
Treating breast feeding thrush – Treating breastfeeding thrush is a crucial aspect of ensuring a healthy and comfortable breastfeeding experience for both mother and baby. This guide delves into the various facets of understanding, diagnosing, and managing thrush, providing actionable steps for a successful breastfeeding journey. We’ll cover everything from the causes and symptoms to effective treatment options and preventative measures.
Understanding the nuances of thrush in breastfeeding mothers and infants is essential. This involves recognizing the distinct signs and symptoms in both, comparing them to other potential breastfeeding complications, and comprehending the impact on the breastfeeding relationship. The importance of a proper diagnosis and a collaborative approach with healthcare professionals will also be highlighted.
Understanding Breastfeeding Thrush
Breastfeeding is a beautiful and rewarding experience, but sometimes, challenges like thrush can arise. This condition, a yeast infection, can affect both the breastfeeding mother and the infant, disrupting the bonding and feeding process. Understanding the causes, symptoms, and risk factors can help mothers proactively manage this common issue.Thrush, medically known as candidiasis, is a fungal infection caused by the overgrowth of a yeast calledCandida albicans*.
It’s a prevalent issue among breastfeeding mothers and their infants, and its impact on the breastfeeding relationship can be significant. This guide will explore the intricacies of breastfeeding thrush, focusing on the causes, signs, symptoms, and the impact it has on the breastfeeding experience.
Dealing with breast-feeding thrush can be tricky, but thankfully, there are some natural remedies that can help. While exploring different options, it’s worth noting the subtle differences between black raspberries and regular raspberries – check out this helpful comparison to understand the nuances of each black raspberry vs raspberry. Ultimately, understanding these distinctions can help you make informed decisions about potential remedies for breast-feeding thrush.
Causes of Thrush in Breastfeeding Mothers and Infants
Yeast infections, like thrush, can occur when the natural balance of microorganisms in the body is disrupted. In breastfeeding mothers, this imbalance can be triggered by various factors. For instance, hormonal changes during pregnancy and breastfeeding can create an environment more conducive to yeast overgrowth. Weakened immune systems, or concurrent illnesses, can also increase the susceptibility to thrush.
Similarly, in infants, thrush can develop due to a disruption of their delicate gut flora, possibly due to antibiotic use or an immature immune system. Additionally, if the mother has thrush, the infant can be exposed to the infection through breastfeeding.
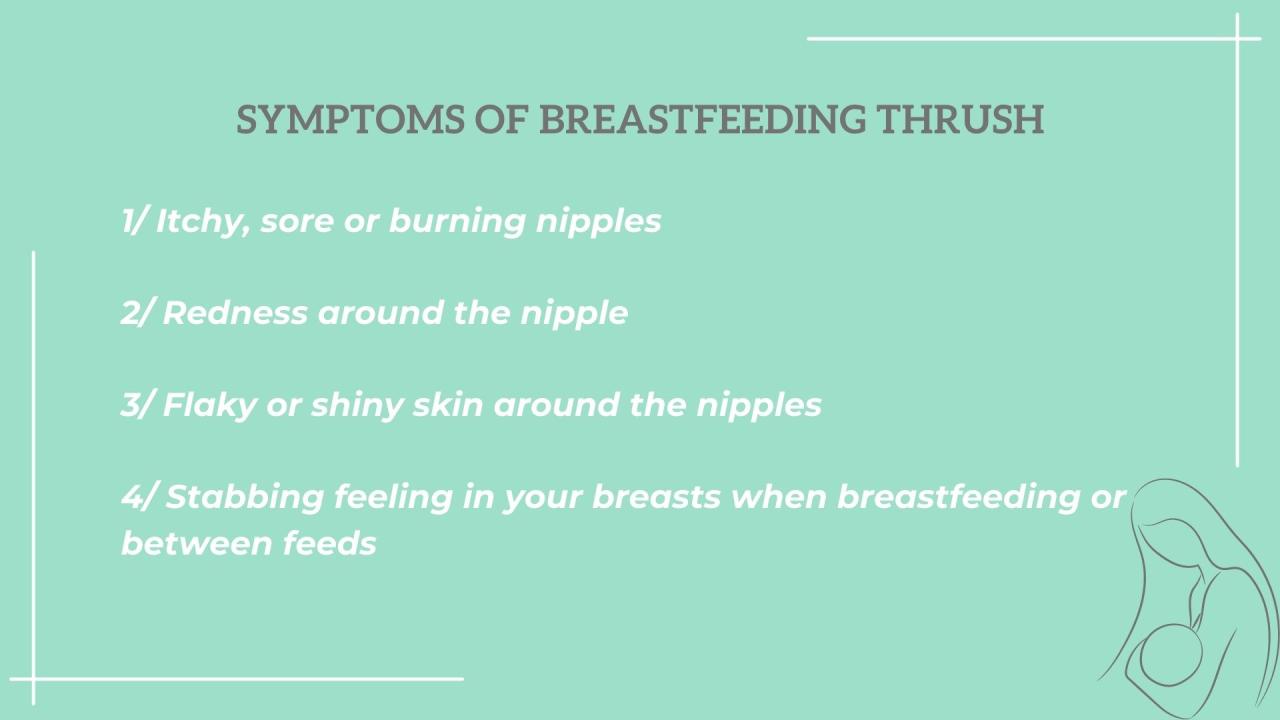
Signs and Symptoms of Thrush
The presentation of thrush varies between mothers and infants. In mothers, thrush typically manifests as painful, red, and cracked nipples. The nipples might also appear inflamed or swollen, and there may be a burning sensation during or after breastfeeding. In infants, thrush often presents as white, cheesy patches on the tongue, inside the mouth, or on the palate.
