Trigger point injections for migraines offer a potential new avenue for pain relief, but what exactly are they? This comprehensive guide explores the ins and outs of TPIs, delving into the mechanisms behind their effectiveness, the procedures involved, and the potential outcomes. We’ll also consider patient selection, potential risks and benefits, alternative therapies, and future research.
Trigger point injections for migraines target specific muscle trigger points believed to be contributing to migraine attacks. Understanding how these injections work, the types of muscles often involved, and the procedure itself is key to making an informed decision about this treatment option. We’ll compare TPIs to other migraine treatments, helping you weigh the pros and cons.
Trigger Point Injections for Migraines
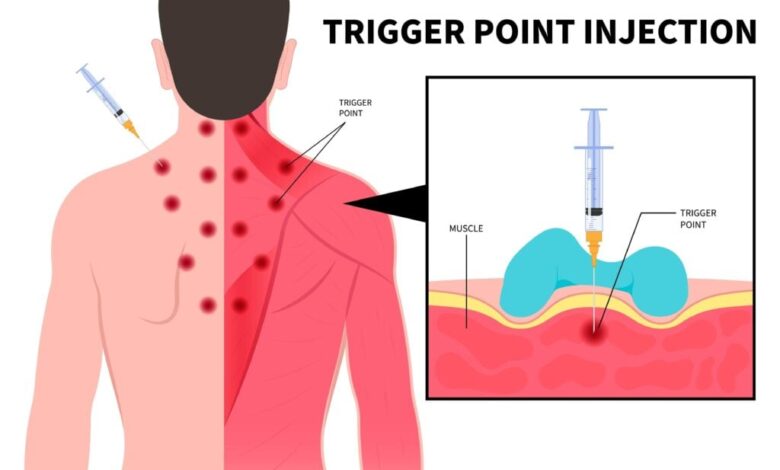
Trigger point injections (TPIs) are a relatively less common but potentially effective treatment option for migraines, particularly for those who haven’t found relief through other methods. This approach focuses on the muscles that may be contributing to the pain cycle of a migraine, providing targeted relief. Understanding the underlying mechanisms and the muscles involved is key to evaluating the suitability of TPIs.Trigger point injections work by targeting specific areas of muscle tension, known as trigger points, that may be contributing to migraine pain.
These trigger points are often hyperirritable spots within the muscle tissue, causing referred pain and potentially exacerbating the migraine cycle. By injecting these areas with local anesthetics and sometimes corticosteroids, the goal is to reduce inflammation, relax the muscle, and alleviate pain. This approach can be beneficial for those experiencing chronic or recurrent migraines.
Underlying Mechanisms of TPIs for Migraines
TPIs aim to address the potential role of musculoskeletal factors in migraine. The theory behind TPIs is that persistent muscle tension and trigger points in certain areas of the body can trigger or exacerbate migraine headaches. The injection of local anesthetics and corticosteroids directly into these trigger points is believed to reduce inflammation, promote muscle relaxation, and interrupt the pain signals being sent to the brain.
Trigger point injections for migraines can be a game-changer, but it’s crucial to remember that sometimes, seemingly healthy foods can be sneaky culprits. For instance, did you know that your healthy yogurt might be full of sugar? your healthy yogurt might be full of sugar This can definitely impact your overall health, potentially even triggering migraines.
While trigger point injections can be a helpful treatment, understanding the full picture of your diet and lifestyle is just as important for long-term migraine management.
This interruption of the pain cycle can potentially lead to decreased migraine frequency and intensity.
Muscles Commonly Associated with Migraine Triggers
Several muscle groups have been implicated in migraine triggers. The muscles of the neck, head, and upper back are frequently cited. The suboccipital muscles (at the base of the skull), trapezius muscles (upper back and neck), and temporalis muscles (sides of the head) are particularly relevant. These muscles can become tense due to stress, poor posture, or other factors, leading to trigger points.
Increased tension in these muscles can cause referred pain to other areas, potentially triggering or exacerbating a migraine. For example, tension in the suboccipital muscles can radiate pain to the head and neck, sometimes mimicking migraine symptoms.
