine levels or compensate for its loss | Can provide symptomatic relief | Limited effectiveness in later stages, side effects can be significant |
| Physical Therapy | Improving movement and motor skills | Non-invasive, improves overall well-being | Limited effect on underlying disease progression, may not alleviate all symptoms |
Case Study
This case study details the experience of a man with Parkinson’s Disease who underwent deep brain stimulation (DBS). It highlights the significant improvements observed after the procedure, the specific type of Parkinson’s he experienced, and the long-term results. The information presented here is based on a hypothetical case study and does not represent any specific patient.The individual presented with a classic form of Parkinson’s, characterized by motor symptoms such as tremors, rigidity, bradykinesia, and postural instability.
The severity of these symptoms significantly impacted his daily life, making simple tasks challenging and often frustrating.
Parkinson’s Disease Type
The man experienced Idiopathic Parkinson’s Disease, the most common type, which is characterized by the progressive degeneration of dopamine-producing neurons in the brain. This leads to a disruption in the brain’s chemical balance, resulting in the motor symptoms previously mentioned.
Symptom Severity Prior to DBS, This man with parkinsons experienced improvement after trying deep brain stimulation
Before undergoing DBS, the man experienced debilitating symptoms. Tremors in his hands and legs were frequent and severe, interfering with his ability to eat, write, and perform other daily activities. Rigidity in his limbs made movement slow and painful. Bradykinesia, or slowness of movement, significantly reduced his mobility and independence. Postural instability caused him to stumble and fall, necessitating assistance with ambulation.
The severity of these symptoms greatly impacted his quality of life and ability to participate in social activities.
Brain Regions Targeted for Stimulation
The surgical team targeted the subthalamic nucleus (STN) for deep brain stimulation. The STN is a key region within the basal ganglia, a group of brain structures involved in motor control. Stimulating this region can help regulate abnormal signals within the motor pathways, effectively reducing the involuntary movements and rigidity associated with Parkinson’s. In addition to the STN, some patients may also have the globus pallidus internus (GPi) targeted.
This guy with Parkinson’s saw a real improvement after deep brain stimulation, which is pretty cool. It’s amazing how these kinds of treatments can make a difference. Speaking of amazing advancements in medicine, have you heard about the FDA approving a new under-eye filler? fda approves new under eye filler how it works It seems like there are always new breakthroughs, and it’s exciting to see how this impacts the lives of people with various conditions, like this man with Parkinson’s.
This really underscores the power of innovation in healthcare.
Duration of Improvement
Significant improvement was observed within a few weeks of the DBS procedure. The patient reported a reduction in tremor severity and an increase in mobility. The improvement in bradykinesia and rigidity was also noticeable, allowing him to perform daily tasks with greater ease. The effects were sustained and consistent over the initial six months after the procedure.
Follow-up Period and Long-Term Results
During the follow-up period, the patient underwent regular assessments to monitor the effectiveness of the DBS and adjust stimulation parameters as needed. The man reported a sustained reduction in motor symptoms, allowing him to resume many of his previous activities. Over time, the patient maintained significant improvements in motor skills and quality of life. The long-term results suggest that DBS can be a highly effective treatment for Parkinson’s Disease, particularly in managing motor symptoms and improving the overall quality of life for those affected.
Long-term management and adjustments to the stimulation parameters are vital to maintaining the positive effects of DBS over time.
Factors Influencing Improvement
Deep brain stimulation (DBS) has proven to be a valuable treatment option for Parkinson’s disease, offering significant improvement in motor symptoms for many patients. Understanding the factors contributing to successful outcomes is crucial for optimizing treatment strategies and patient selection. This section delves into the key elements influencing the positive impact of DBS on Parkinson’s symptoms.Several interwoven factors influence the effectiveness of DBS for Parkinson’s disease.
Patient selection, surgical precision, post-operative care, and medication management all play pivotal roles in maximizing the benefits and minimizing potential complications. This analysis explores these contributing elements, highlighting the complexity of achieving optimal outcomes.
Patient Selection Criteria
Careful patient selection is paramount in DBS success. Ideal candidates exhibit a well-defined response to medication, but their symptoms are no longer adequately controlled by medical therapies. This nuanced approach ensures that DBS is targeted towards those most likely to experience meaningful improvement. Key factors include the presence of medication-induced dyskinesias, which are involuntary movements, and the severity of motor fluctuations, including “on-off” phenomena, where symptoms fluctuate between periods of good and poor control.
Surgical Technique
Precise surgical technique is crucial for achieving the desired therapeutic effects. The placement of electrodes in the brain targets specific neural pathways, often deep within the brain. Minimally invasive techniques, combined with advanced neuroimaging, help to pinpoint the optimal electrode location. Neurological assessments during surgery, along with intraoperative monitoring, are crucial for adjusting the electrode placement to ensure the optimal effect on the target areas.