These patches might also be observed on the cheeks, gums, and roof of the mouth. The infant may experience discomfort and fussiness during feedings, and the symptoms may sometimes include difficulty swallowing.
Risk Factors for Thrush Development
Several factors increase the risk of developing thrush during breastfeeding. These include a weakened immune system, use of antibiotics, stress, and poor oral hygiene. Furthermore, prolonged use of oral contraceptives or hormonal medications can also increase the likelihood of a yeast infection. Mothers with a history of yeast infections are also at higher risk. Maintaining good hygiene practices, particularly for the mother’s nipples and the infant’s mouth, can significantly reduce the risk.
Types of Thrush Infections Relevant to Breastfeeding
While
Dealing with breast feeding thrush can be tricky, but thankfully there are effective treatments available. However, it’s crucial to be mindful of potential side effects, especially when considering medication. For instance, some commonly prescribed mood stabilizing drugs, like those discussed in this article on common mood stabilizing drug can increase risk of birth defects , might carry risks for developing birth defects.
So, it’s always best to discuss treatment options with your doctor to ensure both you and your baby are safe and healthy during this special time.
- Candida albicans* is the most common cause of thrush, other
- Candida* species can also contribute. The specific type of
- Candida* species involved may not always be clinically relevant, as the symptoms and management strategies remain largely consistent across different types of thrush. The primary focus remains on treating the infection and preventing its spread.
Impact of Thrush on the Breastfeeding Relationship
Thrush can significantly impact the breastfeeding relationship. The pain and discomfort associated with thrush can make breastfeeding extremely challenging and painful for the mother, potentially leading to decreased milk production or a reluctance to breastfeed. In infants, thrush can cause discomfort and difficulty feeding, affecting the infant’s growth and development. Early diagnosis and treatment are crucial to mitigate the impact on both the mother and the infant.
Symptoms of Thrush in Mothers and Infants
| Symptom | Mother | Infant | Description |
|---|---|---|---|
| Nipple Pain | Yes | No | Sore, burning, or stinging sensation during or after breastfeeding. |
| Redness | Yes | No | Inflammation and redness of the nipple. |
| Cracked Nipples | Yes | No | Visible fissures and cracks on the nipples. |
| White Patches | No | Yes | Thick, white, and cheesy patches on the infant’s mouth. |
| Fussiness | No | Yes | Infant is irritable and uncomfortable during feeding. |
| Difficulty Swallowing | No | Yes | Infant struggles to take in milk or shows signs of discomfort during feeding. |
Diagnosis and Assessment
Accurately diagnosing breastfeeding thrush is crucial for effective treatment, both for the mother and the baby. A proper diagnosis ensures the right course of action and prevents the spread of infection. This involves identifying the specific cause of the symptoms and ruling out other potential issues.Proper diagnosis is vital because it guides the choice of treatment. Treating thrush with the wrong medication, or failing to address an underlying condition, can lead to ineffective treatment, prolonged discomfort, and potential complications.