Patient Experiences with TPIs
Patient experiences with TPIs for migraines are varied. Some individuals report significant pain relief and reduced migraine frequency after a course of injections. Others find only modest or temporary relief. Important factors influencing outcomes include the individual’s specific migraine triggers, the location and severity of trigger points, and the overall health condition. It’s crucial to consult with a healthcare professional to determine if TPIs are a suitable option.
Reviews and testimonials often highlight the need for multiple sessions to achieve optimal results, with ongoing management to maintain improvements.
Trigger point injections for migraines can be a game-changer, seriously! They’re a targeted approach to address those pesky pain points, but sometimes it’s the less obvious things that contribute to the headaches. For example, you might think you need to “eat for two” during pregnancy, but that’s actually a myth, as explained in this helpful guide on dont eat for two while pregnant.
While focusing on healthy eating habits is crucial, understanding the potential connection between diet and migraines can greatly impact the success of trigger point injections. Ultimately, finding the right treatment plan requires a holistic approach, considering all contributing factors.
Comparison of TPIs to Other Migraine Treatments
| Treatment Type | Mechanism | Advantages | Disadvantages | Cost |
|---|---|---|---|---|
| Trigger Point Injections (TPIs) | Targeting and relaxing muscle trigger points to reduce pain signals. | Potential for significant pain relief in some cases, particularly for those with musculoskeletal involvement. Can be effective for those resistant to other treatments. | Invasive procedure, potential for side effects (e.g., bruising, infection), not suitable for everyone, may not be effective for all individuals. | Variable, depending on the number of injections and location. |
| Medication (e.g., triptans, CGRP inhibitors) | Affecting neurochemical pathways involved in migraine pain. | Rapid relief from migraine pain, widely available. | Potential for side effects, may not be suitable for everyone. Some medications require prescription. | Variable, depending on the medication and dosage. |
| Non-invasive Therapies (e.g., massage, acupuncture) | Relaxing muscles, reducing stress, and influencing pain pathways. | Generally safe and non-invasive, can be incorporated into a broader management plan. | May not provide immediate or significant relief for acute migraines, may require multiple sessions for effectiveness. | Variable, depending on the therapy and provider. |
Procedure and Techniques
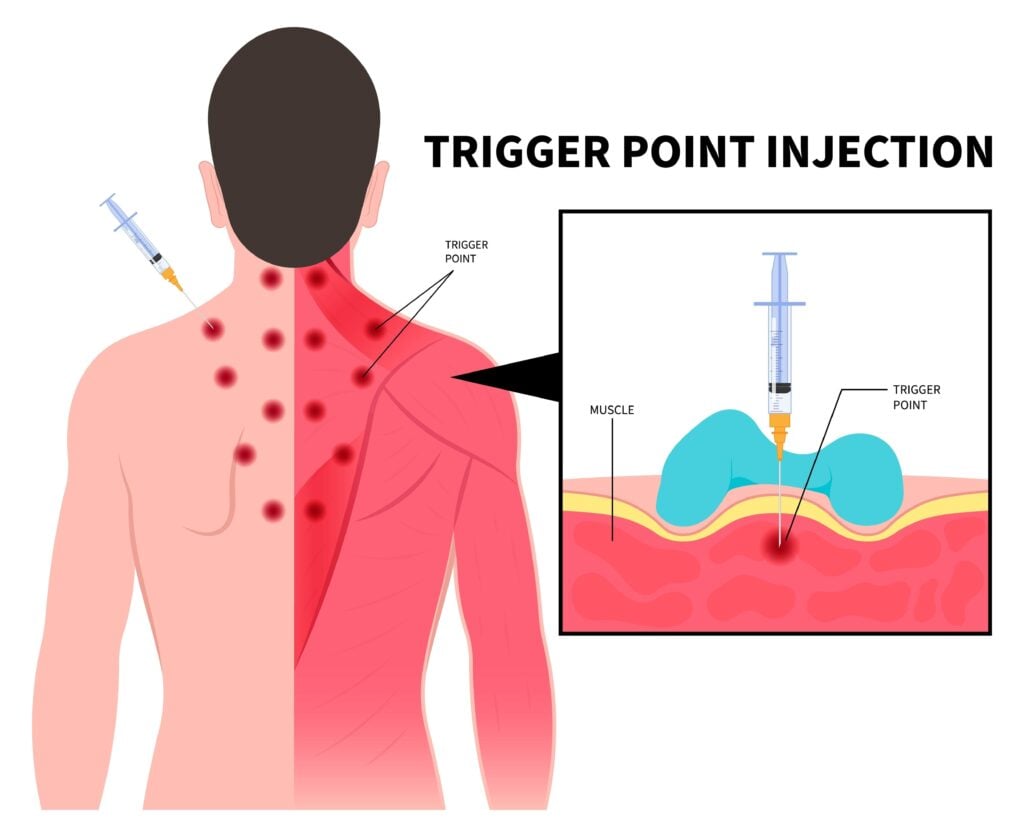
Trigger point injections (TPIs) for migraines offer a targeted approach to alleviate pain by directly addressing the underlying trigger points. This method involves injecting local anesthetic and sometimes steroids directly into these points, aiming to reduce inflammation and muscle tension. Understanding the procedure, identification techniques, and potential complications is crucial for successful treatment.
Procedure for Administering TPIs
The procedure for administering TPIs involves several key steps. First, a thorough patient assessment is critical to identify potential trigger points. Next, the clinician carefully locates the trigger points, often using palpation and diagnostic imaging if needed. The injection site is then cleaned and prepared. A local anesthetic is administered to numb the area, minimizing discomfort.