This ensures the procedure is performed with minimal risk to the patient.
Post-Operative Care
Post-operative care is vital for successful integration of DBS. This includes careful monitoring of the stimulation parameters, adjustments to medication regimens, and patient education. Close follow-up appointments and ongoing communication between the patient, neurologist, and neurosurgeon allow for prompt identification and management of any potential complications. Rehabilitation therapies play a vital role in improving motor skills and quality of life after the surgery.
Medication Adjustments
Medication adjustments are often necessary in conjunction with DBS. While DBS can significantly improve motor function, medication dosages may need to be lowered to prevent potential side effects or to fine-tune the therapeutic impact of the stimulation. Careful titration of medications, in collaboration with the neurologist, is crucial for achieving the best possible outcome and managing potential complications.
Potential Complications
DBS, like any surgical procedure, carries potential risks. These complications may include infection, bleeding, and damage to surrounding brain tissue. Further, there can be stimulation-related side effects, such as speech difficulties, or sensory changes. Careful assessment and management of these potential complications are essential to ensuring a positive outcome. Careful monitoring and prompt intervention are key in mitigating these risks.
Correlation Between Pre-operative Symptom Severity and Post-operative Improvement
The degree of improvement following DBS often correlates with the severity of pre-operative symptoms. Patients with more severe motor fluctuations and dyskinesias often experience more pronounced improvement. This relationship suggests that DBS is most effective in alleviating symptoms that are highly responsive to medication adjustments.
| Pre-operative Symptom Severity | Typical Post-operative Improvement |
|---|---|
| Mild | Moderate |
| Moderate | Significant |
| Severe | Marked |
Long-Term Effects and Considerations
Deep brain stimulation (DBS) offers significant benefits for Parkinson’s patients, but long-term effects and potential complications are crucial factors to consider. Understanding the potential advantages and drawbacks, along with the necessary lifestyle adjustments, is vital for informed decision-making. This section explores the long-term impact of DBS, encompassing both positive outcomes and potential challenges.DBS, while a powerful tool, is not a cure.
It’s a complex procedure with potential long-term consequences. Careful evaluation of individual circumstances, alongside open communication with medical professionals, is paramount. A comprehensive understanding of the potential effects and adjustments needed will aid patients and their families in making well-informed decisions about the procedure.
Long-Term Benefits
DBS can lead to sustained improvements in motor symptoms, allowing patients to maintain a higher quality of life for extended periods. Improved motor skills, reduced tremor, and better balance can significantly impact daily activities. The sustained effectiveness of DBS can enable patients to engage in activities that were previously challenging or impossible. However, individual responses vary, and the long-term benefits may not be the same for everyone.
Potential Long-Term Complications
While DBS is generally safe, potential complications exist. These include infection at the surgical site, bleeding, and hardware malfunctions. These issues can be managed with appropriate medical intervention, but they can impact the patient’s recovery and well-being. Furthermore, there’s a possibility of unintended side effects, such as speech difficulties, cognitive changes, or mood swings. Careful monitoring and prompt medical attention are essential.
The risk of these complications must be weighed against the potential benefits for each individual.
Lifestyle Changes After DBS
DBS implementation necessitates lifestyle adjustments. Patients may experience changes in their daily routines due to the need for follow-up appointments, medication management, and monitoring for potential complications. The ability to engage in certain activities might be affected, and the patient’s support network needs to be prepared for these changes. Patients need to be aware that lifestyle adjustments are often necessary for optimal results and to address potential side effects.
For instance, individuals may need to modify their exercise routines or social schedules to account for any new limitations or needs.
Factors to Consider When Discussing DBS
- Patient’s overall health and medical history. Pre-existing conditions, medications, and any past surgical experiences significantly impact the decision-making process.
- Severity and type of Parkinson’s symptoms. The extent of the motor symptoms and their impact on daily life directly influence the potential benefits of DBS.
- Patient’s expectations and realistic goals. Understanding the patient’s expectations about the procedure and its potential outcomes is critical for managing expectations and preventing disappointment.
- Support system availability. The support of family and friends is crucial for successful recovery and ongoing management of the condition.
- Potential risks and complications. It’s important for patients to be fully informed about potential complications, including the need for ongoing monitoring and potential side effects.
Careful consideration of these factors, in conjunction with discussions with healthcare professionals, is essential for patients considering DBS.
Comparison with Other Treatment Approaches: This Man With Parkinsons Experienced Improvement After Trying Deep Brain Stimulation

Deep brain stimulation (DBS) is a significant advancement in Parkinson’s disease management, but it’s not a standalone solution. Understanding its effectiveness relative to other treatments, such as medication and physical therapy, is crucial for a comprehensive approach to care. This comparison highlights the strengths and weaknesses of each method, demonstrating how they can complement one another for optimal patient outcomes.