A missed diagnosis can also result in a mother or baby experiencing unnecessary suffering and the potential for a more serious issue.
Diagnostic Process for Breastfeeding Thrush
Identifying thrush involves a multifaceted approach, combining visual observation with sample collection and potentially further testing. The key is to identify the characteristic signs and symptoms while ruling out other possibilities.
Methods for Diagnosing Thrush
A thorough assessment begins with a visual examination. This involves careful inspection of the affected areas. For the mother, this includes the nipples, areola, and surrounding skin. For the baby, this includes the mouth, tongue, and gums. Visual examination helps to identify characteristic white patches, redness, cracking, or soreness.In addition to visual examination, sample collection plays a significant role.
A sample can be taken from the affected area for laboratory analysis. For the mother, this might involve collecting a swab from the nipple or areola. For the baby, a sample may be taken from the mouth using a sterile cotton swab. The sample is then sent to a laboratory to be examined under a microscope for the presence of the yeastCandida albicans*.
This helps confirm the diagnosis and distinguish it from other conditions.
Importance of Proper Diagnosis
An accurate diagnosis is essential for effective treatment. It ensures that the correct medication is prescribed, and that any underlying conditions are addressed. Misdiagnosis can lead to ineffective treatment, prolonging the discomfort and potentially impacting breastfeeding success.
Differentiating Thrush from Other Conditions
Breastfeeding mothers and infants can experience a variety of issues that mimic thrush symptoms. Differentiating thrush from other conditions is vital for providing the appropriate treatment. Symptoms like cracked nipples, soreness, or white patches in the mouth can also be associated with other breastfeeding challenges, like latch issues or skin irritations. Accurate diagnosis requires a medical professional to distinguish between various conditions.
Medical Professional’s Role in Diagnosis
A healthcare provider is essential in diagnosing thrush. They can conduct a thorough examination, collect appropriate samples, and interpret the results. They are trained to distinguish thrush from other conditions that may present similar symptoms. This professional expertise is crucial in ensuring the most appropriate and effective treatment plan is implemented.
Comparison of Thrush Symptoms with Other Common Breastfeeding Complications
| Symptom | Thrush | Cracked Nipples | Mastitis |
|---|---|---|---|
| Appearance | White patches, redness, soreness, possible burning | Cracks, redness, soreness, possible bleeding | Redness, swelling, tenderness, warmth, sometimes fever |
| Location | Nipples, areola, inside mouth | Nipples, areola | Breast tissue |
| Associated Factors | Yeast infection | Improper latch, friction | Bacterial infection, blocked milk ducts |
| Treatment | Antifungal medication | Lanolin, nipple shields, improved latch technique | Antibiotics, pain relief, rest, warm compresses |
Treatment Options
Treating breastfeeding thrush requires a multi-faceted approach, focusing on both the mother and the infant. Effective treatment involves addressing the infection promptly and consistently to prevent reoccurrence and discomfort for both individuals. The goal is to eliminate the fungus and restore healthy oral conditions for everyone involved.
Antifungal Medications
A variety of antifungal medications are commonly prescribed for treating thrush in breastfeeding mothers and infants. These medications work by targeting the fungal cells, inhibiting their growth, and ultimately eliminating the infection. The choice of medication often depends on factors such as the severity of the infection, the age of the infant, and any potential drug interactions.
Treatment Regimens for Mothers
Consistent adherence to the prescribed treatment regimen is crucial for successful thrush treatment. This involves taking the medication as directed, for the full duration of the treatment course. Failure to complete the full course can lead to incomplete eradication of the fungus, potentially resulting in a relapse or the development of drug resistance. Furthermore, this adherence is important to ensure that the medication reaches the necessary therapeutic levels to eliminate the infection effectively.
Regular monitoring and communication with the healthcare provider are essential throughout the treatment process.
Treating breastfeeding thrush can be tricky, and sometimes you need a doctor’s expertise. But, does a doctor’s age really impact their ability to provide effective care? The question of whether a doctor’s experience outweighs their age is a valid one, and it’s something worth considering. For instance, should doctors age matter when it comes to diagnosing and treating something as sensitive as breastfeeding thrush?
Ultimately, the most important factor is the doctor’s knowledge and experience in handling the specific condition, regardless of their age.