Finally, a precise injection of the medication is performed, aiming to deliver the medication directly into the trigger point.
Identifying and Targeting Trigger Points
Precise identification of trigger points is paramount for successful TPIs. This often involves palpation, where the clinician feels for taut bands or nodules in the muscles. The clinician may also use diagnostic imaging techniques like ultrasound or electromyography to further pinpoint the location and characteristics of the trigger points. Careful consideration of the patient’s reported pain patterns and neurological examination findings can further refine the targeting process.
Preparing the Patient for the Procedure
Thorough preparation of the patient is essential for a positive experience. This includes providing clear and comprehensive information about the procedure, including potential benefits, risks, and expected sensations. Explaining the steps involved and answering any questions can help alleviate anxiety. Ensuring the patient is comfortable and relaxed before the procedure will also contribute to a better outcome.
The patient should be informed about the signs of any adverse reactions and instructed on when to report them. Educating the patient on post-procedure care is also crucial.
Injection Techniques
Different injection techniques are used in TPIs, each with its own advantages and disadvantages. One common technique involves using a very fine needle and injecting the medication directly into the trigger point. Another method involves injecting the medication into the surrounding tissues, aiming to reduce the surrounding inflammation. The choice of technique often depends on the location and size of the trigger point, as well as the clinician’s experience and preference.
Potential Complications and Side Effects
TPIs, like any medical procedure, carry potential complications. It’s important for both patients and clinicians to understand these possibilities.
| Potential Complication | Description | Frequency | Management |
|---|---|---|---|
| Pain at injection site | Transient discomfort at the injection site. | Common | Over-the-counter pain relievers may be sufficient. |
| Bleeding or bruising | Localized bleeding or bruising at the injection site. | Occasional | Ice packs and elevation can help reduce these symptoms. |
| Infection | Risk of localized infection at the injection site. | Rare | Prompt treatment with antibiotics if infection develops. |
| Nerve damage | Rarely, injections may cause damage to nearby nerves. | Rare | Careful injection technique and appropriate imaging can help minimize this risk. |
| Systemic allergic reaction | Rarely, an allergic reaction to the medication may occur. | Very rare | Immediate treatment with epinephrine and supportive measures. |
Efficacy and Outcomes: Trigger Point Injections For Migraines
Trigger point injections (TPIs) for migraines offer a potential alternative or adjunct therapy for those experiencing chronic or treatment-resistant migraines. Understanding the current research, comparative outcomes, and integration into a comprehensive management plan is crucial for informed decision-making. This section explores the efficacy and potential benefits of TPIs, along with their limitations.TPIs for migraines are not a universally effective solution, and their success hinges on precise identification of trigger points and careful injection technique.