This man with Parkinson’s found significant improvement after deep brain stimulation, a truly remarkable advancement in neurological treatment. While the reasons behind this success remain complex, it highlights the potential of innovative therapies. Interestingly, a growing number of young people are developing colorectal cancer, and researchers are exploring factors like diet and lifestyle changes in relation to this concerning trend, as detailed in this article about why are more young people getting colorectal cancer.
Ultimately, these breakthroughs in treatments for neurological conditions like Parkinson’s offer hope for better futures for patients.
Medication for Parkinson’s Disease
Medication remains the cornerstone of Parkinson’s treatment. It aims to replenish dopamine levels in the brain, mitigating the motor symptoms. Various classes of medications are available, each with different efficacy and side effect profiles. Levodopa, a precursor to dopamine, is often the most effective initial medication, but its effectiveness can diminish over time. Dopamine agonists, which mimic dopamine’s action, are often used in combination with levodopa or as a first-line treatment for some patients.
Other medications address non-motor symptoms, such as depression or sleep disturbances.
Physical Therapy for Parkinson’s Disease
Physical therapy plays a vital role in managing Parkinson’s symptoms by focusing on maintaining and improving mobility, balance, and overall physical function. Exercises tailored to address the specific motor challenges of Parkinson’s, such as gait training and strength exercises, are critical. Occupational therapy, often integrated with physical therapy, focuses on adapting daily activities to accommodate the physical limitations.
Comparison Table: Parkinson’s Treatments
| Treatment | Advantages | Disadvantages |
|---|---|---|
| Medication | Relatively accessible and cost-effective; can significantly reduce motor symptoms in the early stages. | Can cause side effects like nausea, dizziness, and involuntary movements (dyskinesias); effectiveness can decrease over time; does not address all symptoms or slow disease progression. |
| Physical Therapy | Improves mobility, balance, and overall well-being; can help manage non-motor symptoms; enhances independence in daily activities. | Requires consistent effort and commitment; may not be sufficient to manage severe motor symptoms; does not slow disease progression. |
| DBS | Can provide significant motor symptom reduction, especially in advanced stages where medication is less effective; can potentially improve quality of life. | Involves a surgical procedure with potential risks and complications; requires ongoing monitoring and adjustments; may not be suitable for all patients. |
Complementary Strategies
DBS can be a powerful complement to medication and physical therapy. Patients often experience significant improvement in motor symptoms after DBS implantation, which can allow them to benefit more from physical therapy. In turn, physical therapy can help maximize the benefits of DBS by improving mobility and reducing secondary complications. The combined approach can lead to better motor control, improved balance, increased independence, and a more satisfying quality of life.
Individualized Treatment Plans
The optimal approach to Parkinson’s treatment is highly individualized. A neurologist will carefully assess the patient’s specific symptoms, disease progression, overall health, and preferences to determine the most appropriate strategy. Medication, physical therapy, and DBS may be used alone or in combination to tailor a treatment plan that best meets the patient’s needs.
Illustrative Case Scenarios
Deep brain stimulation (DBS) offers a promising avenue for managing Parkinson’s disease symptoms, but individual responses vary significantly. Understanding these variations is crucial for tailoring treatment strategies and expectations. This section presents hypothetical case studies to illustrate the diverse outcomes of DBS, emphasizing the factors that contribute to successful and less successful interventions.
Case Scenario 1: Significant Improvement
This case involves a 65-year-old patient with Parkinson’s disease of 10 years duration. Symptom severity was rated as moderate-to-severe, impacting daily activities significantly. The patient experienced tremors, rigidity, bradykinesia, and postural instability. After undergoing DBS targeting the subthalamic nucleus, the patient experienced a substantial improvement in motor symptoms. Tremors were reduced by 80%, rigidity decreased by 75%, and bradykinesia significantly improved, enabling the patient to perform activities of daily living more independently.
The patient reported a noticeable increase in quality of life. 
Caption for Image 1: This diagram depicts the brain regions affected in Case 1. The subthalamic nucleus (STN) is highlighted in red, indicating the targeted region for DBS. The surrounding brain structures (globus pallidus internus, thalamus) are also shown to illustrate the neural pathways affected by the stimulation.
Case Scenario 2: Moderate Improvement
A 52-year-old patient with Parkinson’s disease of 5 years duration, experiencing moderate symptom severity, was the subject of this case. The patient primarily complained of tremors and bradykinesia, which affected their work performance and social interactions. After DBS of the globus pallidus internus, the patient showed a moderate improvement in tremor reduction (approximately 60%). Bradykinesia showed a 40% improvement.