Treatment Regimens for Infants
Treatment regimens for infants are tailored to their age and health conditions. The dosage and duration of treatment will vary depending on the severity of the infection and the specific antifungal medication prescribed. Parental vigilance and consistent administration of the medication as directed by the healthcare provider are crucial for successful treatment outcomes. Close monitoring of the infant’s response to treatment and reporting any adverse reactions to the healthcare provider are critical for optimal management.
Comparison of Antifungal Medications
Different antifungal medications may vary in their effectiveness and safety profiles for breastfeeding mothers. Factors like potential drug interactions with other medications, the infant’s age, and any pre-existing medical conditions are considered when selecting the most suitable option. For example, some medications may have a higher risk of side effects in infants, so a healthcare professional will carefully evaluate the risks and benefits before prescribing a particular medication.
The healthcare provider will guide the choice of medication based on their expertise and knowledge of the specific circumstances.
Duration of Treatment
The typical duration of treatment for thrush in breastfeeding mothers and infants can vary, depending on the severity of the infection and the response to treatment. Generally, treatment lasts for a period of 7 to 14 days, but in some cases, it may be longer. The healthcare provider will determine the appropriate duration based on the individual’s response to treatment.
Successful eradication of the infection is often confirmed by the absence of symptoms after the completion of the prescribed course of treatment.
Antifungal Medication Table
| Antifungal Medication | Dosage | Potential Side Effects | Important Considerations |
|---|---|---|---|
| Clotrimazole | Various formulations; often applied topically. | Possible skin irritation, burning, or itching at the application site. | Can be effective for mild cases; may not be suitable for severe infections. |
| Miconazole | Oral or topical formulations. | Possible gastrointestinal upset (nausea, vomiting, diarrhea) in some individuals. | Can be effective for various severities of thrush. Consult healthcare provider for dosage and administration instructions. |
| Fluconazole | Oral; various dosages based on severity. | Possible headache, dizziness, or stomach upset. | Often used for more severe infections; may have potential interactions with other medications. |
Management Strategies
Navigating breastfeeding thrush requires a multifaceted approach that extends beyond simply treating the infection. Effective management involves supportive care for the mother, meticulous hygiene practices, and strategies to maintain a positive breastfeeding experience. Addressing the pain and discomfort, and proactively preventing recurrence are crucial for a smooth recovery and continued breastfeeding success.
Supportive Care Measures
Breastfeeding mothers experiencing thrush often experience discomfort and tenderness. Supportive care is paramount to ensure comfort and facilitate continued breastfeeding. This includes providing emotional support, ensuring adequate nutrition, and encouraging rest. Adequate hydration is vital for both the mother and the baby, and maintaining a healthy diet rich in vitamins and minerals can help the body’s natural healing process.
Proper rest and stress management are also crucial, as stress can impact the body’s immune response.
Proper Hygiene Practices
Maintaining meticulous hygiene is essential to prevent thrush transmission and recurrence. This includes regular cleaning of the breasts and nipples, using gentle and non-irritating cleansers, and ensuring proper handwashing techniques before and after handling the baby. Avoiding harsh soaps, lotions, or creams on the breasts can further minimize irritation. Frequent and thorough cleaning can significantly reduce the risk of reinfection and prevent the spread of the infection.
Maintaining a Healthy Breastfeeding Relationship
Maintaining a positive breastfeeding relationship during treatment is vital for the emotional well-being of both the mother and the baby. Open communication with healthcare providers and lactation consultants is essential. The mother should be encouraged to express milk regularly, whether through hand expression or a pump, to maintain milk supply while avoiding pain or discomfort. Maintaining a supportive and understanding environment for the mother is paramount.
Continued breastfeeding, with careful attention to hygiene, can help to reduce the risk of thrush recurrence.
Addressing Pain and Discomfort
Thrush can cause significant pain and discomfort for breastfeeding mothers. Using soft, breathable fabrics for nursing bras and tops, avoiding tight clothing, and applying cool compresses to the nipples can help alleviate discomfort. Over-the-counter pain relievers, as directed by a healthcare professional, can also be helpful in managing pain. If pain persists or worsens, it is crucial to consult a healthcare professional for further evaluation and treatment.
Preventing Thrush Recurrence
Preventing thrush recurrence involves a proactive approach to hygiene and lifestyle. Maintaining good oral hygiene for both the mother and the baby is essential. Using a soft-bristled toothbrush, brushing gently, and avoiding harsh chemicals in mouthwash can help reduce the risk of thrush in the oral cavity. Proper hygiene practices for the baby, including wiping the mouth after feeding, can also contribute to preventing recurrence.