Individual responses vary significantly, and the long-term effects require further investigation. A comprehensive approach that combines TPIs with other therapies, such as lifestyle modifications and medication, is often necessary for optimal management.
Current Research on Effectiveness
The research on the effectiveness of TPIs for migraines is ongoing, with some studies suggesting potential benefits, while others report limited or no significant improvement. A crucial aspect is the variability in study methodologies, sample sizes, and diagnostic criteria, which can impact the reliability of the findings.
Published Studies
Several studies have investigated the impact of TPIs on migraine frequency and severity. Unfortunately, a definitive consensus regarding efficacy has yet to emerge. The lack of standardized protocols and consistent methodologies makes direct comparisons challenging. A review of relevant studies is necessary to understand the varied outcomes. Further research is needed to clarify the role of TPIs in different migraine subtypes and individual patient responses.
Comparison with Other Migraine Treatments, Trigger point injections for migraines
TPIs can be considered a complementary approach to existing migraine treatments, such as medication, lifestyle modifications, and alternative therapies. Comparison of outcomes depends heavily on the specific treatment protocols and individual patient responses. While some studies indicate that TPIs might reduce migraine frequency and intensity, the impact compared to other treatments remains unclear.
Integration into a Comprehensive Migraine Management Plan
TPIs should not be considered a standalone treatment but rather a potential component of a comprehensive migraine management plan. This plan should encompass lifestyle adjustments (sleep hygiene, stress management, diet), medication optimization, and alternative therapies (biofeedback, acupuncture). A multidisciplinary approach, including consultation with neurologists, pain specialists, and other healthcare providers, is crucial for tailoring a personalized management strategy.
Success Rates by Migraine Subtype
| Migraine Subtype | Success Rate of TPIs | Comparison with Other Treatments |
|---|---|---|
| Tension-type headaches | Variable results, ranging from moderate to low. | May be less effective than specific therapies for tension-type headaches. |
| Migraine with aura | Limited evidence; results vary across studies. | Comparable to other treatments but with potential variability in response. |
| Chronic migraine | Potentially beneficial in reducing frequency and intensity. | Results may be similar to other chronic migraine therapies, but with individual variability. |
| Episodic migraine | Some studies show potential for reduced migraine frequency. | Effectiveness may be comparable to preventive medications, depending on the individual. |
Note: The success rates presented in the table are generalized and represent a complex picture of the existing literature. Further research is required to ascertain the specific effectiveness for each migraine subtype.
Trigger point injections for migraines can be a real game-changer, but sometimes, like rinsing that apple off with water might not be good enough, a deeper dive into underlying causes is needed. Addressing potential food sensitivities or environmental triggers could significantly improve outcomes alongside the injections. This deeper approach often leads to more lasting relief from migraine symptoms.
For more on the importance of considering the whole picture when it comes to health, check out this insightful article on rinsing that apple off with water might not be good enough. Ultimately, understanding the complexities of migraine treatment can lead to better results with trigger point injections.
Patient Selection and Considerations
Trigger point injections (TPIs) for migraines offer a potential therapeutic approach, but careful patient selection is crucial for maximizing efficacy and minimizing risks. Properly identifying suitable candidates and understanding contraindications are essential for ensuring the procedure’s success and patient safety. This section delves into the criteria for selecting appropriate patients, highlighting factors to consider, and emphasizing the importance of pre-procedure education.Thorough evaluation is paramount to determining if a patient will benefit from TPIs.
This involves understanding the patient’s specific migraine characteristics, underlying medical conditions, and potential risks associated with the procedure. Ultimately, the goal is to ensure that the intervention is safe, effective, and aligned with the patient’s overall health goals.
Criteria for Selecting Suitable Patients
Careful evaluation of a patient’s medical history and migraine characteristics is critical. Patients with chronic migraine, particularly those experiencing significant functional impairment, might be ideal candidates for TPIs. The presence of well-defined, tender trigger points, consistently linked to migraine attacks, is another important indicator. Furthermore, a patient’s willingness to adhere to post-procedure recommendations and actively participate in their care is vital.