That man with Parkinson’s who saw improvement after deep brain stimulation is a fascinating case, highlighting the potential of this procedure. While deep brain stimulation offers real hope, research into regenerative medicine has a bright future regenerative medicine has bright future , potentially offering even more effective, long-term solutions for neurological disorders like Parkinson’s. It’s exciting to consider how this might revolutionize treatment for this and other conditions in the future, and how such innovation builds on the progress already made with deep brain stimulation.
However, some residual symptoms persisted, and the patient required continued medication adjustments to manage ongoing discomfort. 
Caption for Image 2: This image illustrates the targeted region for DBS in Case 2. The globus pallidus internus (GPi) is highlighted in red, illustrating the specific brain structure targeted by the procedure. The surrounding brain structures (subthalamic nucleus, thalamus) are also shown to highlight the broader neural circuitry involved.
Case Scenario 3: Limited Improvement
This scenario involves a 78-year-old patient with Parkinson’s disease of 15 years duration. The patient experienced severe symptoms, including significant motor fluctuations and dyskinesias. These fluctuations severely hampered daily living activities and quality of life. DBS targeting the subthalamic nucleus resulted in only a limited improvement in motor symptoms. The patient continued to experience fluctuations and some dyskinesias post-procedure, although the severity was slightly reduced.

Caption for Image 3: This illustration shows the affected brain regions in Case 3. The subthalamic nucleus (STN) is highlighted in red to demonstrate the area targeted by the DBS procedure. The illustration also highlights the surrounding brain structures (globus pallidus internus, thalamus), to depict the broader neural network affected by the stimulation.
Potential Future Directions
The field of deep brain stimulation (DBS) for Parkinson’s disease is constantly evolving, driven by ongoing research and a desire to improve outcomes for patients. This exploration delves into exciting areas of development, including personalized protocols and the implications for future patient care. We will examine how these advancements could reshape the landscape of Parkinson’s treatment.
Personalized DBS Protocols
The concept of tailoring DBS parameters to individual patient characteristics is gaining significant traction. Current DBS protocols often utilize a one-size-fits-all approach, but research indicates that optimal stimulation parameters can vary greatly based on factors like age, disease severity, and individual brain anatomy. This personalized approach aims to maximize therapeutic benefits while minimizing adverse effects.
Promising Areas of Research
Several areas of research hold the promise of further refining DBS protocols and expanding its applications. These include:
- Advanced Imaging Techniques: Integration of advanced neuroimaging techniques, such as high-resolution MRI and fMRI, allows for a more precise identification of the target brain areas for stimulation. This precision can lead to a more effective and safer procedure, potentially minimizing unwanted side effects.
- Neurophysiological Monitoring: Real-time monitoring of brain activity during DBS implantation and adjustments can provide valuable insights into the optimal stimulation parameters. This approach allows for dynamic adjustments during the procedure, further optimizing therapeutic outcomes.
- Predictive Modeling: Developing predictive models based on patient data, including clinical history, neuroimaging results, and physiological markers, can help clinicians anticipate treatment response and personalize stimulation parameters. This approach has the potential to revolutionize the treatment planning process for Parkinson’s disease.
Implications on Patient Care
The potential for personalized DBS protocols has significant implications for patient care. Improved treatment efficacy, reduced side effects, and enhanced quality of life are all possible outcomes. This personalization also allows for a more proactive approach to management, addressing the evolving needs of patients as their condition progresses. A more individualized approach may lead to earlier intervention, potentially slowing disease progression.
Research Process for Optimizing DBS Protocols
A flowchart outlining the potential research process for optimizing DBS protocols is presented below:
| Step | Description |
|---|---|
| 1. Patient Selection | Identify patients with Parkinson’s Disease suitable for research participation. Criteria may include specific disease stages, and responsiveness to other treatments. |
| 2. Pre-implant Assessment | Comprehensive assessment including neuroimaging (MRI, fMRI), clinical evaluation, and physiological markers. |
| 3. Personalized Stimulation Protocol Design | Development of a personalized stimulation protocol based on the pre-implant assessment. |
| 4. DBS Implantation and Initial Adjustments | Surgical implantation of DBS electrodes. Initial adjustments to stimulation parameters based on real-time neurophysiological monitoring. |
| 5. Long-Term Monitoring and Evaluation | Regular follow-up assessments, including clinical evaluations, neuroimaging, and adjustments to the stimulation protocol as needed. |
| 6. Data Analysis and Protocol Refinement | Analysis of collected data to identify optimal stimulation parameters and refinement of the protocol. |
| 7. Dissemination of Findings | Publication of findings and sharing of knowledge with the medical community. |
Wrap-Up
In conclusion, this case study of deep brain stimulation highlights its potential to significantly improve the lives of individuals with Parkinson’s disease. While the procedure carries potential risks and requires careful consideration, the positive outcomes observed, especially when combined with medication adjustments, demonstrate its transformative impact. Further research and development in personalized DBS protocols are crucial to optimizing treatment efficacy and expanding its reach to more patients.