Monitoring for any signs of recurrence, such as white patches or soreness, is essential to address the issue promptly.
Hygiene Practices for Breastfeeding Mothers and Infants
| Hygiene Practice | Breastfeeding Mother | Infant | Specific Examples |
|---|---|---|---|
| Oral Hygiene | Brush teeth gently with a soft-bristled toothbrush, avoiding harsh chemicals in mouthwash. | Clean the mouth with a soft, damp cloth after feeding. | Use fluoride toothpaste if appropriate. Avoid harsh chemicals in mouthwash. |
| Breast Care | Clean nipples with mild soap and water, avoiding harsh soaps and lotions. | Clean the baby’s mouth with a soft, damp cloth after feeding. | Use warm compresses for sore nipples. Avoid tight clothing or bras. |
| Handwashing | Wash hands thoroughly with soap and water before and after handling the baby and breasts. | Clean the baby’s hands after feeding and before handling. | Use antibacterial soap if appropriate, especially in high-risk situations. |
| Clothing | Wear loose-fitting, breathable clothing. | Ensure clothing is clean and free from irritants. | Avoid tight bras, use nursing tops. Change baby’s clothes as needed. |
Prevention Strategies: Treating Breast Feeding Thrush
Breastfeeding thrush, while often manageable, can be frustrating for both mothers and babies. Proactive prevention is key to minimizing the risk of recurrent infections and ensuring a smooth breastfeeding journey. Understanding the contributing factors and implementing preventative measures can significantly reduce the likelihood of thrush development.Effective prevention strategies go beyond simply treating an existing infection; they focus on maintaining a healthy environment for both mother and infant.
This involves meticulous attention to oral hygiene, identifying potential risk factors, and adopting optimal feeding techniques. By understanding these factors, mothers can proactively create a protective shield against thrush.
Maintaining Oral Hygiene
Maintaining impeccable oral hygiene for both the mother and infant is crucial in preventing thrush. Proper oral hygiene practices help remove potential breeding grounds for the yeast that causes thrush. This is particularly important for mothers as oral thrush can be easily transmitted to their infants during breastfeeding.
- Mothers should brush their teeth and tongue thoroughly, especially after meals, to remove food particles and bacteria.
- Mothers should practice good oral hygiene routines, including flossing and using mouthwash as recommended by dentists.
- Infants should have their gums and mouths cleaned gently with a soft, damp cloth after each feeding, especially for babies who are not yet teething.
Identifying and Addressing Potential Risk Factors
Certain factors can increase the susceptibility to thrush. Identifying and mitigating these risks is essential for preventing recurrences.
- Recognizing and treating underlying medical conditions, such as weakened immune systems or diabetes, can help prevent thrush.
- Proper use of antibiotics or other medications can help minimize their impact on the oral flora and prevent yeast overgrowth.
- Maintaining good overall health, including a balanced diet rich in probiotics and prebiotics, can contribute to a stronger immune response.
Proper Latch and Feeding Techniques
Optimal latch and feeding techniques are vital in preventing thrush transmission. A proper latch ensures effective milk transfer and minimizes the risk of injury or irritation in the mother’s nipples and the infant’s mouth.
- A well-established latch reduces the risk of damage to the nipple, preventing the entry of yeast into the bloodstream.
- A proper latch allows for a consistent and effective milk flow, avoiding milk pooling in the baby’s mouth which could potentially promote the growth of bacteria.
- Ensuring a good latch can prevent excessive irritation of the nipples, a common precursor to thrush development. Seeking guidance from a lactation consultant can help ensure proper technique.
Addressing Underlying Medical Conditions
Certain medical conditions can increase a person’s susceptibility to thrush. Addressing these conditions is crucial for preventing recurrences.
- Women with weakened immune systems, such as those undergoing chemotherapy or those with autoimmune disorders, may be more prone to thrush.
- Diabetes can impact the balance of the oral microbiome, increasing the risk of yeast overgrowth.
- Chronic conditions or those requiring prolonged use of certain medications, like steroids, can also influence susceptibility to thrush.