Understanding their expectations and ensuring realistic outcomes are crucial for managing their expectations.
Contraindications for TPIs
Certain conditions can preclude TPIs. Active infections, bleeding disorders, or coagulopathies increase the risk of complications. Patients with known hypersensitivity to the local anesthetic or steroid components used in the procedure should be excluded. Moreover, pregnancy and breastfeeding periods, especially during the first trimester, are often contraindicated due to potential risks to the developing fetus. Pre-existing neurological conditions, especially those with a history of stroke or seizures, necessitate cautious consideration.
Additionally, a history of significant skin infections at the injection site may also be a contraindication.
Factors to Consider in Patient Selection
Several factors should be evaluated to determine if a patient is a good candidate for TPIs. These include:
- Migraine frequency and severity: Patients experiencing frequent and severe migraine attacks may benefit more from TPIs. Examples include individuals with a documented history of 15 or more migraine days per month, or experiencing significant impairment in daily activities due to migraine.
- Presence and location of trigger points: Identifying specific, tender trigger points is crucial. Their consistent correlation with migraine attacks suggests a potential for TPI success. For example, if a patient regularly experiences migraines after clenching their jaw, trigger points in the temporomandibular joint area could be targeted.
- Patient motivation and compliance: Patients must be motivated and willing to adhere to post-procedure recommendations, such as avoiding strenuous activity or maintaining a healthy lifestyle.
- Overall health status: Pre-existing medical conditions, such as bleeding disorders, infections, or neurological conditions, can affect the suitability of TPIs.
Importance of Patient Education and Counseling
Thorough patient education and counseling are essential before undergoing TPIs. This involves explaining the procedure, potential benefits, risks, and alternative treatment options. Patients should understand the limitations of TPIs and that they are not a one-size-fits-all solution. Open communication about expectations, including the possibility of limited relief or the need for additional treatments, is crucial. Realistic expectations should be established.
This preparation empowers patients to make informed decisions.
Summary Table of TPIs for Various Patient Demographics
| Patient Demographic | Benefits | Drawbacks | Considerations |
|---|---|---|---|
| Chronic migraine sufferers with well-defined trigger points | Potentially significant pain relief | Potential for limited or temporary relief | Careful evaluation of trigger point location and consistency |
| Patients with episodic migraine and identifiable trigger points | Potential for reducing migraine frequency and severity | Risk of injection site reactions | Patient’s willingness to undergo multiple injections |
| Patients with comorbidities (e.g., anxiety, depression) | Potential for reducing migraine-related disability | Potential for interactions with other medications | Careful consideration of patient’s overall health and potential interactions |
| Older adults | Potential for improving quality of life | Increased risk of complications due to age-related factors | Close monitoring for adverse effects and individual tailoring of treatment plan |
Potential Benefits and Risks
Trigger point injections (TPIs) for migraines offer a potential pathway to pain relief, but like any medical procedure, they come with inherent risks. Understanding both the advantages and disadvantages is crucial for informed decision-making. This section delves into the potential benefits and risks of TPIs, considering long-term outcomes and patient experiences.
Potential Benefits of TPIs for Migraine Management
TPIs aim to alleviate migraine pain by targeting and treating specific trigger points. These points, often in the neck and shoulder muscles, are believed to contribute to migraine episodes through referred pain and muscle tension. Successful TPIs can result in a reduction in the frequency, intensity, and duration of migraine attacks, leading to improved quality of life. Patients may experience a decrease in overall pain levels and an increase in their ability to perform daily activities without being hampered by migraine pain.
Potential Risks and Complications of TPIs
While TPIs can be beneficial, potential complications and side effects exist. These can range from minor discomfort to more serious adverse events. Needle insertion can sometimes cause localized pain, bruising, or swelling. In some cases, bleeding, infection, or nerve damage may occur, though these are less common. Rarely, allergic reactions to the injected medication can manifest.