Preventative Measures Table
| Preventative Measure | Rationale | Examples | Impact |
|---|---|---|---|
| Thorough oral hygiene | Removes potential food particles and bacteria that could promote yeast growth. | Brushing teeth and tongue, flossing, and using mouthwash | Reduces the risk of thrush. |
| Addressing underlying medical conditions | Conditions like diabetes or weakened immune systems can increase susceptibility to thrush. | Managing diabetes effectively, consulting with healthcare providers about immune-suppressing conditions. | Reduces the risk of recurrence and severity of thrush. |
| Optimal latch and feeding techniques | Proper latch minimizes nipple damage, preventing entry points for yeast. | Seeking lactation consultant support, practicing correct latch positioning. | Minimizes the risk of thrush development and ensures effective milk transfer. |
| Balanced diet rich in probiotics and prebiotics | Supports a healthy microbiome and immune response. | Eating yogurt, kefir, or other probiotic-rich foods. | Strengthens the body’s defense against thrush. |
Follow-up and Monitoring
Following a thrush diagnosis, consistent monitoring and follow-up appointments are crucial for both the breastfeeding mother and her infant. This proactive approach ensures the treatment is effective, prevents complications, and allows for timely adjustments if needed. Regular check-ins with a healthcare provider are essential for navigating the treatment process successfully.Effective treatment hinges on diligent follow-up. Monitoring the infant’s response to treatment and the mother’s healing process is vital to ensure complete eradication of the infection and to prevent recurrence.
By actively participating in follow-up appointments, breastfeeding mothers can actively manage the condition and minimize potential setbacks.
Importance of Follow-up Appointments
Regular follow-up appointments are essential to assess the effectiveness of the treatment and to address any potential complications promptly. They provide an opportunity to discuss any concerns, modify the treatment plan if necessary, and ensure both the mother and infant are responding well to the therapy. This proactive approach helps prevent long-term issues and promotes successful breastfeeding.
Monitoring Treatment Effectiveness
Close monitoring is critical to evaluate the treatment’s efficacy. Symptoms like redness, soreness, or cracking should significantly diminish or disappear with appropriate treatment. A healthcare provider will examine both the mother’s nipples and the infant’s mouth for signs of thrush. A visual inspection, combined with a physical examination, allows for a comprehensive evaluation of the healing process.
This allows for a timely adjustment to the treatment plan if necessary.
Addressing Treatment Failures or Complications
Treatment failures or complications can arise for various reasons. If symptoms persist or worsen despite appropriate treatment, a healthcare provider should be consulted immediately. Potential complications could include a deeper infection, resistance to the medication, or a secondary infection. Addressing these issues promptly is crucial to prevent further complications and ensure a positive outcome for both the mother and infant.
Resources for Continued Support
Several resources can offer ongoing support and information for breastfeeding mothers facing thrush. Lactation consultants, support groups, and online forums can provide valuable insights and guidance. These communities can offer practical advice, emotional support, and a sense of connection with other mothers navigating similar experiences.
Signs and Symptoms to Watch For
During follow-up appointments, close attention should be paid to the following signs and symptoms: Continued pain or discomfort in the nipples, persistent white patches in the infant’s mouth, difficulty feeding, or a change in the infant’s behavior (e.g., fussiness or decreased appetite). These observations help identify any potential issues and allow for prompt intervention.
Follow-up Appointment Timeline, Treating breast feeding thrush
| Appointment Number | Anticipated Outcomes | Potential Issues | Action Plan |
|---|---|---|---|
| 1 (Initial) | Diagnosis confirmation, initial treatment plan established | No improvement in symptoms, suspicion of secondary infection | Adjust treatment, consider additional tests, refer to specialist |
| 2 (Week 1-2) | Assessment of initial treatment response, modification if needed | Symptoms persist, treatment failure, new symptoms emerge | Modify treatment, consider alternative medications, refer to specialist |
| 3 (Week 3-4) | Full resolution of symptoms, prevention strategies discussed | Recurrence of symptoms, discomfort during feeding | Review feeding techniques, explore different nursing positions, address any contributing factors |
Closure

In conclusion, treating breastfeeding thrush requires a multifaceted approach encompassing understanding the causes, proper diagnosis, effective treatment, and proactive management strategies. Maintaining open communication with healthcare providers is key. By following the preventative measures and supportive care strategies Artikeld in this guide, you can significantly reduce the risk of thrush and foster a healthy and happy breastfeeding experience. Remember, early intervention and adherence to treatment plans are crucial for successful management.