Careful patient selection and meticulous injection technique are crucial to minimizing these risks.
Long-Term Outcomes and Recurrence Potential
The long-term efficacy of TPIs for migraine management varies among patients. Some individuals experience sustained relief, with a significant reduction in migraine frequency and severity. However, others may experience a temporary or partial response, or the pain may return over time. Factors such as the underlying cause of the migraines, the patient’s individual response to treatment, and the adherence to lifestyle recommendations play a role in the long-term outcome.
Patient Testimonials and Experiences
Numerous patients have reported positive experiences with TPIs. For example, one patient reported a significant reduction in migraine frequency after a series of injections. Another patient described experiencing relief from debilitating neck pain, which was a significant trigger for their migraines. These anecdotal accounts highlight the potential for TPIs to provide relief, but it’s crucial to remember that individual responses can vary.
Table of Potential Risks and Benefits of TPIs
| Risk | Description | Likelihood | Mitigation Strategies |
|---|---|---|---|
| Local Pain | Discomfort at the injection site. | High | Local anesthetic, proper injection technique. |
| Bruising | Localized discoloration due to bleeding. | Moderate | Applying ice packs, elevation of the affected area. |
| Infection | Bacterial or fungal infection at the injection site. | Low | Strict aseptic technique during injection, antibiotic prophylaxis. |
| Nerve Damage | Injury to nerves in the treated area. | Very Low | Proper injection technique, careful needle placement, monitoring. |
| Allergic Reaction | Adverse reaction to the medication. | Low | Pre-injection allergy testing, careful monitoring, emergency preparedness. |
| Bleeding | Excessive bleeding at the injection site. | Low | Proper injection technique, monitoring for excessive bleeding. |
| Recurrence | Pain returning after initial improvement. | Variable | Adherence to follow-up care, lifestyle modifications, addressing underlying causes. |
Alternatives and Complementary Approaches
Trigger point injections (TPIs) for migraines can be a helpful treatment, but they aren’t always the sole solution. Often, the most effective approach involves combining TPIs with other strategies to address the multifaceted nature of migraine. This section explores alternative and complementary therapies, emphasizing their potential synergy with TPIs and lifestyle modifications to manage migraine triggers.Understanding that migraines are influenced by a complex interplay of factors, including stress, diet, and sleep, it is essential to consider a holistic approach to management.
Combining TPIs with complementary therapies can offer a more comprehensive and potentially more effective strategy for migraine relief.
Alternative Therapies to Complement TPI Treatment
Integrating alternative therapies can enhance the benefits of TPIs by addressing the underlying causes and triggers of migraines. These therapies can work synergistically with TPIs to provide a more comprehensive approach to migraine management.
- Acupuncture: This ancient Chinese technique involves inserting thin needles into specific points on the body. Some studies suggest that acupuncture can reduce migraine frequency and intensity. Its mechanism of action likely involves modulating pain pathways and influencing neurotransmitters.
- Biofeedback: This technique teaches individuals to recognize and control physiological responses, such as muscle tension and heart rate, which can be linked to migraine triggers. By learning to manage these responses, individuals can potentially reduce migraine episodes.
- Massage Therapy: Manual manipulation of soft tissues, such as muscles and connective tissues, can help alleviate tension and trigger points, potentially reducing migraine frequency. Massage therapy can be particularly helpful in conjunction with TPIs for localized pain relief.
- Yoga and Meditation: These practices promote relaxation and stress reduction, which are crucial for managing migraine triggers. Regular yoga and meditation can help individuals develop coping mechanisms for managing stress and tension headaches.
- Dietary Modifications: Certain foods and drinks can trigger migraines in susceptible individuals. Identifying and avoiding these triggers can significantly reduce migraine frequency. Examples include aged cheeses, processed meats, and caffeine.
Potential Interactions and Benefits of Combining TPIs with Other Therapies
Careful consideration of potential interactions and synergistic effects is crucial when combining TPIs with alternative therapies.
| Therapy Type | Description | Potential Interaction with TPIs | Benefits |
|---|---|---|---|
| Acupuncture | Inserting thin needles into specific body points | Potentially complementary; both aim to modulate pain pathways. No known direct interactions. | May reduce migraine frequency and intensity. Can address stress and tension, which are often linked to migraines. |
| Biofeedback | Learning to control physiological responses | Potentially synergistic; helps manage triggers and stress. No known direct interactions. | Reduces stress, tension, and may help identify migraine triggers. |
| Massage Therapy | Manual manipulation of soft tissues | Potentially complementary; addresses tension and trigger points. Massage can enhance TPI effects by relaxing surrounding muscles. | Reduces localized pain and muscle tension, potentially increasing TPI efficacy. |
| Yoga/Meditation | Stress reduction and relaxation techniques | Potentially synergistic; addresses stress and anxiety. No known direct interactions. | Reduces stress, improves relaxation response, which can help manage migraine triggers. |
| Dietary Modifications | Avoiding migraine triggers (e.g., caffeine, aged cheese) | Potentially synergistic; avoids potential triggers. No known direct interactions. | Reduces migraine frequency and severity by eliminating trigger foods. |
Future Directions and Research
Trigger point injections (TPIs) for migraines show promise, but further research is crucial to refine their application and maximize their effectiveness. Understanding the complex interplay of trigger points, neurological pathways, and individual patient responses is vital for optimizing treatment outcomes. This section explores promising avenues for future research, focusing on improving TPI techniques, evaluating long-term effects, and expanding our knowledge of the underlying mechanisms.
Areas Requiring Further Research
The efficacy of TPIs for migraines is not uniformly demonstrated across all patient populations. Variability in patient responses, the exact mechanisms through which TPIs alleviate migraine pain, and the long-term consequences of these procedures need further exploration. This requires a deeper dive into the biological processes involved and a more personalized approach to patient selection and treatment protocols.
Potential Advancements in TPI Techniques
Technological advancements offer exciting possibilities for improving TPI procedures. Real-time imaging, such as ultrasound or MRI guidance, can enhance precision and minimize invasiveness. These techniques allow for more accurate targeting of trigger points, potentially reducing discomfort and increasing treatment efficacy. Furthermore, the development of novel injection techniques, such as targeted drug delivery systems, may optimize drug distribution and prolong the analgesic effect.
Minimally invasive procedures, like the use of smaller needles and precise injection methods, will reduce patient discomfort and improve safety profiles.
Emerging Research Topics in TPI for Migraines
Emerging research areas in TPIs for migraines encompass a variety of factors. One significant area of investigation involves understanding the relationship between trigger point activity, the central nervous system, and the development of migraine attacks. Further investigation into the role of specific neurotransmitters and inflammatory markers in migraine pathophysiology will provide a clearer picture of the underlying mechanisms.
The impact of TPI on the long-term management of migraine, including its effects on medication usage and overall quality of life, is also a key area for research.
Unanswered Questions in TPI Research
Numerous unanswered questions remain regarding the optimal selection of patients who will benefit most from TPIs. Determining the optimal frequency and duration of TPI treatments to maximize efficacy and minimize side effects is crucial. Further investigation into the potential long-term complications of TPIs is also warranted.
Future Research Avenues: Long-Term Effects
Investigating the long-term effects of TPIs for migraines is paramount. A longitudinal study design following patients over several years is essential to evaluate the lasting impact on migraine frequency, severity, and associated disability. The study should track changes in medication usage, pain management strategies, and overall well-being.
- Evaluating the impact of TPIs on the need for prophylactic medications.
- Assessing the long-term effects on the quality of life, including social and occupational functioning.
- Determining the potential for trigger point recurrence after TPI treatment and developing strategies for prevention.
- Comparing the effectiveness of TPIs with other treatment modalities for migraines.
Final Summary
Trigger point injections for migraines represent a complex treatment option with potential benefits and risks. This in-depth exploration of TPIs provides a well-rounded understanding of the procedure, its efficacy, and the considerations involved in patient selection. By comparing TPIs to other migraine treatments and highlighting potential complications, we equip you with the knowledge to make informed decisions. Remember, consulting with a healthcare professional is crucial for personalized guidance.
